Correlation between Epidurographic Contrast Flow Patterns and Clinical Effectiveness in Chronic Lumbar Discogenic Radicular Pain Treated with Epidural Steroid Injections Via Different Approaches
- Affiliations
-
- 1Department of Anaesthesia, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India. drruchi_sgrd@rediff.com
- 2Department of Anaesthesia, Post Graduate Institute of Medical Education and research, Chandigarh, India.
- 3Department of Radiodiagnosis and Imaging, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India.
- KMID: 1802502
- DOI: http://doi.org/10.3344/kjp.2014.27.4.353
Abstract
- BACKGROUND
Epidural steroid injections are an accepted procedure for the conservative management of chronic backache caused by lumbar disc pathology. The purpose of this study was to evaluate the epidurographic findings for the midline, transforaminal and parasagittal approaches in lumbar epidural steroid injections, and correlating them with the clinical improvement.
METHODS
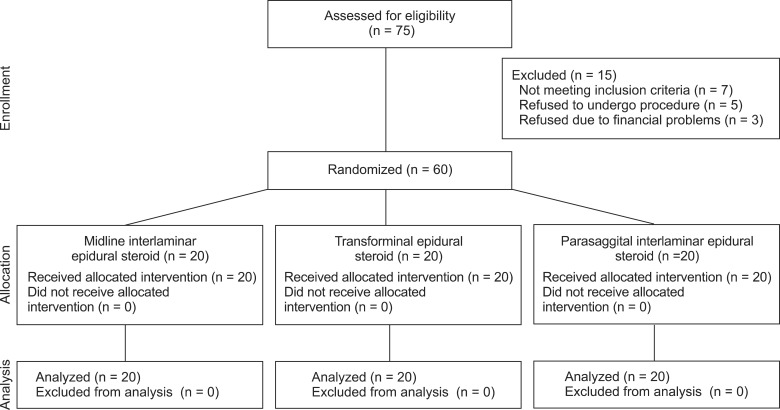
Sixty chronic lower back pain patients with unilateral radiculitis from a herniated/degenerated disc were enrolled. After screening the patients according to the exclusion criteria and randomly allocating them to 3 groups of 20 patients, fluoroscopic contrast enhanced epidural steroids were injected via midline (group 1), transforaminal (group 2) and parasagittal interlaminar (group 3) approaches at the level of the pathology. The fluoroscopic patterns of the three groups were studied and correlated with the clinical improvement measured by the VAS over the next 3 months; any incidences of complications were recorded.
RESULTS
The transforaminal group presented better results in terms of VAS reduction than the midline and parasagittal approach groups (P < 0.05). The epidurography showed a better ventral spread for both the transforaminal (P < 0.001) and the paramedian approaches (P < 0.05), as compared to the midline approach. The nerve root filling was greater in the transforaminal group (P < 0.001) than in the other two groups. The ventral spread of the contrast agent was associated with improvement in the VAS score and this difference was statistically significant in group 1 (P < 0.05), and highly significant in groups 2 and 3 (P < 0.001). In all the groups, any complications observed were transient and minor.
CONCLUSIONS
The midline and paramedian approaches are technically easier and statistically comparable, but clinically less efficacious than the transforaminal approach. The incidence of ventral spread and nerve root delineation show a definite correlation with clinical improvement. However, an longer follow-up period is advisable for a better evaluation of the actual outcom.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Ultrasound-guided pararadicular block using a paramedian sagittal oblique approach for managing low back pain in a pregnant woman -A case report-
Seul Gi Ahn, Jisoo Lee, Hue Jung Park, Young Hoon Kim
Anesth Pain Med. 2016;11(3):291-294. doi: 10.17085/apm.2016.11.3.291.What is the Role of Epidural Injections in the Treatment of Lumbar Discogenic Pain: A Systematic Review of Comparative Analysis with Fusion
Laxmaiah Manchikanti, Peter S. Staats, Devi E. Nampiaparampil, Joshua A. Hirsch
Korean J Pain. 2015;28(2):75-87. doi: 10.3344/kjp.2015.28.2.75.Sufficient explanation of management affects patient satisfaction and the practice of post-treatment management in spinal pain, a multicenter study of 1007 patients
Jae Yun Kim, Jae Hang Shim, Sung Jun Hong, Jong Yeun Yang, Hey Ran Choi, Yun Hee Lim, Ho Sik Moon, Jaemoon Lee, Jae Hun Kim
Korean J Pain. 2017;30(2):116-125. doi: 10.3344/kjp.2017.30.2.116.Comparison of clinical efficacy in epidural steroid injections through transforaminal or parasagittal approaches
Ji Hee Hong, Eun Kyul Park, Ki Bum Park, Ji Hoon Park, Sung Won Jung
Korean J Pain. 2017;30(3):220-228. doi: 10.3344/kjp.2017.30.3.220.Effect of needle type on intravascular injection in transforaminal epidural injection: a meta-analysis
Jae Yun Kim, Soo Nyoung Kim, Chulmin Park, Ho Young Lim, Jae Hun Kim
Korean J Pain. 2019;32(1):39-46. doi: 10.3344/kjp.2019.32.1.39.
Reference
-
1. Mehta M, Salmon N. Extradural block. Confirmation of the injection site by X-ray monitoring. Anaesthesia. 1985; 40:1009–1012. PMID: 4061788.
Article2. Botwin KP, Natalicchio J, Hanna A. Fluoroscopic guided lumbar interlaminar epidural injections: a prospective evaluation of epidurography contrast patterns and anatomical review of the epidural space. Pain Physician. 2004; 7:77–80. PMID: 16868616.3. McLain RF, Kapural L, Mekhail NA. Epidural steroid therapy for back and leg pain: mechanisms of action and efficacy. Spine J. 2005; 5:191–201. PMID: 15749619.
Article4. Candido KD, Raghavendra MS, Chinthagada M, Badiee S, Trepashko DW. A prospective evaluation of iodinated contrast flow patterns with fluoroscopically guided lumbar epidural steroid injections: the lateral parasagittal interlaminar epidural approach versus the transforaminal epidural approach. Anesth Analg. 2008; 106:638–644. PMID: 18227326.
Article5. Rosenberg SK, Grabinsky A, Kooser C, Boswell MV. Effectiveness of transforaminal epidural steroid injections in low back pain: a one year experience. Pain Physician. 2002; 5:266–270. PMID: 16902652.6. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976). 2002; 27:11–16. PMID: 11805628.7. Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009; 12:233–251. PMID: 19165306.8. Furman MB, Lee TS, Mehta A, Simon JI, Cano WG. Contrast flow selectivity during transforaminal lumbosacral epidural steroid injections. Pain Physician. 2008; 11:855–861. PMID: 19057631.9. Rados I, Sakic K, Fingler M, Kapural L. Efficacy of interlaminar vs transforaminal epidural steroid injection for the treatment of chronic unilateral radicular pain: prospective, randomized study. Pain Med. 2011; 12:1316–1321. PMID: 21914118.
Article10. Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehabil. 1998; 79:1362–1366. PMID: 9821894.
Article11. Smith CC, Booker T, Schaufele MK, Weiss P. Interlaminar versus transforaminal epidural steroid injections for the treatment of symptomatic lumbar spinal stenosis. Pain Med. 2010; 11:1511–1515. PMID: 20735751.
Article12. Botwin K, Natalicchio J, Brown LA. Epidurography contrast patterns with fluoroscopic guided lumbar transforaminal epidural injections:a prospective evaluation. Pain Physician. 2004; 7:211–215. PMID: 16868594.13. Choi YK, Barbella JD. Evaluation of epidurographic contrast patterns with fluoroscopic-guided lumbar interlaminar ventral epidural injection. Pain Pract. 2009; 9:275–281. PMID: 19490461.
Article14. Manchikanti L, Cash KA, Pampati V, Damron KS, McManus CD. Evaluation of lumbar transforaminal epidural injections with needle placement and contrast flow patterns: a prospective, descriptive report. Pain Physician. 2004; 7:217–223. PMID: 16868595.15. Desai MJ, Shah B, Sayal PK. Epidural contrast flow patterns of transforaminal epidural steroid injections stratified by commonly used final needle-tip position. Pain Med. 2011; 12:864–870. PMID: 21539705.
Article16. Yang SC, Fu TS, Lai PL, Niu CC, Chen LH, Chen WJ. Transforaminal epidural steroid injection for discectomy candidates: an outcome study with a minimum of two-year follow-up. Chang Gung Med J. 2006; 29:93–99. PMID: 16642732.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- What is the Role of Epidural Injections in the Treatment of Lumbar Discogenic Pain: A Systematic Review of Comparative Analysis with Fusion
- Persistent Hiccup after Epidural Steroid Injection: Case reports
- An Analysis of Pattern of Transforaminal Epidurography
- Evaluation of Contrast Flow Patterns with Fluoroscopic Guided Lumbar Transforaminal Epidural Injections
- Selective Epidural Steroid Injection in a Patient with Refractory Radicular Leg Pain: A case report