J Korean Ophthalmol Soc.
2009 Nov;50(11):1698-1704.
Anticholinesterase Treatment for Patients With Paralytic Strabismus Following a Viper Bite
- Affiliations
-
- 1Department of Ophthalmology, Dongguk University Gyeongju Hospital, Gyeongju, Korea. letter0116@naver.com
Abstract
- PURPOSE
To describe the therapeutic effect of anticholinesterase treatment for patients with paralytic strabismus and blepharoptosis following a viper bite
METHODS
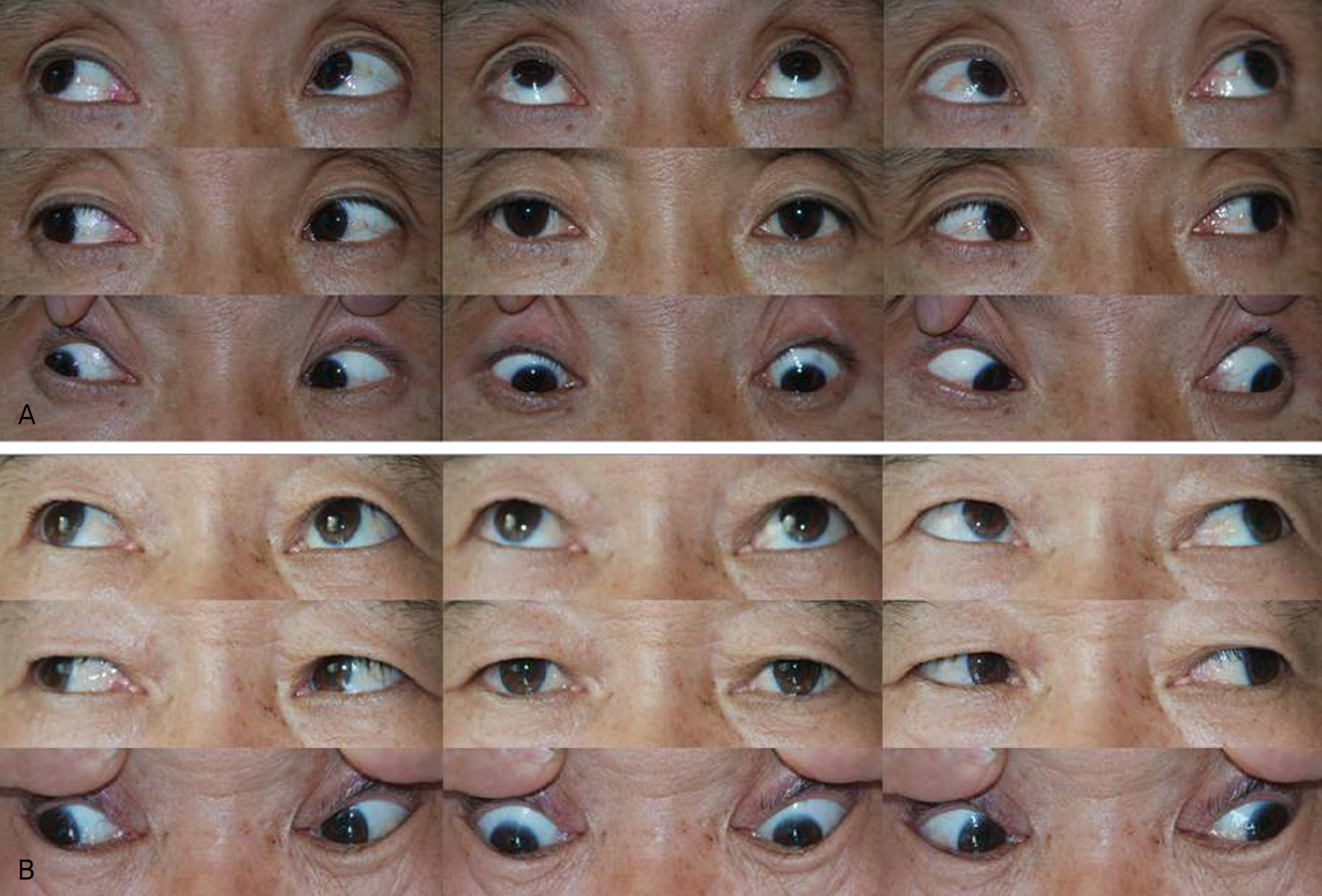
A prospective non-comparative interventional case series study was designed including 6 patients with ophthalmic complications such as paralytic strabismus and blepharoptosis following a viper bite. Anticholinesterase (pyridostigmine) 60 mg was administered to patients 3 times a day in additional to conservative treatment including antivenom, antibiotics and tetanus toxoid. Patients underwent a measurement of deviation, diplopia test and MRD 1. Subjective evaluation of the diplopia symptoms was performed daily after treatment.
RESULTS
Subjective diplopia was relieved in 2 out of the 6 patients on the first day and in the other 4 patients on the second day. The angle of deviation decreased approximately 37% on the first day and ocular position became orthophoric on the third day in all patients. The blepharoptosis was completely resolved in 4 patients on the first day. No complication following anticholinesterase treatment was noticed.
CONCLUSIONS
Treatment using anticholinesterase for patients suffering from diplopia and blepharoptosis following a viper bite is an effective and safe treatment.
MeSH Terms
Figure
Reference
-
References
1. Russell FE. Snake venom poisoning in the United States. Annu Rev Med. 1980; 31:247–59.
Article2. Ari AB. Patient with purely extraocular manifestation from a pit viper snakebite. Mil Med. 2001; 16:667–9.3. Moore TC. Snakebite from the Korean pit viper. Mil Med. 1977; 142:546–9.
Article4. Campbell CH. The effects of snake venoms and their neurotoxins on the nervous system of man and animals. Contemp Neurol Ser. 1975; 12:259–93.5. Yoon JW, Choi CD, Kwon MD, Choi YK. A case of visual distur-bance by viper bites. J Korean Ophthalmol Soc. 1970; 11:159–61.6. Sung CK, Ha MC. A case of extraocular muscle paresis by viper bite. J Korean Ophthalmol Soc. 1981; 22:261–3.7. Lee SW, Jung IC, Yoon YH, et al. Anticholinesterse therapy for patients with ophthalmoplegia following snake bites: report of two cases. J Korean Med Sci. 2004; 19:631–3.8. Paik NK, Son JR. The clinical character of Korean poisonous snake bite. J Korean Surg Soc. 1996; 51:119–27.9. Kinoshita T, Ohba N, Sasaki N. A case of bilateral medial rectus paresis following bite by a viper. Jpn J Clin Ophthalmol. 1998; 52:1741–3.10. Sugihara H, Nimura A, Kato T, Nikita T. Enzymochemical studies on snake venoms. X. Purification and properties of arginine ester hydrolase (ME-3) in the venom of Trimeresurus mucrosquamatus. Yakugaku Zasshi. 1982; 102:560–7.
Article11. Chang CC, Chen HM, Lin MF, Yang CC. Immunochemical studies on cobra venom toxin. Toxicon. 1976; 14:408–9.12. Cho IO, Chang SD, Lee SY. Paralytic exotropia from pit viper snakebite. J Korean Ophthalmol Soc. 2004; 45:1939–44.13. Von Noorden GK. Binocular vision and ocular motility. Theory and management of strabismus. 6th ed.St. Lous: C.V Mosby;2002. p. 101–13.14. Campolattaro BN, Wang FM. Anatomy and physiology of the extraocular muscles and surrounding tissues. 3th ed.Philadelpia: Mosby;1999. p. 6–8.15. Re G, Trisolino G, Miglio F. Eye muscle paralysis after Vipera aspis envenomation. J Accid Emerg Med. 1999; 16:458.
Article16. Antonini G, Rasura M, Conti G, Mattia C. Neuromuscular paralysis in Vipera aspis envenomation: pathogenetic mechanism. J Nerol Neurosurg Psychiatry. 1991; 54:187.17. Fauci AS, Braunwald E, Kasper DL, et al. Harrison's principles of internal medicine. 15th ed.New York: McGraw-Hill;2001. p. 382.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Paralytic Strabismus after a Snake Bite on the Toe
- Paralytic Exotropia from Pit Viper Snakebite
- Binocular Visual Rehabilitation in Paralytic Strabismus by Botulinum A Toxin Chemodenervation
- Botulinum Toxin A Chemodenervation in Strabismus
- The Effect of Botulinum Toxin Chemodenervation in Chronic Paralytic Strabismus