J Korean Med Sci.
2012 Dec;27(12):1541-1546. 10.3346/jkms.2012.27.12.1541.
Coagulopathy as a Prognostic Factor of Acute Lung Injury in Children
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. jdparkmd@snu.ac.kr
- KMID: 2157979
- DOI: http://doi.org/10.3346/jkms.2012.27.12.1541
Abstract
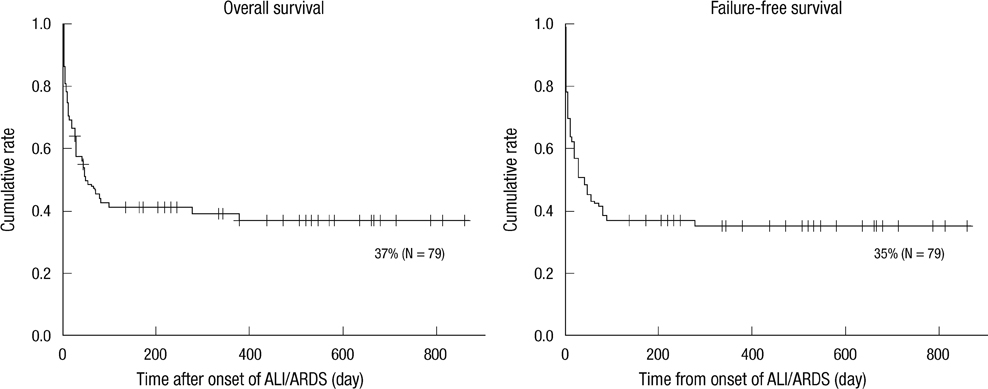
- The coagulation cascade and inflammatory process are known to be associated with the pathophysiology of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). We retrospectively investigated laboratory values indicating coagulopathy obtained within 24 hr from diagnosis of ALI/ARDS in 79 children who received mechanical ventilation between 2008 and 2009 and their final outcomes. Prothrombin time (PT) (P = 0.001) and activated partial thromboplastin time PTT (APTT) (P = 0.001) were more prolonged in non-survivors than survivors (mean; 1.57 vs 1.33; 63 vs 57). In multivariate analysis with stratification by oxygenation-index (< 14.5, > or = 14.5), prolonged PT (> or = 1.46 international normalized ratio, [INR]) (hazard ratio; 2.043, 1.027-4.064) was associated with lower non-pulmonary-organ-failure-free survival rate (FFS), and prolonged APTT (> or = 50 seconds) (2.062, 1.031-4.121; 2.422, 1.227-4.781) was associated with lower overall survival rate (OS) and lower FFS. In stratification by ventilation-index (< 40, > or = 40), prolonged PT (2.232, 1.095-4.540; 2.177, 1.092-4.342) and prolonged APTT (2.574, 1.230-5.386; 3.089, 1.500-6.360) were associated with lower OS and lower FFS. Prolonged PT and APTT are associated with mortality in mechanically ventilated children with ALI/ARDS. We suggest PT and APTT as prognostic factors of ALI/ARDS in children.
Keyword
MeSH Terms
-
Acute Lung Injury/*etiology/mortality
Adolescent
Blood Coagulation Disorders/*complications
Child
Child, Preschool
Female
Humans
Infant
Infant, Newborn
Male
Multivariate Analysis
Partial Thromboplastin Time
Prognosis
Prothrombin Time
Respiratory Distress Syndrome, Adult/*etiology/mortality
Retrospective Studies
Survival Rate
Young Adult
Figure
Reference
-
1. Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000. 342:1334–1349.2. Meduri GU. The role of the host defence response in the progression and outcome of ARDS: pathophysiological correlations and response to glucocorticoid treatment. Eur Respir J. 1996. 9:2650–2670.3. Meduri GU, Annane D, Chrousos GP, Marik PE, Sinclair SE. Activation and regulation of systemic inflammation in ARDS: rationale for prolonged glucocorticoid therapy. Chest. 2009. 136:1631–1643.4. Idell S. Coagulation, fibrinolysis, and fibrin deposition in acute lung injury. Crit Care Med. 2003. 31:S213–S220.5. Schultz MJ, Haitsma JJ, Zhang H, Slutsky AS. Pulmonary coagulopathy as a new target in therapeutic studies of acute lung injury or pneumonia--a review. Crit Care Med. 2006. 34:871–877.6. McClintock D, Zhuo H, Wickersham N, Matthay MA, Ware LB. Biomarkers of inflammation, coagulation and fibrinolysis predict mortality in acute lung injury. Crit Care. 2008. 12:R41.7. Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994. 149:818–824.8. Trachsel D, McCrindle BW, Nakagawa S, Bohn D. Oxygenation index predicts outcome in children with acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2005. 172:206–211.9. Ben-Abraham R, Moreh O, Augerten A, Vardi A, Harel R, Barzilay Z, Paret G. Adapting prognostic respiratory variables of ARDS in children to small-scale community needs. J Crit Care. 1999. 14:120–124.10. Goldstein B, Giroir B, Randolph A. International Consunsus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005. 6:2–8.11. Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med. 1996. 24:743–752.12. Lee YS, Kim S, Kang EK, Park JD. Antithrombin-III as an early prognostic factor in children with acute lung injury. Korean J Pediatr. 2007. 50:443–448.13. Walsh TS, Stanworth SJ, Prescott RJ, Lee RJ, Watson DM, Wyncoll D. Writing Committee of the Intensive Care Study of Coagulopathy Investigators. Prevalence, management, and outcomes of critically ill patients with prothrombin time prolongation in United Kingdom intensive care units. Crit Care Med. 2010. 38:1939–1946.14. Eisele B, Lamy M, Thijs LG, Keinecke HO, Schuster HP, Matthias FR, Fourrier F, Heinrichs H, Delvos U. Antithrombin III in patients with severe sepsis. A randomized, placebo-controlled, double-blind multicenter trial plus a meta-analysis on all randomized, placebo-controlled, double-blind trials with antithrombin III in severe sepsis. Intensive Care Med. 1998. 24:663–672.15. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001. 344:699–709.16. Warren BL, Eid A, Singer P, Pillay SS, Carl P, Novak I, Chalupa P, Atherstone A, Penzes I, Kubler A, et al. Caring for the critically ill patient. Highdose antithrombin III in severe sepsis: a randomized controlled trial. JAMA. 2001. 286:1869–1878.17. van der Poll T, Levi M, Nick JA, Abraham E. Activated protein C inhibits local coagulation after intrapulmonary delivery of endotoxin in humans. Am J Respir Crit Care Med. 2005. 171:1125–1128.18. Laterre PF, Wittebole X, Dhainaut JF. Anticoagulant therapy in acute lung injury. Crit Care Med. 2003. 31:S329–S336.19. MacLaren R, Stringer KA. Emerging role of anticoagulants and fibrinolytics in the treatment of acute respiratory distress syndrome. Pharmacotherapy. 2007. 27:860–873.20. Welty-Wolf KE, Carraway MS, Miller DL, Ortel TL, Ezban M, Ghio AJ, Idell S, Piantadosi CA. Coagulation blockade prevents sepsis-induced respiratory and renal failure in baboons. Am J Respir Crit Care Med. 2001. 164:1988–1996.21. Miller DL, Welty-Wolf K, Carraway MS, Ezban M, Ghio A, Suliman H, Piantadosi CA. Extrinsic coagulation blockade attenuates lung injury and proinflammatory cytokine release after intratracheal lipopolysaccharide. Am J Respir Cell Mol Biol. 2002. 26:650–658.22. Khan H, Belsher J, Yilmaz M, Afessa B, Winters JL, Moore SB, Hubmayr RD, Gajic O. Fresh-frozen plasma and platelet transfusions are associated with development of acute lung injury in critically ill medical patients. Chest. 2007. 131:1308–1314.23. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000. 342:1301–1308.24. Meduri GU, Headley AS, Golden E, Carson SJ, Umberger RA, Kelso T, Tolley EA. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1998. 280:159–165.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antithrombin-III as an early prognostic factor in children with acute lung injury
- The Effect of Acute Coagulopathy in Profoundly Traumatic Patients on Acute and Early Deaths
- Lung repair after acute lung injury
- Plasminogen activator inhibitor(PAI-1) and factor VIII in acute lung injury
- A Case of Acute Lung Injury after Transfusion during Cesarean Section: A Case Report