Korean J Gastroenterol.
2014 Dec;64(6):348-355. 10.4166/kjg.2014.64.6.348.
Differences in the Adverse Effects of Azathioprine between Inflammatory Bowel Disease and Autoimmune Hepatitis in Korean Patients
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea. seenae99@dsmc.or.kr
- KMID: 2160667
- DOI: http://doi.org/10.4166/kjg.2014.64.6.348
Abstract
- BACKGROUND/AIMS
Azathioprine (AZA) has been widely used in the therapy of inflammatory bowel disease (IBD) and autoimmune hepatitis (AIH). However, studies evaluating the adverse effects of AZA in these two diseases are lacking. The aim of this study was to compare the adverse effects of AZA in Korean IBD and AIH patients.
METHODS
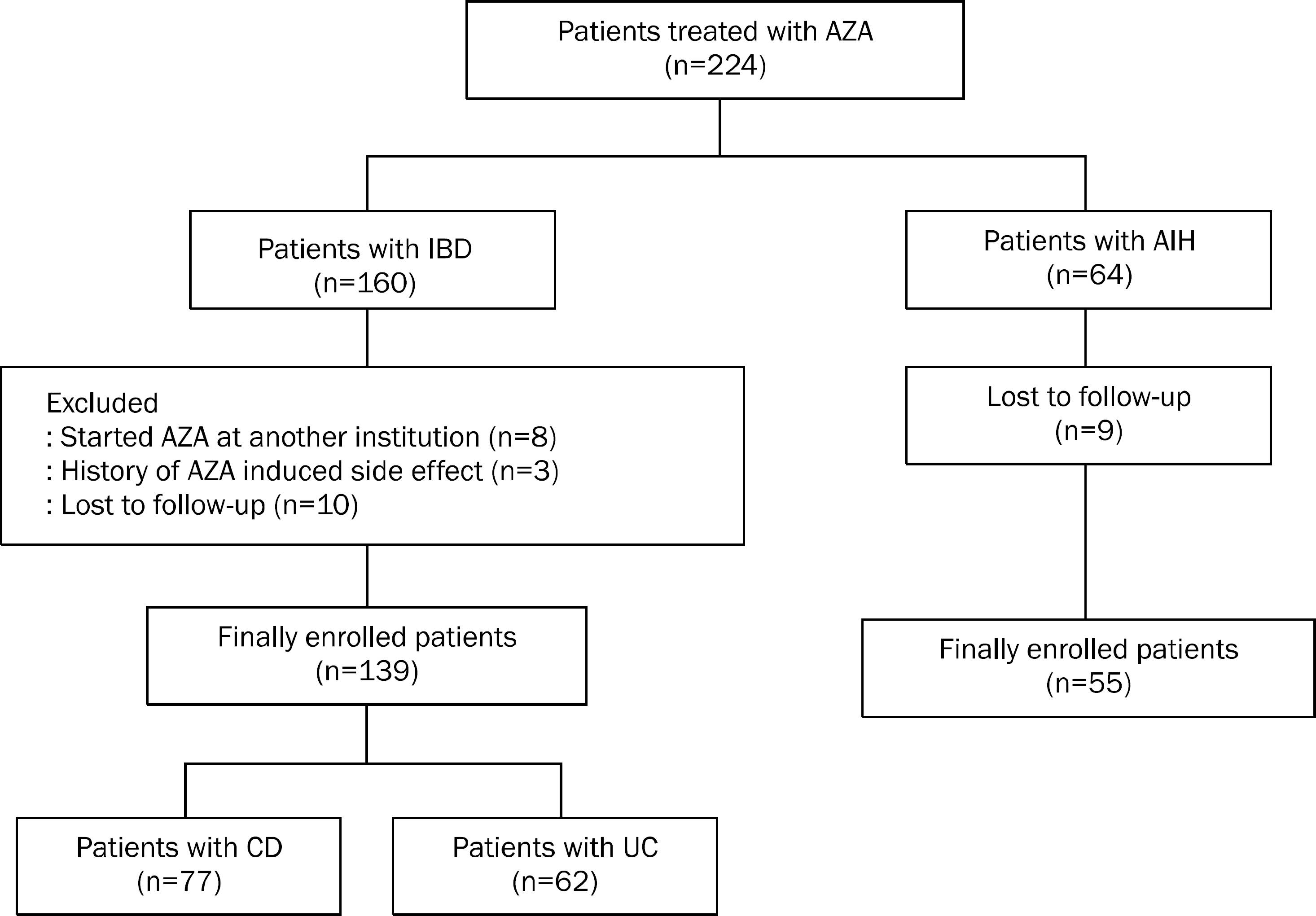
Patients with IBD or AIH who were treated with AZA at Keimyung University Dongsan Medical Center (Daegu, Korea) between January 2002 and March 2011 were enrolled. Their medical records were reviewed retrospectively in terms of clinical characteristics and adverse effects of AZA.
RESULTS
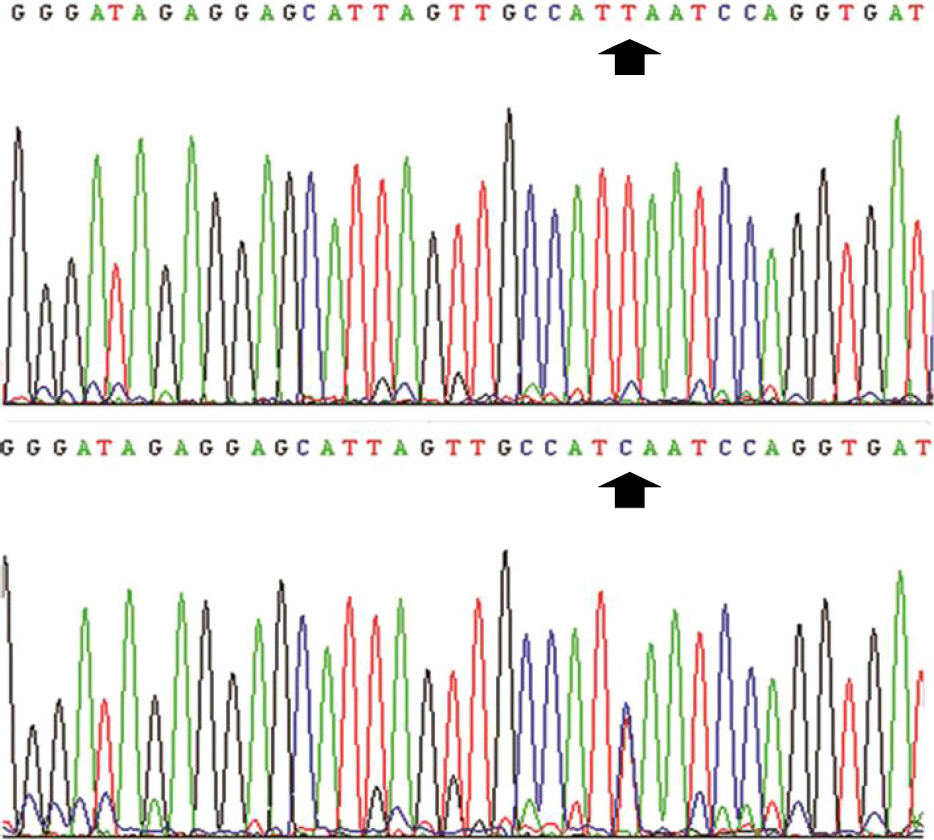
A total of 139 IBD patients and 55 AIH patients were finally enrolled. Thirty IBD patients (21.6%) and eight AIH patients (14.5%) experienced adverse effects of AZA. In particular, the prevalence of leukopenia was significantly higher in the IBD group than in the AIH group (p=0.026). T474C mutation was observed in three of 10 patients who were assessed for thiopurine methyltransferase (TPMT) genotype.
CONCLUSIONS
IBD patients are at increased risk for the adverse effects of AZA compared with AIH patients, of which leukopenia was the most commonly observed. Therefore, IBD patients receiving AZA therapy should be carefully monitored.
MeSH Terms
-
Adolescent
Adult
Aged
Azathioprine/adverse effects/*therapeutic use
Base Sequence
Female
Genotype
Hepatitis, Autoimmune/*drug therapy
Humans
Immunosuppressive Agents/adverse effects/*therapeutic use
Inflammatory Bowel Diseases/*drug therapy
Leukopenia/epidemiology/etiology
Male
Methyltransferases/chemistry/genetics
Middle Aged
Polymorphism, Single Nucleotide
Republic of Korea
Retrospective Studies
Young Adult
Azathioprine
Immunosuppressive Agents
Methyltransferases
Figure
Reference
-
References
1. Kim ES, Kim WH. Inflammatory bowel disease in Korea: epi-demiological, genomic, clinical, and therapeutic characteristics. Gut Liver. 2010; 4:1–14.
Article2. Liberal R, Grant CR, Longhi MS, Mieli-Vergani G, Vergani D. Diagnostic criteria of autoimmune hepatitis. Autoimmun Rev. 2014; 13:435–440.
Article3. Bajaj JS, Saeian K, Varma RR, et al. Increased rates of early adverse reaction to azathioprine in patients with Crohn's disease compared to autoimmune hepatitis: a tertiary referral center experience. Am J Gastroenterol. 2005; 100:1121–1125.
Article4. Fraser AG, Orchard TR, Jewell DP. The efficacy of azathioprine for the treatment of inflammatory bowel disease: a 30 year review. Gut. 2002; 50:485–489.
Article5. Manns MP, Czaja AJ, Gorham JD, et al. American Association for the Study of Liver Diseases. Diagnosis and management of autoimmune hepatitis. Hepatology. 2010; 51:2193–2213.
Article6. Connell WR, Kamm MA, Ritchie JK, Lennard-Jones JE. Bone marrow toxicity caused by azathioprine in inflammatory bowel disease: 27 years of experience. Gut. 1993; 34:1081–1085.
Article7. Chun JY, Kang B, Lee YM, Lee SY, Kim MJ, Choe YH. Adverse events associated with azathioprine treatment in korean pediatric inflammatory bowel disease patients. Pediatr Gastroenterol Hepatol Nutr. 2013; 16:171–177.
Article8. de Jong DJ, Goullet M, Naber TH. Side effects of azathioprine in patients with Crohn's disease. Eur J Gastroenterol Hepatol. 2004; 16:207–212.
Article9. Gisbert JP, Niño P, Rodrigo L, Cara C, Guijarro LG. Thiopurine methyltransferase (TPMT) activity and adverse effects of azathioprine in inflammatory bowel disease: long-term follow-up study of 394 patients. Am J Gastroenterol. 2006; 101:2769–2776.
Article10. Kim JH, Cheon JH, Kim WH. The frequency and the course of the adverse effects of azathioprine/6-mercaptopurine treatment in patients with inflammatory bowel disease. Korean J Gastroenterol. 2008; 51:291–297.11. Saibeni S, Virgilio T, D'Incà R, et al. The use of thiopurines for the treatment of inflammatory bowel diseases in clinical practice. Dig Liver Dis. 2008; 40:814–820.
Article12. Bastida G, Nos P, Aguas M, et al. Incidence, risk factors and clinical course of thiopurine-induced liver injury in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2005; 22:775–782.
Article13. Ben Ari Z, Mehta A, Lennard L, Burroughs AK. Azathioprine-in-duced myelosuppression due to thiopurine methyltransferase deficiency in a patient with autoimmune hepatitis. J Hepatol. 1995; 23:351–354.14. Czaja AJ. Drug therapy in the management of type 1 autoimmune hepatitis. Drugs. 1999; 57:49–68.
Article15. George J, Present DH, Pou R, Bodian C, Rubin PH. The long-term outcome of ulcerative colitis treated with 6-mercaptopurine. Am J Gastroenterol. 1996; 91:1711–1714.16. Sandborn WJ, Tremaine WJ, Wolf DC, et al. Lack of effect of intra-venous administration on time to respond to azathioprine for steroid-treated Crohn's disease. North American Azathioprine Study Group. Gastroenterology. 1999; 117:527–535.17. Present DH, Meltzer SJ, Krumholz MP, Wolke A, Korelitz BI. 6-Mercaptopurine in the management of inflammatory bowel disease: short- and long-term toxicity. Ann Intern Med. 1989; 111:641–649.
Article18. Kim JH, Cheon JH, Hong SS, et al. Influences of thiopurine methyltransferase genotype and activity on thiopurine-induced leukopenia in Korean patients with inflammatory bowel disease: a retrospective cohort study. J Clin Gastroenterol. 2010; 44:e242–e248.19. Kim DU, Kim YH, Kim BJ, et al. The efficacy of low dose azathioprine/6-mercaptopurine in patients with inflammatory bowel disease. Hepatogastroenterology. 2009; 56:1395–1402.20. Jun JB, Cho DY, Kang C, Bae SC. Thiopurine S-methyltransferase polymorphisms and the relationship between the mutant alleles and the adverse effects in systemic lupus erythematosus patients taking azathioprine. Clin Exp Rheumatol. 2005; 23:873–876.21. Jung YS, Cheon JH, Park JJ, et al. Correlation of genotypes for thiopurine methyltransferase and inosine triphosphate py-rophosphatase with long-term clinical outcomes in Korean patients with inflammatory bowel diseases during treatment with thiopurine drugs. J Hum Genet. 2010; 55:121–123.
Article22. Venkat Raman G, Sharman VL, Lee HA. Azathioprine and allo-purinol: a potentially dangerous combination. J Intern Med. 1990; 228:69–71.23. Szumlanski CL, Weinshilboum RM. Sulphasalazine inhibition of thiopurine methyltransferase: possible mechanism for inter-action with 6-mercaptopurine and azathioprine. Br J Clin Pharmacol. 1995; 39:456–459.
Article24. Korelitz BI. Steroids may prevent leukopenia, interfering with response to IV azathioprine in treatment of Crohn's disease. Gastroenterology. 2000; 118:1281–1282.25. Dubinsky MC. Azathioprine, 6-mercaptopurine in inflammatory bowel disease: pharmacology, efficacy, and safety. Clin Gastroenterol Hepatol. 2004; 2:731–743.
Article26. Black AJ, McLeod HL, Capell HA, et al. Thiopurine methyltransferase genotype predicts therapy-limiting severe toxicity from azathioprine. Ann Intern Med. 1998; 129:716–718.
Article27. Heneghan MA, Allan ML, Bornstein JD, Muir AJ, Tendler DA. Utility of thiopurine methyltransferase genotyping and phenotyping, and measurement of azathioprine metabolites in the management of patients with autoimmune hepatitis. J Hepatol. 2006; 45:584–591.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Monitoring and Safety of Azathioprine Therapy in Inflammatory Bowel Disease
- The Frequency and the Course of the Adverse Effects of Azathioprine/6-Mercaptopurine Treatment in Patients with Inflammatory Bowel Disease
- Polymyositis Associated with Autoimmune Hepatitis
- Azathioprine-Induced Non-Cirrhotic Portal Hypertension in a Patient with Crohn’s Disease
- The Frequency and the Course of the Adverse Effects of Azathioprine/6-Mercaptopurine Treatment in Patients with Inflammatory Bowel Disease