Korean J Crit Care Med.
2015 Nov;30(4):265-271. 10.4266/kjccm.2015.30.4.265.
Brain Magnetic Resonance Imaging in Patients with Favorable Outcomes after Out-of-Hospital Cardiac Arrest: Many Have Encephalopathy Even with a Good Cerebral Performance Category Score
- Affiliations
-
- 1Department of Emergency Medicine, Gachon University Gil Medical Center, Incheon, Korea. empearl@giilhospital.com
- KMID: 2156179
- DOI: http://doi.org/10.4266/kjccm.2015.30.4.265
Abstract
- BACKGROUND
The aim of this study was to retrospectively evaluate and analyze the brain magnetic resonance imaging (B-MRI) findings of patients with a favorable neurological outcome following cerebral performance category (CPC) after out-of-hospital cardiac arrest (OHCA) at single university hospital emergency center.
METHODS
Patients with return of spontaneous circulation (> 24 h) after OHCA who were older than 16 years of age and who had been admitted to the emergency intensive care unit (EICU) for over a 57-month period between July 2007 and March 2012 and survived with a favorable neurological outcome were enrolled. B-MRI was taken after recovery of their mental status.
RESULTS
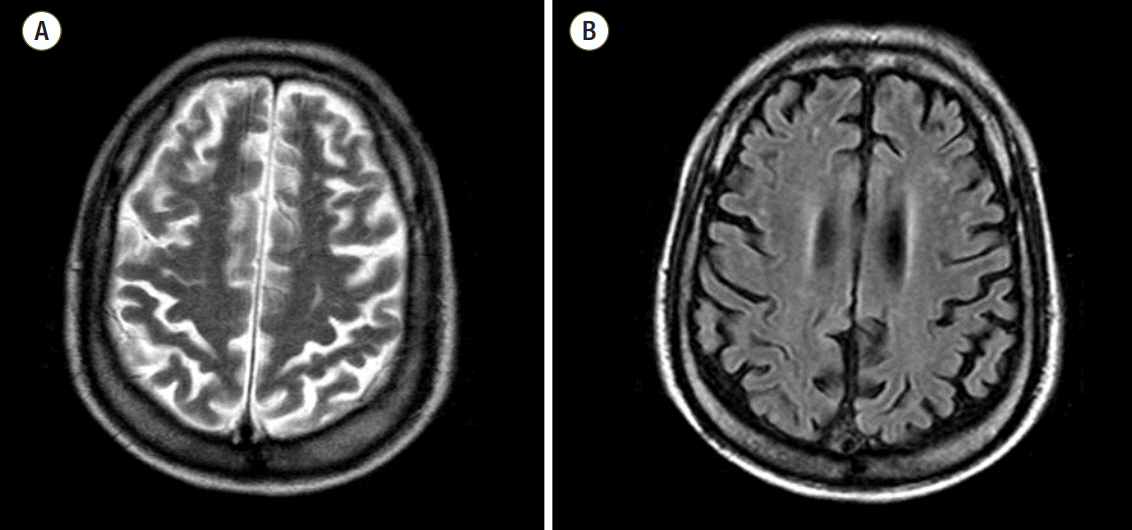
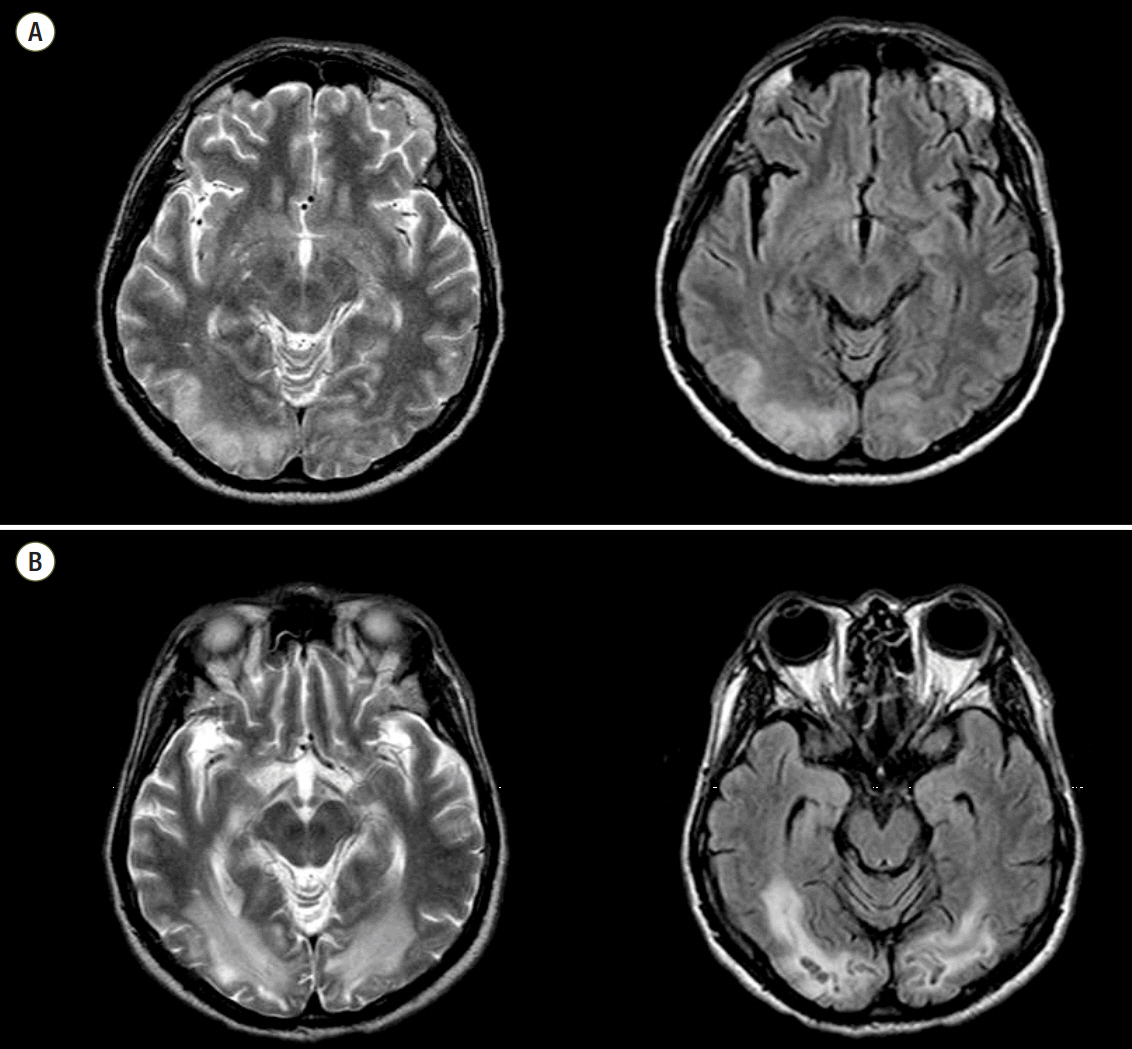
Fifty-two patients among the 305 admitted patients had a good CPC, and 33 patients' B-MRI were analyzed (CPC 1: 26 patients, CPC 2: 7 patients). Among these, 18 (54.5%) patients had a normal finding on B-MRI. On the other hand, ischemia/infarction/microangiopathy compatible with hypoxic-ischemic encephalopathy (HIE) were found on various brain areas including subcortical white matter (7/13), cerebral cortex, central semiovlae, basal ganglia, putamen, periventricular white matter, and cerebellum.
CONCLUSIONS
Survivors with a favorable neurological outcome from OHCA showed HIE on B-MRI, especially all of the patients with a CPC 2. More detail neurologic category including brain imaging would be needed to categorize patients with favorable outcome after OHCA.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Rosamon W, Flegal K, Furie K, Go A, Greenlund K, Haase N, et al. Heart disease and stroke statistics--2008 updates: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008; 117:e25–146.2. Ahn KO, Shin SD, Suh GJ, Cha WC, Song KJ, Kim SJ, et al. Epidemiology and outcomes from non-traumatic out-of-hospital cardiac arrest in Korea: a nationwide observational study. Resuscitation. 2010; 81:974–81.
Article3. Caine D, Watson JD. Neuropsychological and neuropathological sequelae of cerebral anoxia: a critical review. J Int Neuropsychol Soc. 2000; 6:86–99.
Article4. Roine RO, Kajaste S, Kaste M. Neuropsychological sequlae of cardiac arrest. JAMA. 1993; 269:237–42.5. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346:549–56.6. Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002; 346:557–63.
Article7. Peberdy MA, Callaway CW, Neumar RW, Geocardin RG, Zimmerman JL, Donnino M, et al. Part 9: postcardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122(18 Suppl 3):S768–86.8. Topcuoqlu MA, Oquz KK, Buyukserbetci G, Bulut E. Prognostic value of magnetic resonance imaging in post-resuscitation encephlaopathy. Intern Med. 2009; 48:1635–45.9. Kawahara H, Takeda Y, Tanaka A, Nagano O, Katayama H, Hirakawa M, et al. Does diffusion-weighted magnetic resonance imaging enable detection of early ischemic change following transient cerebral ischemia? J Neurol Sci. 2000; 181:73–81.
Article10. Arbelaez A, Castillo M, Mukherji SK. Diffusion-weignted MR imaging of global cerebral anoxia. AJNR Am J Neuroradiol. 1999; 20:999–1007.11. Els T, Kassubek J, Kubalek R, Klisch J. Diffusion-weighted MRI during early global cerebral hyoxia: a predictor for clinical outcome? Acta Neurol Scand. 2004; 110:361–7.12. Weiss N, Galanaud D, Carpentier A, Naccache L, Puybasset L. Clinical review: prognostic value of magnetic resonance imaging in acute brain injury and coma. Crit Care. 2007; 11:230.
Article13. Singhal AB, Topcuoqlu MA, Koroshetz WJ. Diffusion MRI in three types of anoxic encephalopathy. J Neurol Sci. 2002; 196:37–40.
Article14. Greer D, Scripko P, Bartscher J, Sims J, Camargo E, Singhal A, et al. Serial MRI changes in comatose cardiac arrest patients. Neurocrit Care. 2011; 14:61–7.
Article15. Wijdicks EF, Campeau NG, Miller GM. MR imaging in comatose survivors of cardiac resuscitation. AJNR Am J Neuroradiol. 2001; 22:1561–5.16. Wu O, Sorensen AG, Benner T, Singhal AB, Furie KL, Greer DM, et al. Comatose patients with cardiac arrest: predicting clinical outcome with diffusion-weighted MR imaging. Radiology. 2009; 252:173–81.
Article17. Konaka K, Miyashita K, Naritomi H. Changes in diffusion-weighted magnetic resonance imaging findings in the acute and subacute phases of anoxic enecephalopathy. J Stroke Cerebrovasc Dis. 2007; 16:82–3.18. Friberg H, Rundgren M, Westhall E, Nielsen N, Cronberg T. Continuous evaluation of neurological prognosis after cardiac arrest. Acta Anaesthesiol Scand. 2013; 57:6–15.
Article19. Samaniego EA, Persoon S, Wijman CA. Prognosis after cardiac arrest and hypothermia: a new paradigm. Curr Neurol Neurosci Rep. 2011; 11:111–9.
Article20. van Alem AP, de Vos R, Schmand B, Koster RW. Cognitive impairment in survivors of out-of-hospital cardiac arrest. Am J Heart. 2004; 148:416–21.
Article21. Grubb NR, O’Carroll R, Cobbe SM, Sirel J, Fox KA. Chronic memory impairment after cardiac arrest outside hospital. BMJ. 1996; 313:143–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complete Recovery of Perfusion Abnormalities in a Cardiac Arrest Patient Treated with Hypothermia: Results of Cerebral Perfusion MR Imaging
- Utility of Susceptibility-Weighted Imaging in Comatose Patients after Cardiac Arrest: A Preliminary Study
- The Usefulness of Proton Magnetic Resonance Spectroscopy in Comatose Patients after Successful Cardiopulmonary Resuscitation
- A Case of Congenital Cytomegalovirus Encephalopathy with Patchy, Nodular Lesion of Periventricular area on Brain Magnetic Resonance Imaging
- Efficacies of Somatosensory Evoked Potential and Diffusion-Weighted Magnetic Resonance Imaging as Predictors of Prognosis for Patients Experiencing Coma after Cardiac Arrest