Ann Dermatol.
2011 Oct;23(Suppl 2):S151-S154. 10.5021/ad.2011.23.S2.S151.
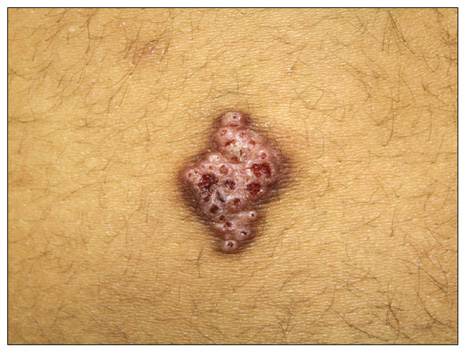
Syringocystadenoma Papilliferum of the Back Combined with a Tubular Apocrine Adenoma
- Affiliations
-
- 1Department of Dermatology, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea. leejd@olmh.cuk.ac.kr
- KMID: 2156777
- DOI: http://doi.org/10.5021/ad.2011.23.S2.S151
Abstract
- Syringocystadenoma papilliferum (SCAP) and tubular apocrine adenoma (TAA) are rare benign sweat gland tumors. SCAP and TAA may have a histopathologic overlap, but few cases of a SCAP combined with a TAA have been reported. Herein we describe an unusual case of a SCAP co-existing with a TAA located on the back of a 12-year-old girl.
MeSH Terms
Figure
Reference
-
1. Taylor RS, Perone JB, Kaddu S, Kerl H. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Appendage tumors and hamartomas of the skin. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw Hill;1068–1087.2. Ahmed TS, Priore JD, Seykora JT. Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Tumors of the epidermal appendages. Lever's histopathology of the skin. 2008. 10th ed. Philadelphia: Lippincott Williams & Wilkins;858–8602.3. Toribio J, Zulaica A, Peteiro C. Tubular apocrine adenoma. J Cutan Pathol. 1987. 14:114–117.
Article4. Ansai S, Watanabe S, Aso K. A case of tubular apocrine adenoma with syringocystadenoma papilliferum. J Cutan Pathol. 1989. 16:230–236.
Article5. Epstein BA, Argenyi ZB, Goldstein G, Whitaker D. An unusual presentation of a congenital benign apocrine hamartoma. J Cutan Pathol. 1990. 17:53–58.
Article6. Ishiko A, Shimizu H, Inamoto N, Nakmura K. Is tubular apocrine adenoma a distinct clinical entity? Am J Dermatopathol. 1993. 15:482–487.
Article7. Aktepe F, Demir Y, Dilek FH. Tubular apocrine adenoma in association with syringocystadenoma papilliferum. Dermatol Online J. 2003. 9:7.
Article8. Ahn BK, Park YK, Kim YC. A case of tubular apocrine adenoma with syringocystadenoma papilliferum arising in nevus sebaceus. J Dermatol. 2004. 31:508–510.
Article9. Lee CK, Jang KT, Cho YS. Tubular apocrine adenoma with syringocystadenoma papilliferum arising from the external auditory canal. J Laryngol Otol. 2005. 119:1004–1006.
Article10. Yamane N, Kato N, Yanagi T, Osawa R. Naevus sebaceus on the female breast accompanied with a tubular apocrine adenoma and a syringocystadenoma papilliferum. Br J Dermatol. 2007. 156:1397–1399.
Article11. Vazmitel M, Michal M, Mukensnabl P, Kazakov DV. Syringocystadenoma papilliferum with sebaceous differentiation in an intradermal tubular apocrine component. Report of a case. Am J Dermatopathol. 2008. 30:51–53.
Article12. Kim MS, Lee JH, Lee WM, Son SJ. A case of tubular apocrine adenoma with syringocystadenoma papilliferum that developed in a nevus sebaceus. Ann Dermatol. 2010. 22:319–322.
Article13. Kazakov DV, Bisceglia M, Calonje E, Hantschke M, Kutzner H, Mentzel T, et al. Tubular adenoma and syringocystadenoma papilliferum: a reappraisal of their relationship. An interobserver study of a series, by a panel of dermatopathologists. Am J Dermatopathol. 2007. 29:256–263.
Article14. Townsend TC, Bowen AR, Nobuhara KK. Syringocystadenoma papilliferum: an unusual cutaneous lesion in a pediatric patient. J Pediatr. 2004. 145:131–133.
Article15. Hann SK, Choi YS, Choi EH. Syringocystadenoma papilliferum. Ann Dermatol. 1990. 2:100–104.16. Requena L, Kiryu H, Ackerman AB. Neoplasms with apocrine differentiation. 1998. Philadelphia, PA: Lippicott-Raven.17. James WD, Berger TG, Elston DM. Epidermal nevi, neoplasms, and cysts. Andrews' diseases of the skin clinical dermatology. 2006. 10th ed. Philadelphia: Elsevier;633–683.18. Falck VG, Jordaan HF. Papillary eccrine adenoma. A tubulopapillary hidradenoma with eccrine differentiation. Am J Dermatopathol. 1986. 8:64–72.19. Hsu PJ, Liu CH, Huang CJ. Mixed tubulopapillary hidradenoma and syringocystadenoma papilliferum occurring as a verrucous tumor. J Cutan Pathol. 2003. 30:206–210.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Syringocystadenoma Papilliferum in Co-existence with Tubular Apocrine Adenoma on the Calf
- A Case of Tubular Apocrine Adenoma with Syringocystadenoma Papilliferum that Developed in a Nevus Sebaceus
- A Cases of Nevus Sebaceus of Jandassohn Associated with Tubular Apocrine Adenoma
- A Case of Tubular Apocrine Adenoma
- Three Cases Showing Combined Features of Syringocystadenoma Papilliferum andTubular Apocrine Adenoma Superimposed on Nevus Sebaceus