Korean J Radiol.
2015 Jun;16(3):604-612. 10.3348/kjr.2015.16.3.604.
Cervical Interlaminar Epidural Steroid Injection for Unilateral Cervical Radiculopathy: Comparison of Midline and Paramedian Approaches for Efficacy
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. jwjwkwon@gmail.com
- 2School of Business Administration, Hallym University, Chuncheon 200-702, Korea.
- KMID: 2155530
- DOI: http://doi.org/10.3348/kjr.2015.16.3.604
Abstract
OBJECTIVE
The objective of this study was to compare the clinical outcomes of the cervical interlaminar epidural steroid injection (CIESI) for unilateral radiculopathy by the midline or paramedian approaches and to determine the prognostic factors of CIESI.
MATERIALS AND METHODS
We retrospectively analyzed 182 patients who underwent CIESI from January 2009 to December 2012. Inclusion criteria were no previous spinal steroid injection, presence of a cross-sectional image, and presence of follow-up records. Exclusion criteria were patients with bilateral cervical radiculopathy and/or dominant cervical axial pain, combined peripheral neuropathy, and previous cervical spine surgery. Short-term clinical outcomes were evaluated at the first follow-up after CIESI. We compared the clinical outcomes between the midline and paramedian approaches. Possible prognostic factors for the outcome, such as age, gender, duration of radiculopathy, and cause of radiculopathy were also analyzed.
RESULTS
Cervical interlaminar epidural steroid injections were effective in 124 of 182 patients (68.1%) at the first follow-up. There was no significant difference in the clinical outcomes of CIESI, between midline (69.6%) and paramedian (63.7%) approaches (p = 0.723). Cause of radiculopathy was the only significant factor affecting the efficacy of CIESI. Patients with disc herniation had significantly better results than patients with neural foraminal stenosis (82.9% vs. 56.0%) (p < 0.001).
CONCLUSION
There is no significant difference in treatment efficacy between the midline and paramedian approaches in CIESI, for unilateral radiculopathy. The cause of the radiculopathy is significantly associated with the treatment efficacy; patients with disc herniation experience better pain relief than those with neural foraminal stenosis.
Keyword
MeSH Terms
-
Adrenal Cortex Hormones/*therapeutic use
Adult
Aged
Cervical Cord/physiopathology
Cross-Sectional Studies
Female
Humans
Injections, Epidural
Intervertebral Disc Displacement/*drug therapy/radiography
Male
Middle Aged
Radiculopathy/*drug therapy/radiography
Retrospective Studies
Treatment Outcome
Adrenal Cortex Hormones
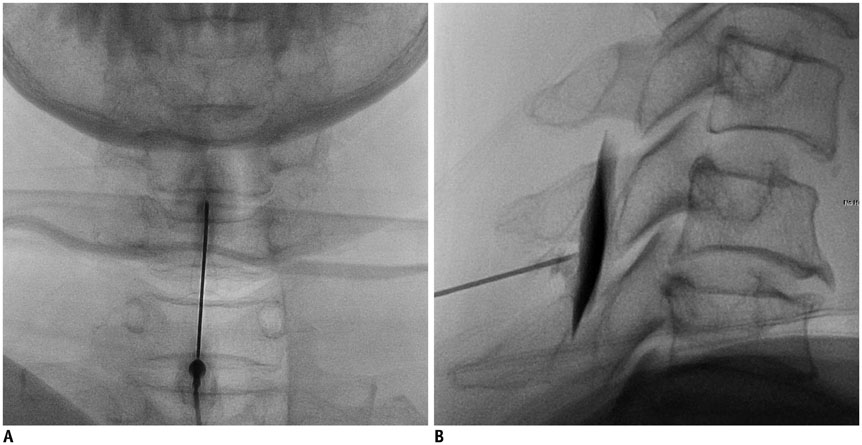
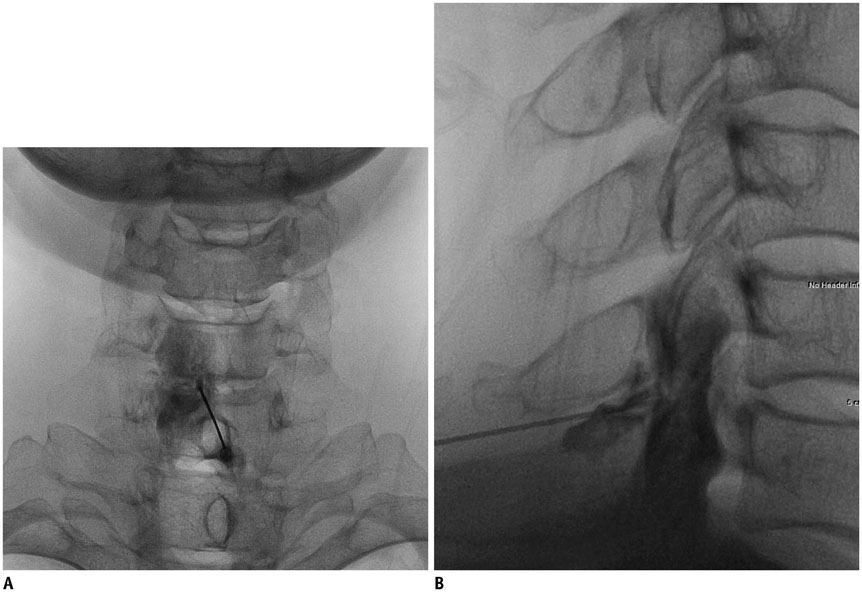
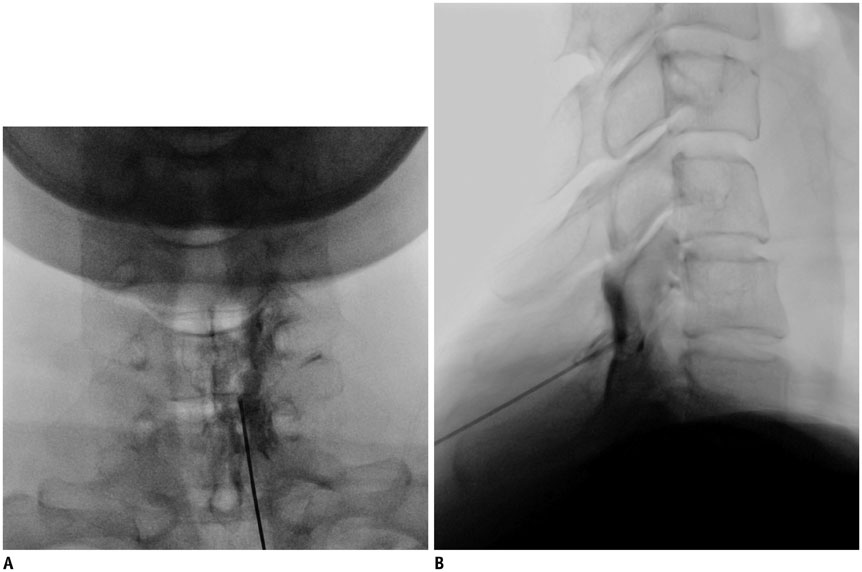
Figure
Reference
-
1. Benyamin RM, Singh V, Parr AT, Conn A, Diwan S, Abdi S. Systematic review of the effectiveness of cervical epidurals in the management of chronic neck pain. Pain Physician. 2009; 12:137–157.2. Diwan S, Manchikanti L, Benyamin RM, Bryce DA, Geffert S, Hameed H, et al. Effectiveness of cervical epidural injections in the management of chronic neck and upper extremity pain. Pain Physician. 2012; 15:E405–E434.3. Hogan QH. Epidural anatomy examined by cryomicrotome section. Influence of age, vertebral level, and disease. Reg Anesth. 1996; 21:395–406.4. Lirk P, Kolbitsch C, Putz G, Colvin J, Colvin HP, Lorenz I, et al. Cervical and high thoracic ligamentum flavum frequently fails to fuse in the midline. Anesthesiology. 2003; 99:1387–1390.5. Abbed KM, Coumans JV. Cervical radiculopathy: pathophysiology, presentation, and clinical evaluation. Neurosurgery. 2007; 60:1 Supp1 1. S28–S34.6. Fardon DF, Milette PC. Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976). 2001; 26:E93–E113.7. Czervionke LF, Fenton DS. Imaging painful spine disorders. 1st ed. Philadelphia: Saunders;2011. p. 180–187.8. Castagnera L, Maurette P, Pointillart V, Vital JM, Erny P, Sénégas J. Long-term results of cervical epidural steroid injection with and without morphine in chronic cervical radicular pain. Pain. 1994; 58:239–243.9. Lin EL, Lieu V, Halevi L, Shamie AN, Wang JC. Cervical epidural steroid injections for symptomatic disc herniations. J Spinal Disord Tech. 2006; 19:183–186.10. Kwon JW, Lee JW, Kim SH, Choi JY, Yeom JS, Kim HJ, et al. Cervical interlaminar epidural steroid injection for neck pain and cervical radiculopathy: effect and prognostic factors. Skeletal Radiol. 2007; 36:431–436.11. Strub WM, Brown TA, Ying J, Hoffmann M, Ernst RJ, Bulas RV. Translaminar cervical epidural steroid injection: short-term results and factors influencing outcome. J Vasc Interv Radiol. 2007; 18:1151–1155.12. Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. The effectiveness of fluoroscopic cervical interlaminar epidural injections in managing chronic cervical disc herniation and radiculitis: preliminary results of a randomized, double-blind, controlled trial. Pain Physician. 2010; 13:223–236.13. Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. Management of chronic pain of cervical disc herniation and radiculitis with fluoroscopic cervical interlaminar epidural injections. Int J Med Sci. 2012; 9:424–434.14. Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical postsurgery syndrome: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012; 15:13–25.15. Douglas S, Leo FC. Image-guided spine intervention. 1st ed. Philadelphia: Saunders;2002. p. 99–126.16. Huston CW. Cervical epidural steroid injections in the management of cervical radiculitis: interlaminar versus transforaminal. A review. Curr Rev Musculoskelet Med. 2009; 2:30–42.17. Abbasi A, Malhotra G, Malanga G, Elovic EP, Kahn S. Complications of interlaminar cervical epidural steroid injections: a review of the literature. Spine (Phila Pa 1976). 2007; 32:2144–2151.18. Rivest C, Katz JN, Ferrante FM, Jamison RN. Effects of epidural steroid injection on pain due to lumbar spinal stenosis or herniated disks: a prospective study. Arthritis Care Res. 1998; 11:291–297.19. Fish DE, Kobayashi HW, Chang TL, Pham Q. MRI prediction of therapeutic response to epidural steroid injection in patients with cervical radiculopathy. Am J Phys Med Rehabil. 2009; 88:239–246.20. Ferrante FM, Wilson SP, Iacobo C, Orav EJ, Rocco AG, Lipson S. Clinical classification as a predictor of therapeutic outcome after cervical epidural steroid injection. Spine (Phila Pa 1976). 1993; 18:730–736.21. Lee JW, Hwang SY, Lee GY, Lee E, Kang HS. Fluoroscopic cervical paramidline interlaminar epidural steroid injections for cervical radiculopathy: effectiveness and outcome predictors. Skeletal Radiol. 2014; 43:933–938.22. Goupille P, Jayson MI, Valat JP, Freemont AJ. The role of inflammation in disk herniation-associated radiculopathy. Semin Arthritis Rheum. 1998; 28:60–71.23. Flower RJ, Blackwell GJ. Anti-inflammatory steroids induce biosynthesis of a phospholipase A2 inhibitor which prevents prostaglandin generation. Nature. 1979; 278:456–459.24. Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand. 2006; 50:265–282.25. Lee JW, Park KW, Chung SK, Yeom JS, Kim KJ, Kim HJ, et al. Cervical transforaminal epidural steroid injection for the management of cervical radiculopathy: a comparative study of particulate versus non-particulate steroids. Skeletal Radiol. 2009; 38:1077–1082.26. Lee SH, Kim KT, Kim DH, Lee BJ, Son ES, Kwack YH. Clinical outcomes of cervical radiculopathy following epidural steroid injection: a prospective study with follow-up for more than 2 years. Spine (Phila Pa 1976). 2012; 37:1041–1047.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Cervical Radiculopathy with Epidural Steroid Injection
- Epidural Steroid Injection in the Treatment of Cervical Radiculopathy
- Treatment of Cervical Perineural Cyst by the Transforaminal Epidural Steroid Injection
- Correlation between Epidurographic Contrast Flow Patterns and Clinical Effectiveness in Chronic Lumbar Discogenic Radicular Pain Treated with Epidural Steroid Injections Via Different Approaches
- Painless cervical motor radiculopathy relieved by cervical epidural steroid injection: A case report