Cancer Res Treat.
2015 Jul;47(3):379-386. 10.4143/crt.2014.021.
A Survey of Stereotactic Body Radiotherapy in Korea
- Affiliations
-
- 1Department of Radiation Oncology, Soonchunhyang University College of Medicine, Bucheon, Korea.
- 2Department of Radiation Oncology, Korea Institute of Radiological and Medical Sciences, Seoul, Korea. mskim@kcch.re.kr
- 3Department of Radiation Oncology, Incheon St. Mary's Hospital, The Catholic University of Korea, Incheon, Korea.
- 4Department of Radiation Oncology, Inha University Hospital, Inha University School of Medicine, Incheon, Korea.
- 5Department of Radiation Oncology, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 6Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea.
- 7Department of Radiation Oncology, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- 8Department of Radiation Oncology, Dongnam Institute of Radiological and Medical Sciences, Busan, Korea.
- 9Department of Radiation Oncology, Gachon University Gil Medical Center, Gachon University of Medicine and Science, Incheon, Korea.
- 10Department of Radiation Oncology, Soonchunhyang University College of Medicine, Seoul, Korea.
- 11Department of Radiation Oncology, Haeundae Paik Hospital, Inje University School of Medicine, Busan, Korea.
- KMID: 2148486
- DOI: http://doi.org/10.4143/crt.2014.021
Abstract
- PURPOSE
The purpose of this study is to investigate the current status of stereotactic body radiotherapy (SBRT) in Korea. A nationwide survey was conducted by the Korean Stereotactic Radiosurgery Group of the Korean Society for Radiation Oncology (KROG 13-13).
MATERIALS AND METHODS
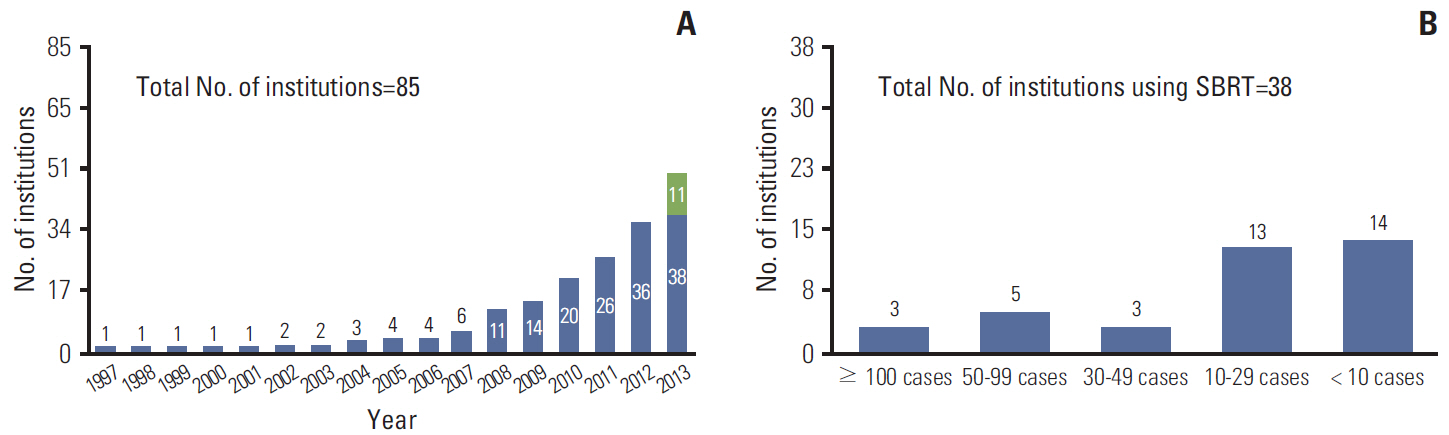
SBRT was defined as radiotherapy with delivery of a high dose of radiation to an extracranial lesion in < or = 4 fractions. A 16-questionnaire survey was sent by e-mail to the chief of radiation oncology at 85 institutions in June 2013.
RESULTS
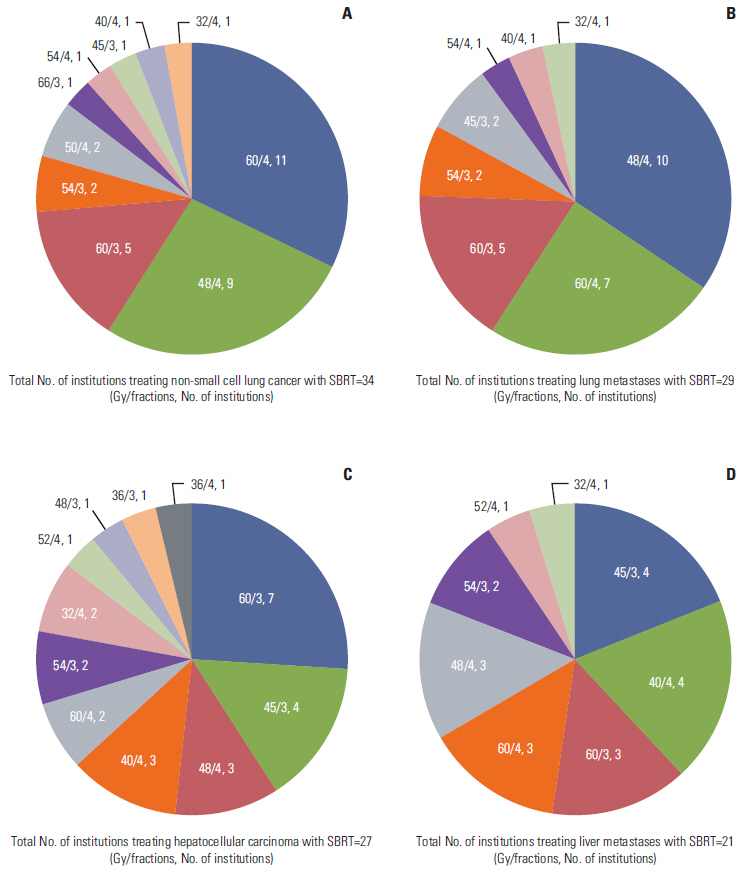
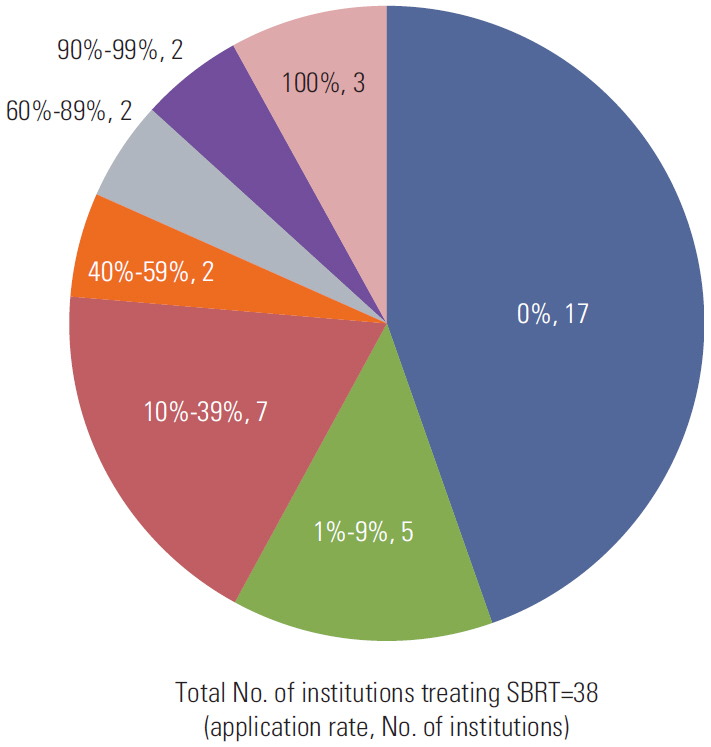
All institutions (100%) responded to this survey. Of these, 38 institutions (45%) have used SBRT and 47 institutions (55%) have not used SBRT. Regarding the treatment site, the lung (92%) and liver (76%) were the two most common sites. The most common schedules were 60 Gy/4 fractions for non-small cell lung cancer, 48 Gy/4 fractions for lung metastases, 60 Gy/3 fractions for hepatocellular carcinoma, and 45 Gy/3 fractions or 40 Gy/4 fractions for liver metastases. Four-dimensional computed tomography (CT) was the most common method for planning CT (74%). During planning CT, the most common method of immobilization was the use of an alpha cradle/vacuum-lock (42%).
CONCLUSION
Based on this survey, conduct of further prospective studies will be needed in order to determine the appropriate prescribed doses and to standardize the practice of SBRT.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Practice Patterns of Radiotherapy in Patients with Hepatocellular Carcinoma: A Korean Radiation Oncology Group Study (KROG 14-07)
Hyejung Cha, Hee Chul Park, Jeong Il Yu, Tae Hyun Kim, Taek-Keun Nam, Sang Min Yoon, Won Sup Yoon, Jun Won Kim, Mi Sook Kim, Hong Seok Jang, Youngmin Choi, Jin Hee Kim, Chul Seung Kay, Inkyung Jung, Jinsil Seong
Cancer Res Treat. 2017;49(1):61-69. doi: 10.4143/crt.2016.097.
Reference
-
References
1. Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand. 1951; 102:316–9.2. Tipton K, Launders JH, Inamdar R, Miyamoto C, Schoelles K. Stereotactic body radiation therapy: scope of the literature. Ann Intern Med. 2011; 154:737–45.3. Potters L, Steinberg M, Rose C, Timmerman R, Ryu S, Hevezi JM, et al. American Society for Therapeutic Radiology and Oncology and American College of Radiology practice guideline for the performance of stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2004; 60:1026–32.4. Khrizman P, Small W Jr, Dawson L, Benson AB 3rd. The use of stereotactic body radiation therapy in gastrointestinal malignancies in locally advanced and metastatic settings. Clin Colorectal Cancer. 2010; 9:136–43.5. Nagata Y, Hiraoka M, Mizowaki T, Narita Y, Matsuo Y, Norihisa Y, et al. Survey of stereotactic body radiation therapy in Japan by the Japan 3-D Conformal External Beam Radiotherapy Group. Int J Radiat Oncol Biol Phys. 2009; 75:343–7.6. Pan H, Simpson DR, Mell LK, Mundt AJ, Lawson JD. A survey of stereotactic body radiotherapy use in the United States. Cancer. 2011; 117:4566–72.7. Lock MI, Hoyer M, Bydder SA, Okunieff P, Hahn CA, Vichare A, et al. An international survey on liver metastases radiotherapy. Acta Oncol. 2012; 51:568–74.8. Daly ME, Perks JR, Chen AM. Patterns-of-care for thoracic stereotactic body radiotherapy among practicing radiation oncologists in the United States. J Thorac Oncol. 2013; 8:202–7.9. Guckenberger M, Allgauer M, Appold S, Dieckmann K, Ernst I, Ganswindt U, et al. Safety and efficacy of stereotactic body radiotherapy for stage 1 non-small-cell lung cancer in routine clinical practice: a patterns-of-care and outcome analysis. J Thorac Oncol. 2013; 8:1050–8.10. Onishi H, Araki T, Shirato H, Nagata Y, Hiraoka M, Gomi K, et al. Stereotactic hypofractionated high-dose irradiation for stage I nonsmall cell lung carcinoma: clinical outcomes in 245 subjects in a Japanese multiinstitutional study. Cancer. 2004; 101:1623–31.11. Zhang J, Yang F, Li B, Li H, Liu J, Huang W, et al. Which is the optimal biologically effective dose of stereotactic body radiotherapy for Stage I non-small-cell lung cancer? A meta-analysis. Int J Radiat Oncol Biol Phys. 2011; 81:e305–16.12. Grills IS, Hope AJ, Guckenberger M, Kestin LL, Werner-Wasik M, Yan D, et al. A collaborative analysis of stereotactic lung radiotherapy outcomes for early-stage non-small-cell lung cancer using daily online cone-beam computed tomography image-guided radiotherapy. J Thorac Oncol. 2012; 7:1382–93.13. Wigg AJ, Palumbo K, Wigg DR. Radiotherapy for hepatocellular carcinoma: systematic review of radiobiology and modeling projections indicate reconsideration of its use. J Gastroenterol Hepatol. 2010; 25:664–71.14. Dawson LA, McGinn CJ, Normolle D, Ten Haken RK, Walker S, Ensminger W, et al. Escalated focal liver radiation and concurrent hepatic artery fluorodeoxyuridine for unresectable intrahepatic malignancies. J Clin Oncol. 2000; 18:2210–8.15. Lausch A, Sinclair K, Lock M, Fisher B, Jensen N, Gaede S, et al. Determination and comparison of radiotherapy dose responses for hepatocellular carcinoma and metastatic colorectal liver tumours. Br J Radiol. 2013; 86:20130147.16. Kwon JH, Bae SH, Kim JY, Choi BO, Jang HS, Jang JW, et al. Long-term effect of stereotactic body radiation therapy for primary hepatocellular carcinoma ineligible for local ablation therapy or surgical resection. Stereotactic radiotherapy for liver cancer. BMC Cancer. 2010; 10:475.17. Louis C, Dewas S, Mirabel X, Lacornerie T, Adenis A, Bonodeau F, et al. Stereotactic radiotherapy of hepatocellular carcinoma: preliminary results. Technol Cancer Res Treat. 2010; 9:479–87.18. Huang WY, Jen YM, Lee MS, Chang LP, Chen CM, Ko KH, et al. Stereotactic body radiation therapy in recurrent hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2012; 84:355–61.19. Kang JK, Kim MS, Cho CK, Yang KM, Yoo HJ, Kim JH, et al. Stereotactic body radiation therapy for inoperable hepatocellular carcinoma as a local salvage treatment after incomplete transarterial chemoembolization. Cancer. 2012; 118:5424–31.20. Lax I, Blomgren H, Naslund I, Svanstrom R. Stereotactic radiotherapy of malignancies in the abdomen. Methodological aspects. Acta Oncol. 1994; 33:677–83.21. Li W, Purdie TG, Taremi M, Fung S, Brade A, Cho BC, et al. Effect of immobilization and performance status on intrafraction motion for stereotactic lung radiotherapy: analysis of 133 patients. Int J Radiat Oncol Biol Phys. 2011; 81:1568–75.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stereotactic Body Radiotherapy for Early Stage Lung Cancer
- The mixed era of stereotactic radiosurgery and radiotherapy
- Current status of stereotactic body radiotherapy for the treatment of hepatocellular carcinoma
- Stereotactic body radiotherapy for solitary spine metastasis
- Stereotactic radiotherapy for early stage non-small cell lung cancer