Ann Rehabil Med.
2016 Feb;40(1):21-27. 10.5535/arm.2016.40.1.21.
Crystallization of Local Anesthetics When Mixed With Corticosteroid Solutions
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. keewonkimm.d@gmail.com
- KMID: 2155161
- DOI: http://doi.org/10.5535/arm.2016.40.1.21
Abstract
OBJECTIVE
To evaluate at which pH level various local anesthetics precipitate, and to confirm which combination of corticosteroid and local anesthetic crystallizes.
METHODS
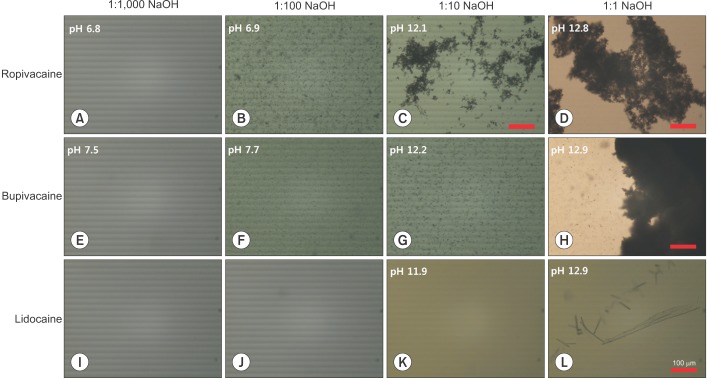
Each of ropivacaine-HCl, bupivacaine-HCl, and lidocaine-HCl was mixed with 4 different concentrations of NaOH solutions. Also, each of the three local anesthetics was mixed with the same volume of 3 corticosteroid solutions (triamcinolone acetonide, dexamethasone sodium phosphate, and betamethasone sodium phosphate). Precipitation of the local anesthetics (or not) was observed, by the naked eye and by microscope. The pH of each solution and the size of the precipitated crystal were measured.
RESULTS
Alkalinized with NaOH to a certain value of pH, local anesthetics precipitated (ropivacaine pH 6.9, bupivacaine pH 7.7, and lidocaine pH 12.9). Precipitation was observed as a cloudy appearance by the naked eye and as the aggregation of small particles (<10 µm) by microscope. The amount of particles and aggregation increased with increased pH. Mixed with betamethasone sodium phosphate, ropivacaine was precipitated in the form of numerous large crystals (>300 µm, pH 7.5). Ropivacaine with dexamethasone sodium phosphate also precipitated, but it was only observable by microscope (a few crystals of 10-100 µm, pH 7.0). Bupivacaine with betamethasone sodium phosphate formed precipitates of non-aggregated smaller particles (<10 µm, pH 7.7). Lidocaine mixed with corticosteroids did not precipitate.
CONCLUSION
Ropivacaine and bupivacaine can precipitate by alkalinization at a physiological pH, and therefore also produce crystals at a physiological pH when they are mixed with betamethasone sodium phosphate. Thus, the potential risk should be noted for their use in interventions, such as epidural steroid injections.
MeSH Terms
Figure
Cited by 2 articles
-
Ultrasound-Guided Percutaneous Needle Fasciotomy after Steroid Injection for Dupuytren's Contracture
Jae-Sung Yoo, Kang Heo, Seong-Jun Kim, Kwang-Hee Park, Jong-Pil Kim
Arch Hand Microsurg. 2018;23(1):28-34. doi: 10.12790/ahm.2018.23.1.28.Effect of intravenous dexamethasone on the duration of postoperative analgesia for popliteal sciatic nerve block: a randomized, double-blind, placebo-controlled study
Byung-Gun Kim, Woojoo Lee, Jang Ho Song, Chunwoo Yang, Gyung A Heo, Hongseok Kim
Korean J Anesthesiol. 2021;74(4):317-324. doi: 10.4097/kja.20640.
Reference
-
1. Derby R, Lee SH, Date ES, Lee JH, Lee CH. Size and aggregation of corticosteroids used for epidural injections. Pain Med. 2008; 9:227–234. PMID: 18298706.
Article2. MacMahon PJ, Shelly MJ, Scholz D, Eustace SJ, Kavanagh EC. Injectable corticosteroid preparations: an embolic risk assessment by static and dynamic microscopic analysis. AJNR Am J Neuroradiol. 2011; 32:1830–1835. PMID: 21940803.
Article3. Benzon HT, Chew TL, McCarthy RJ, Benzon HA, Walega DR. Comparison of the particle sizes of different steroids and the effect of dilution: a review of the relative neurotoxicities of the steroids. Anesthesiology. 2007; 106:331–338. PMID: 17264728.4. Gharibo C, Koo C, Chung J, Moroz A. Epidural steroid injections: an update on mechanisms of injury and safety. Tech Reg Anesth Pain Manag. 2009; 13:266–271.
Article5. Manchikanti L, Falco FJ, Benyamin RM, Gharibo CG, Candido KD, Hirsch JA. Epidural steroid injections safety recommendations by the Multi-Society Pain Workgroup (MPW): more regulations without evidence or clarification. Pain Physician. 2014; 17:E575–E588. PMID: 25247907.6. Rodriguez RW. How safe is epidural steroid injection? Examining drug-related factors. Pract Pain Manag. 2014; 14:31–35.7. McLure HA, Rubin AP. Review of local anaesthetic agents. Minerva Anestesiol. 2005; 71:59–74. PMID: 15714182.8. Brandis K. Alkalinisation of local anaesthetic solutions. Aust Prescr. 2011; 34:173–175.
Article9. Milner QJ, Guard BC, Allen JG. Alkalinization of amide local anaesthetics by addition of 1% sodium bicarbonate solution. Eur J Anaesthesiol. 2000; 17:38–42. PMID: 10758442.
Article10. Chassard D, Berrada K, Bouletreau P. Alkalinization of local anesthetics: theoretically justified but clinically useless. Can J Anaesth. 1996; 43:384–393. PMID: 8697555.11. Peterfreund RA, Datta S, Ostheimer GW. pH adjustment of local anesthetic solutions with sodium bicarbonate: laboratory evaluation of alkalinization and precipitation. Reg Anesth. 1989; 14:265–270. PMID: 2562097.12. Fulling PD, Peterfreund RA. Alkalinization and precipitation characteristics of 0.2% ropivacaine. Reg Anesth Pain Med. 2000; 25:518–521. PMID: 11009239.
Article13. Schmidt AC. The role of molecular structure in the crystal polymorphism of local anesthetic drugs: crystal polymorphism of local anesthetic drugs, part X. Pharm Res. 2005; 22:2121–2133. PMID: 16283568.
Article14. Koitabashi T, Sekiguchi H, Miyao H, Kawasaki J, Kawazoe T. Precipitation of pH-adjusted local anesthetics with sodium bicarbonate. Masui. 1995; 44:15–20. PMID: 7699818.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Density Change of Local Anesthetics and a Mixed Solution Can Be Estimated by Refractometry
- A Study for Reducing Pain from Injection of Lidocaine Hydrochloride
- Mechanism of Action of Local Anesthetics
- The use of adjuvants to local anesthetics: benefit and risk
- Direct Effects of Ester - Type Local Anesthetics on Isolated Rat Left Ventricular Papillary Muscles