J Korean Med Sci.
2006 Feb;21(1):143-150. 10.3346/jkms.2006.21.1.143.
Experience of a Korean Disaster Medical Assistance Team in Sri Lanka after the South Asia Tsunami
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea. suhgil@snu.ac.kr
- 21339 Seoul Emergency Information Center, Seoul, Korea.
- KMID: 2157798
- DOI: http://doi.org/10.3346/jkms.2006.21.1.143
Abstract
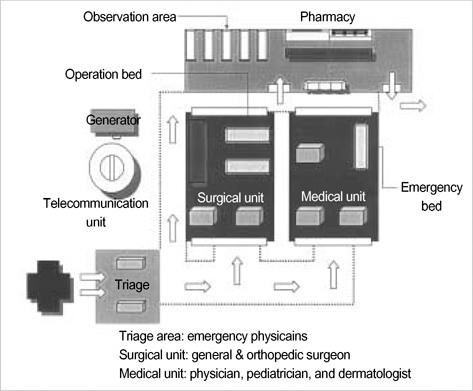
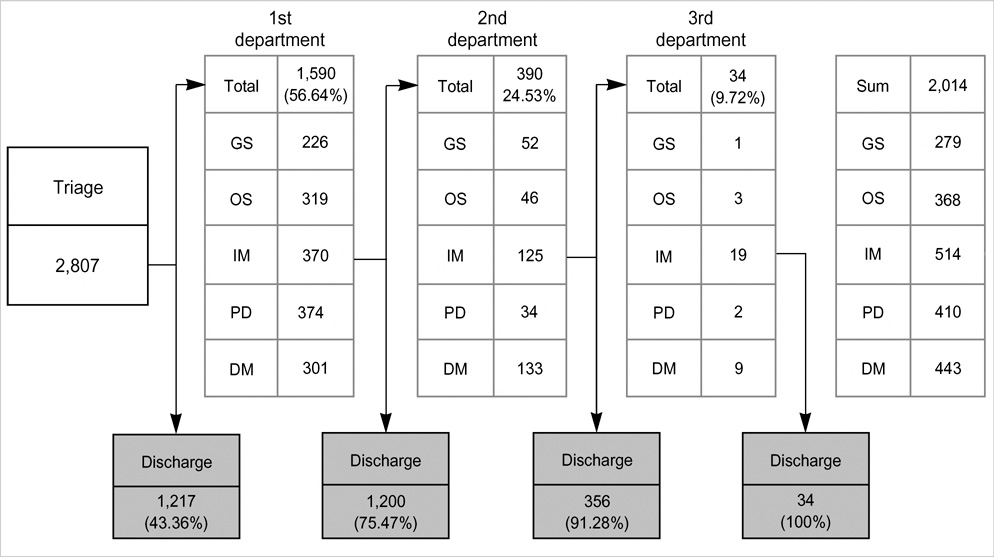
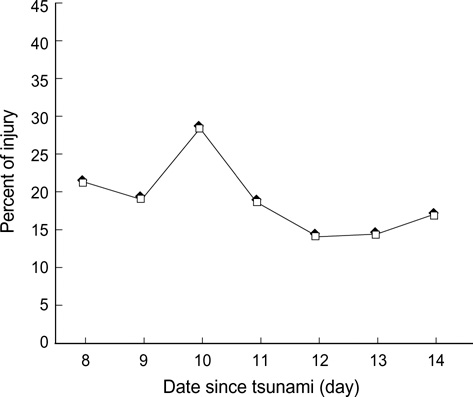
- On 26 December 2004, a huge tsunami struck the coasts of South Asian countries and it resulted in 29,729 deaths and 16,665 injuries in Sri Lanka. This study characterizes the epidemiology, clinical data and time course of the medical problems seen by a Korean disaster medical assistance team (DMAT) during its deployment in Sri Lanka, from 2 to 8 January 2005. The team consisting of 20 surgical and medical personnel began to provide care 7 days after tsunami in the southern part of Sri Lanka, the Matara and Hambantota districts. During this period, a total of 2,807 patients visited our field clinics with 3,186 chief complaints. Using the triage and refer system, we performed 3,231 clinical examinations and made 3,259 diagnoses. The majority of victims had medical problems (82.4%) rather than injuries (17.6%), and most conditions (92.1%) were mild enough to be discharged after simple management. There were also substantial needs of surgical managements even in the second week following the tsunami. Our study also suggests that effective triage system, self-sufficient preparedness, and close collaboration with local authorities may be the critical points for the foreign DMAT activity.
MeSH Terms
-
Adolescent
Adult
Aged
Asia, Southeastern
Child
Child, Preschool
Emergency Medical Services/organization & administration/statistics & numerical data
Female
Geography
Humans
Infant
Infant, Newborn
International Cooperation
Korea
Male
*Medical Assistance
Middle Aged
*Natural Disasters
Patients/classification/*statistics & numerical data
*Relief Work
Retrospective Studies
Sri Lanka
Figure
Cited by 1 articles
-
Disaster medicine: current status and future directions of emergency medical team for overseas disaster crisis
Minhong Choa, Jiyoung Noh, Hyun Soo Chung
J Korean Med Assoc. 2017;60(2):149-155. doi: 10.5124/jkma.2017.60.2.149.
Reference
-
1. Taylor PR, Emonson DL, Schlimmer JE. Operation Shaddock--the Australian Defense Force response to the tsunami disaster in Papua New Guinea. Med J Aust. 1998. 169:602–606.2. Holian AC, Keith PP. Orthopaedic surgery after the Aitape tsunami. Med J Aust. 1998. 169:606–609.
Article3. Asari Y, Koido Y, Nakamura K, Yamamoto Y, Ohta M. Analysis of medical needs on day 7 after the tsunami disaster in Papua New Guinea. Prehospital Disaster Med. 2000. 15:9–13.
Article4. South Asia earthquake and tsunamis. World Health Organization. accession date: 16 June 2005. Available from: http://www.who.int/hac/crises/international/asia_tsunami/en.5. Emergency Info. Disaster Management Unit of the Hon Prime Minister. accession date: 15 February 2005. Available from: http://www.emergencyinfo.gov.lk/index.html.6. Quick G, Hogan DE. Hogan DE, Burstein JL, editors. Research in disaster medicine. Disaster Medicine. 2002. Philadelphia: Lippincott Williams & Wilkins;395–403.7. Liang NJ, Shih YT, Shih FY, Wu HM, Wang HJ, Shi SF, Liu MY, Wang BB. Disaster epidemiology and medical response in the Chi-Chi earthquake in Taiwan. Ann Emerg Med. 2001. 38:549–555.
Article8. Pretto EA, Angus DC, Abrams JI, Shen B, Bissell R, Ruiz Castro VM, Sawyers R, Watoh Y, Ceciliano N, Ricci E. Disaster Reanimatology Study Group. An analysis of prehospital mortality in an earthquake. Prehosp Disaster Med. 1994. 9:107–117.
Article9. Hsu EB, Ma M, Lin FY, VanRooyen MJ, Burkle FM Jr. Emergency medical assistance team response following Taiwan Chi-Chi earthquake. Prehospital Disaster Med. 2002. 17:17–22.
Article10. Kim JW, Park SH, Jung YS, Cho JP. Analysis of medical service in the 1999 Turkey earthquake. J Korean Soc Emerg Med. 2001. 12:330–337.11. Song HG, Kang BS, Song KJ, Jeong YK. Subacute-stage organized medical support services in a disaster area: analysis of medical support in the 99 Taiwan earthquake. J Korean Soc Emerg Med. 2000. 11:362–371.12. McCarty DL. Hogan DE, Burstein JL, editors. Tsunamis. Disaster Medicine. 2002. Philadelphia: Lippincott Williams & Wilkins;229–234.13. Alson R, Alexander D, Leonard RB, Stringer LW. Analysis of medical treatment at a field hospital following Hurricane Andrew, 1992. Ann Emerg Med. 1993. 22:1721–1728.
Article14. Henderson AK, Lillibridge SR, Salinas C, Graves RW, Roth PB, Noji EK. Disaster medical assistance teams: providing health care to a community struck by Hurricane Iniki. Ann Emerg Med. 1994. 23:726–730.
Article15. Elder NJ, Greenouch PG. Hogan DE, Burstein JL, editors. Managing disasters in austere environments. Disaster Medicine. 2002. Philadelphia: Lippincott Williams & Wilkins;154–160.16. Brewer RD, Morris PD, Cole TB. Hurricane-related emergency department visits in an inland area: an analysis of the public health impact of Hurricane Hugo in North Carolina. Ann Emerg Med. 1994. 23:731–736.
Article17. Handrigan MT, Becker BM, Jagminas L, Becker TJ. Emergency medical services in the reconstruction phase following a major earthquake: a case study of the 1988 Armenia earthquake. Prehospital Disaster Med. 1998. 13:35–40.
Article18. Wallace AG. Hogan DE, Burstein JL, editors. National Disaster Medical System: Disaster medical assistance teams. Disaster Medicine. 2002. Philadelphia: Lippincott Williams & Wilkins;133–142.19. Mahoney LE, Whiteside DF, Belue HE, Mortisugu KP, Esch VH. Disaster medical assistance teams. Ann Emerg Med. 1987. 16:354–358.
Article20. Schultz CH, Koenig KL, Noji EK. A medical disaster response to reduce immediate mortality after an earthquake. N Engl J Med. 1996. 334:438–444.
Article21. Redmond AD, Watson S, Nightingale P. The south Manchester Accident Rescue Team and the earthquake in Iran, June 1990. BMJ. 1991. 302:1521–1523.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- E-waste scenario in South-Asia: an emerging risk to environment and public health
- The Growing Problem of Radiologist Shortage in Sri Lanka
- Experiences and lessons of the disaster medical assistance in Korea
- Disaster Medical Assistance Team
- Neglecting the neglected during the COVID-19 pandemic: the case of leptospirosis in Sri Lanka