J Korean Med Sci.
2004 Aug;19(4):631-633. 10.3346/jkms.2004.19.4.631.
Anticholinesterase Therapy for Patients with Ophthalmoplegia Following Snake Bites: Report of Two Cases
- Affiliations
-
- 1Department of Emergency Medicine, College of Medicine, Korea University, Seoul, Korea. kuedchoi@korea.ac.kr
- KMID: 2157701
- DOI: http://doi.org/10.3346/jkms.2004.19.4.631
Abstract
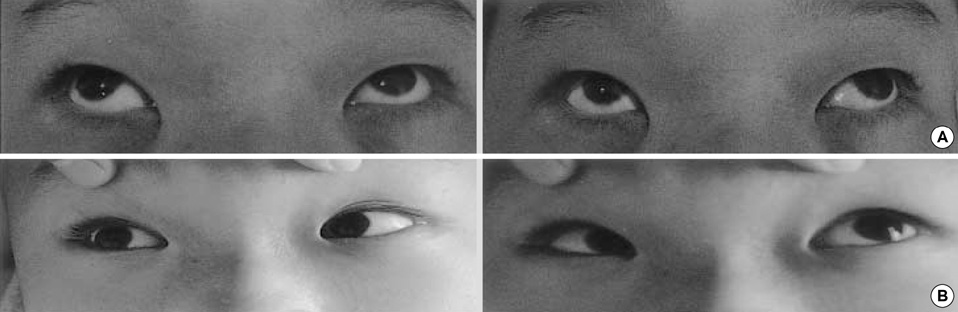
- Although ophthalmoplegia following snake bites is not indicative of a serious neurotoxic complication, symptoms of diplopia, dizziness and ocular discomfort can be emotionally devastating for patients. The authors experienced two cases of ophthalmoplegia following snake bites in Korea. The patients complained of diplopia that had developed several hours after the snake bites. The diplopia did not improve with antivenom treatment, but resolved completely after several injections of neostigmine.
MeSH Terms
Figure
Reference
-
1. Yoon JW, Kwon DM, Choi CD, Choi YK. A case of visual disturbance by viper bite. J Korean Ophthalmol Soc. 1970. 11:159–161.2. Sung CK, Hah MC. A case of extraocular muscle paresis by viper bite. J Korean Ophthalmol Soc. 1981. 22:261–263.3. Gaar GG, Normann SA. Ford MD, Delaney KA, Ling LJ, Erickson T, editors. Coral snake. Clinical toxicology. 2001. 1st ed. Philadelphia: W.B. Saunders Company;873–877.4. Nordt SP, Clark RF. Ford MD, Delaney KA, Ling LJ, Erickson T, editors. Rattlesnakes and other crotalids. Clinical toxicology. 2001. 1st ed. Philadelphia: W.B. Saunders Company;863–872.5. Ellenhorn MJ, Schonwald S, Ordog G, Wasserberger J. Ellenhorn's medical toxicology: Diagnosis and treatment of human poisoning. 1997. 2nd ed. Baltimore (Maryland): Williams & Wilkins;1739–1764.6. Lalloo DG, Trevett AJ, Korinhona A, Nwokolo N, Laurenson IF, Paul M, Black J, Naraqi S, Mavo B, Saweri A. Snake bites by the Papuan taipan (Oxyuranus scutellatus canni): paralysis, hemostatic and electrocardiographic abnormalities, and effects of antivenom. Am J Trop Med Hyg. 1995. 52:525–531.
Article7. Dart RC, Gomez HF, Daly FFS. Tintinalli JE, Kelen GD, Stapczynski JS, editors. Reptile bites. Emergency medicine: A comprehensive study guide. 2000. 5th ed. New York: McGraw-Hill;1251–1256.8. Gallagher EJ. Goldfrank LR, Flomenbaum NE, Lewin NA, Howland MA, Hoffman RS, Nelson LS, editors. Neurologic principles. Goldfrank's Toxicologic emergencies. 2002. 7th ed. New York: McGraw-Hill;282–302.9. Roberts JR, Otten EJ. Goldfrank LR, Flomenbaum NE, Lewin NA, Howland MA, Hoffman RS, Nelson LS, editors. Snakes and other reptiles. Goldfrank's Toxicologic emergencies. 2002. 7th ed. New York: McGraw-Hill;1552–1567.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case with Ophthalmoplegia Following Snake Bite
- Ocular Manifestations of Venomous Snake Bite over a One-year Period in a Tertiary Care Hospital
- Anticholinesterase Treatment for Patients With Paralytic Strabismus Following a Viper Bite
- A Case Report of Snake bites During Pregnancy
- The clinical evaluation of decompressio fasciotomy for swollen extremities