Yonsei Med J.
2013 Jul;54(4):949-956. 10.3349/ymj.2013.54.4.949.
Tracheal Wall Thickening Is Associated with the Granulation Tissue Formation Around Silicone Stents in Patients with Post-Tuberculosis Tracheal Stenosis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hjk3425@skku.edu
- KMID: 2158231
- DOI: http://doi.org/10.3349/ymj.2013.54.4.949
Abstract
- PURPOSE
Tracheal restenosis due to excessive granulation tissue around a silicone stent requires repeated bronchoscopic interventions in patients with post-tuberculosis tracheal stenosis (PTTS). The current study was conducted to identify the risk factors for granulation tissue formation after silicone stenting in PTTS patients.
MATERIALS AND METHODS
A retrospective study was conducted between January 1998 and December 2010. Forty-two PTTS patients with silicone stenting were selected. Clinical and radiological variables were retrospectively collected and analyzed.
RESULTS
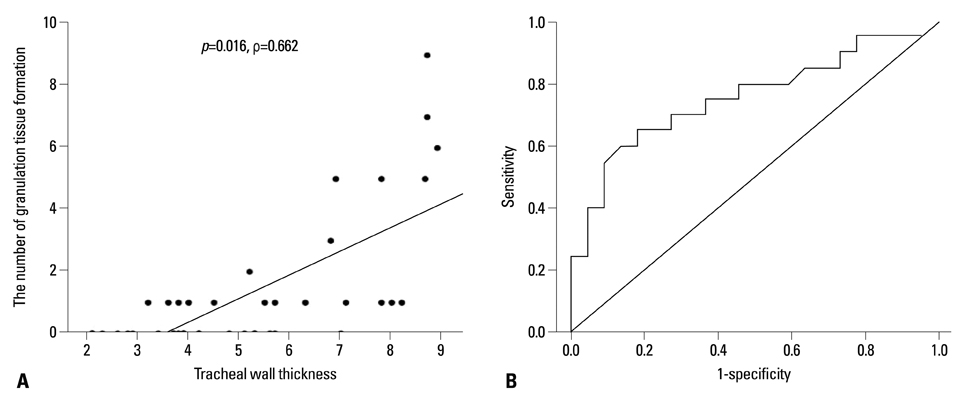
Tracheal restenosis due to granulation tissue formation were found in 20 patients (47.6%), and repeated bronchoscopic interventions were conducted. In multivariate analysis, tracheal wall thickness, measured on axial computed tomography scan, was independently associated with granulation tissue formation after silicone stenting. Furthermore, the degree of tracheal wall thickness was well correlated with the degree of granulation tissue formation.
CONCLUSION
Tracheal wall thickening was associated with granulation tissue formation around silicone stents in patients with post-tuberculosis tracheal stenosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Um SW, Yoon YS, Lee SM, Yim JJ, Yoo CG, Chung HS, et al. Predictors of persistent airway stenosis in patients with endobronchial tuberculosis. Int J Tuberc Lung Dis. 2008; 12:57–62.2. Chung HS, Lee JH. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest. 2000; 117:385–392.
Article3. Rikimaru T. Endobronchial tuberculosis. Expert Rev Anti Infect Ther. 2004; 2:245–251.
Article4. Shim YS. Endobronchial tuberculosis. Respirology. 1996; 1:95–106.
Article5. Kim H. Stenting therapy for stenosing airway disease. Respirology. 1998; 3:221–228.
Article6. Wan IY, Lee TW, Lam HC, Abdullah V, Yim AP. Tracheobronchial stenting for tuberculous airway stenosis. Chest. 2002; 122:370–374.
Article7. Hu HC, Liu YH, Wu YC, Hsieh MJ, Chao YK, Wu CY, et al. Granulation tissue formation following Dumon airway stenting: the influence of stent diameter. Thorac Cardiovasc Surg. 2011; 59:163–168.
Article8. Schmäl F, Fegeler W, Terpe HJ, Hermann W, Stoll W, Becker K. Bacteria and granulation tissue associated with Montgomery T-tubes. Laryngoscope. 2003; 113:1394–1400.
Article9. Lee JY, Yi CA, Kim TS, Kim H, Kim J, Han J, et al. CT scan features as predictors of patient outcome after bronchial intervention in endobronchial TB. Chest. 2010; 138:380–385.
Article10. Colt HG, Dumon JF. Airway stents. Present and future. Clin Chest Med. 1995; 16:465–478.11. Nouraei SA, Petrou MA, Randhawa PS, Singh A, Howard DJ, Sandhu GS. Bacterial colonization of airway stents: a promoter of granulation tissue formation following laryngotracheal reconstruction. Arch Otolaryngol Head Neck Surg. 2006; 132:1086–1090.12. Zhang J, Wang T, Wang J, Pei YH, Xu M, Wang YL, et al. Effect of three interventional bronchoscopic methods on tracheal stenosis and the formation of granulation tissues in dogs. Chin Med J (Engl). 2010; 123:621–627.13. Webb EM, Elicker BM, Webb WR. Using CT to diagnose nonneoplastic tracheal abnormalities: appearance of the tracheal wall. AJR Am J Roentgenol. 2000; 174:1315–1321.14. Prince JS, Duhamel DR, Levin DL, Harrell JH, Friedman PJ. Nonneoplastic lesions of the tracheobronchial wall: radiologic findings with bronchoscopic correlation. Radiographics. 2002; 22 Spec No:S215–S230.
Article15. Brown JJ, Bayat A. Genetic susceptibility to raised dermal scarring. Br J Dermatol. 2009; 161:8–18.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experience of Silicone Airway Stent in the Management of Benign Tracheobronchial Stenosis
- Clinical Experience of Rigid Bronchoscopy in Single Center
- Airway obstruction due to post intubation circumferential tracheal web formation: A case report
- Airway Expandible Metallic Stent Implantation in Children with Tracheal or Bronchial Stenosis
- A Case Report of Primary Tracheal Tuberculosis with Asthma-like Symptoms