J Korean Soc Radiol.
2016 Jan;74(1):55-60. 10.3348/jksr.2016.74.1.55.
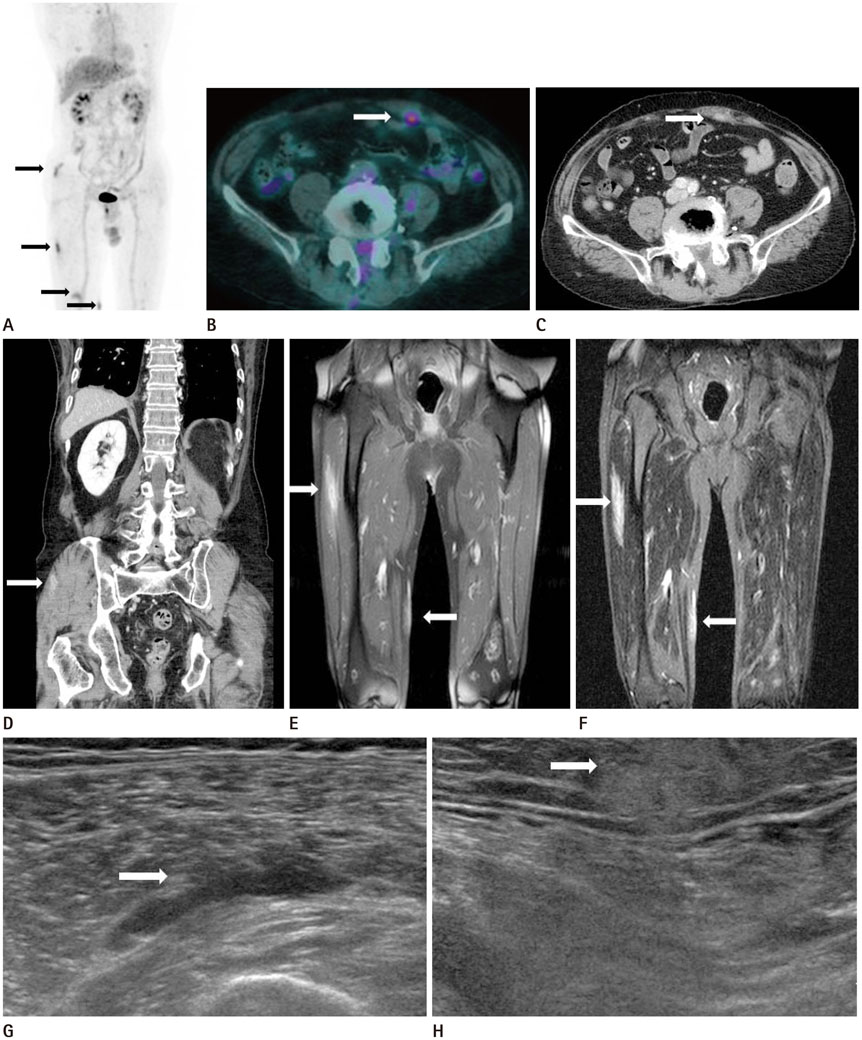
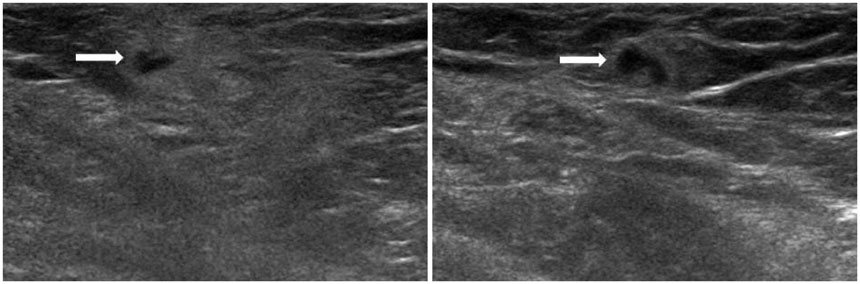
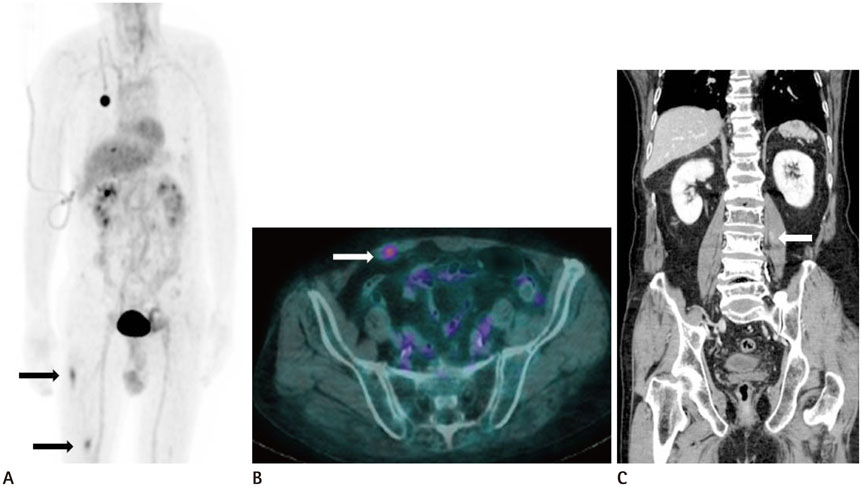
Multifocal Sparganosis Mimicking Lymphoma Involvement: Multimodal Imaging Findings of Ultrasonography, CT, MRI, and Positron Emission Tomography-Computed Tomography
- Affiliations
-
- 1Department of Radiology, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea. zzzz3@hanmail.net
- 2Department of Pathology, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea.
- 3Division of Hematology-Oncology, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 4Division of Hematology-Oncology, Department of Internal Medicine, Seoul Medical Center, Seoul, Korea.
- KMID: 2150463
- DOI: http://doi.org/10.3348/jksr.2016.74.1.55
Abstract
- Sparganosis is a rare parasitic disease caused by the migrating plerocercoid larva of Spirometra species tapeworms. The most frequent clinical manifestation is a subcutaneous nodule resembling a neoplasm. In this study, we presented multimodal findings of ultrasonography, computed tomography, magnetic resonance imaging, positron emission tomography-computed tomography and follow-up imagings on multifocal sparganosis, mimicking lymphoma involvement in a patient with lymphoma.
MeSH Terms
Figure
Reference
-
1. Lee BJ, Ahn SK, Kim SC, Lee SH. Clinical and histopathologic study of sparganosis. Korean J Dermatol. 1992; 30:168–174.2. Roh SY, Lee JY, Park KW, Jung SN. Sparganosis in a patient with diffuse large B cell lymphoma. J Cancer Res Ther. 2013; 9:712–714.3. Lee EK, Yoo YB. Axillary sparganosis which was misunderstood lymph node metastasis during neoadjuvant chemotheraphy in a breast cancer patient. Ann Surg Treat Res. 2014; 87:336–339.4. Kim JI, Kim TW, Hong SM, Moon TY, Lee IS, Choi KU, et al. Intramuscular sparganosis in the gastrocnemius muscle: a case report. Korean J Parasitol. 2014; 52:69–73.5. Park HJ, Park NH, Lee EJ, Park CS, Lee SM, Park SI. Ultrasonographic Findings of Subcutaneous and Muscular Sparganosis. J Korean Soc Radiol. 2009; 61:183–187.6. Hung GD, Chen YH, Chen DY, Lan JL. Subcutaneous panniculitis-like T-cell lymphoma presenting with hemophagocytic lymphohistiocytosis and skin lesions with characteristic high-resolution ultrasonographic findings. Clin Rheumatol. 2007; 26:775–778.7. Kim YH, Kim HS, Kim SY, Hwang YJ, Seo JW, Lee JY, et al. MR findings of subcutaneous panniculitis-like T-cell lymphoma: a case report. J Korean Radiol Soc. 2007; 57:479–482.8. Song T, Wang WS, Zhou BR, Mai WW, Li ZZ, Guo HC, et al. CT and MR characteristics of cerebral sparganosis. AJNR Am J Neuroradiol. 2007; 28:1700–1705.9. Tsai MD, Chang CN, Ho YS, Wang AD. Cerebral sparganosis diagnosed and treated with stereotactic techniques. Report of two cases. J Neurosurg. 1993; 78:129–113.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diffuse Large B-Cell Lymphoma in the Era of Precision Oncology: How Imaging Is Helpful
- Follicular Lymphoma mimicking Metastatic Nodes on the F-18 FDG PET/CT and MRI for Staging of Endometrial Cancer
- CT, Magnetic Resonance, and 18F-Fluorodeoxyglucose Positron Emission Tomography/CT Imaging Features of Mucosa-Associated Lymphoid Tissue Lymphoma Involving Medial Rectus Muscle: A Case Report
- Positron Emission Tomography-CT, CT, and MR Imaging Findings of Tumor-Mimicking Organized Hematoma in the Maxillary Sinus: Two Case Reports
- A Case of Recurrence-Mimicking Charcoal Granuloma in a Breast Cancer Patient: Ultrasound, CT, PET/CT and Breast-Specific Gamma Imaging Findings