Korean Circ J.
2014 May;44(3):148-155. 10.4070/kcj.2014.44.3.148.
Clinical Outcomes in Patients with Intermediate Coronary Stenoses: MINIATURE Investigators (Korea MultIceNter TrIal on Long-Term Clinical Outcome According to the Plaque Burden and Treatment Strategy in Lesions with MinimUm Lumen ARea lEss Than 4 mm2 Using Intravascular Ultrasound)
- Affiliations
-
- 1Division of Cardiology, Chonnam National University School of Medicine, Gwangju, Korea. myungho@chollian.net
- 2Division of Cardiology, Keimyung University College of Medicine, Dongsan Medical Center, Daegu, Korea.
- 3Division of Cardiology, Saint Carollo Hospital, Suncheon, Korea.
- 4Division of Cardiology, Gwangju Veterans Hospital, Gwangju, Korea.
- 5Division of Cardiology, Chonbuk National University College of Medicine, Jeonju, Korea.
- 6Division of Cardiology, Inje University College of Medicine, Ilsan Paik Hospital, Goyang, Korea.
- 7Division of Cardiology, Chung-Ang University College of Medicine, Seoul, Korea.
- 8Division of Cardiology, Korea University College of Medicine, Ansan Hospital, Ansan, Korea.
- 9Division of Cardiology, Wonkwang University College of Medicine, Iksan, Korea.
- 10Division of Cardiology, Yonsei University College of Medicine, Severance Hospital, Seoul, Korea.
- 11Division of Cardiology, Korea University Guro Hospital, Seoul, Korea.
- 12Division of Cardiology, Gachon University Gil Medical Center, Incheon, Korea.
- 13Division of Cardiology, Jeju National University College of Medicine, Jeju, Korea.
- 14Division of Cardiology, Samsung Medical Center, Seoul, Korea.
- 15Division of Cardiology, Chosun University College of Medicine, Gwangju, Korea.
- 16Division of Cardiology, KyungHee University Medical Center, Seoul, Korea.
- KMID: 2145475
- DOI: http://doi.org/10.4070/kcj.2014.44.3.148
Abstract
- BACKGROUND AND OBJECTIVES
We evaluated the two-year clinical outcomes in patients with angiographically intermediate lesions according to the plaque burden and treatment strategy.
SUBJECTS AND METHODS
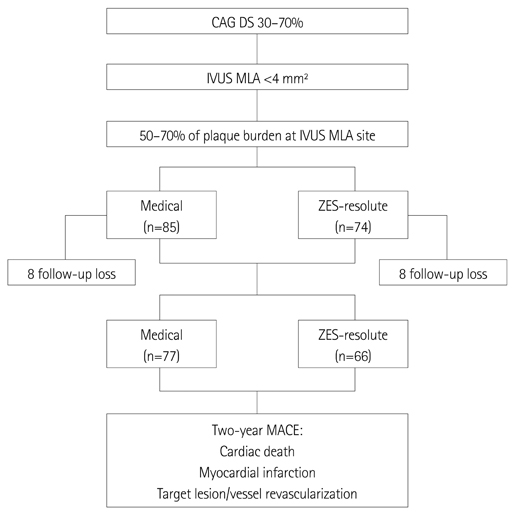
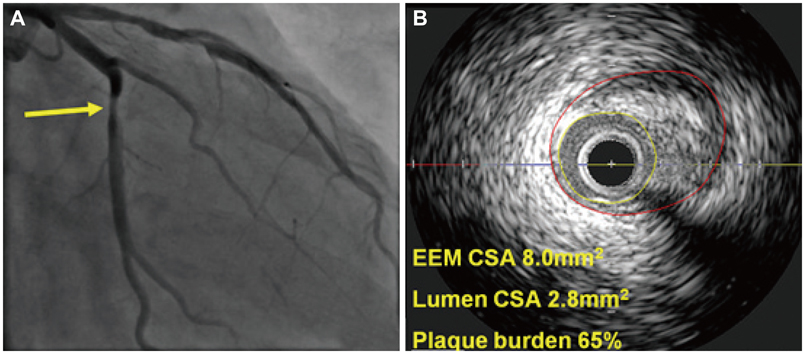
We prospectively enrolled patients with angiographically intermediate lesions (diameter stenosis 30-70%) with an intravascular ultrasound (IVUS) minimum lumen area (MLA) <4 mm2 with 50-70% plaque burden of 16 Korean percutaneous coronary intervention centers. Patients were divided into medical therapy group (n=85) and zotarolimus-eluting stent group (ZES; Resolute) group (n=74). We evaluated the incidences of two-year major adverse cardiovascular events (MACE).
RESULTS
A two-year clinical follow-up was completed in 143 patients and MACE occurred in 12 patients. There were no significant differences in the incidences of death (1.3% vs. 3.0%, p=0.471), target vessel-related non-fatal myocardial infarction (0.0% vs. 0.0%, p=1.000) and target vessel revascularizations (7.8% vs. 4.5%, p=0.425) between medical and ZES groups. Independent predictors of two-year MACE included acute myocardial infarction {odds ratio (OR)=2.87; 95% confidence interval (CI) 1.43-6.12, p=0.014}, diabetes mellitus (OR=2.46; 95% CI 1.24-5.56, p=0.028) and non-statin therapy (OR=2.32; 95% CI 1.18-5.24, p=0.034).
CONCLUSION
Medical therapy shows comparable results with ZES, and myocardial infarction, diabetes mellitus and non-statin therapy were associated with the occurrence of two-year MACE in patients with intermediate lesion with IVUS MLA <4 mm2 with 50-70% of plaque burden.
MeSH Terms
Figure
Reference
-
1. Briguori C, Anzuini A, Airoldi F, et al. Intravascular ultrasound criteria for the assessment of the functional significance of intermediate coronary artery stenoses and comparison with fractional flow reserve. Am J Cardiol. 2001; 87:136–141.2. Tobis J, Azarbal B, Slavin L. Assessment of intermediate severity coronary lesions in the catheterization laboratory. J Am Coll Cardiol. 2007; 49:839–848.3. Abizaid A, Mintz GS, Pichard AD, et al. Clinical, intravascular ultrasound, and quantitative angiographic determinants of the coronary flow reserve before and after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1998; 82:423–428.4. Pijls NH, Van Gelder B, Van der Voort P, et al. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995; 92:3183–3193.5. Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996; 334:1703–1708.6. Baumgart D, Haude M, Goerge G, et al. Improved assessment of coronary stenosis severity using the relative flow velocity reserve. Circulation. 1998; 98:40–46.7. Ahn JM, Kang SJ, Mintz GS, et al. Validation of minimal luminal area measured by intravascular ultrasound for assessment of functionally significant coronary stenosis comparison with myocardial perfusion imaging. JACC Cardiovasc Interv. 2011; 4:665–671.8. Koo BK, Yang HM, Doh JH, et al. Optimal intravascular ultrasound criteria and their accuracy for defining the functional significance of intermediate coronary stenoses of different locations. JACC Cardiovasc Interv. 2011; 4:803–811.9. Kang SJ, Lee JY, Ahn JM, et al. Intravascular ultrasound-derived predictors for fractional flow reserve in intermediate left main disease. JACC Cardiovasc Interv. 2011; 4:1168–1174.10. Dhawan J, Bray CL. Are Asian coronary arteries smaller than Caucasian? A study on angiographic coronary artery size estimation during life. Int J Cardiol. 1995; 49:267–269.11. Lip GY, Rathore VS, Katira R, Watson RD, Singh SP. Do Indo-Asians have smaller coronary arteries? Postgrad Med J. 1999; 75:463–466.12. Effects of tissue plasminogen activator and a comparison of early invasive and conservative strategies in unstable angina and non-Q-wave myocardial infarction. Results of the TIMI IIIB Trial. Thrombolysis in Myocardial Ischemia. Circulation. 1994; 89:1545–1556.13. Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001; 37:1478–1492.14. Stone GW, Maehara A, Lansky AJ, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011; 364:226–235.15. Nicholls SJ, Tuzcu EM, Kalidindi S, et al. Effect of diabetes on progression of coronary atherosclerosis and arterial remodeling: a pooled analysis of 5 intravascular ultrasound trials. J Am Coll Cardiol. 2008; 52:255–262.16. Boyle PJ. Diabetes mellitus and macrovascular disease: mechanisms and mediators. Am J Med. 2007; 120:9 Suppl 2. S12–S17.17. Takayama T, Hiro T, Ueda Y, et al. Plaque stabilization by intensive LDL-cholesterol lowering therapy with atorvastatin is delayed in type 2 diabetic patients with coronary artery disease-Serial angioscopic and intravascular ultrasound analysis. J Cardiol. 2013; 61:381–386.18. Stancoven A, McGuire DK. Preventing macrovascular complications in type 2 diabetes mellitus: glucose control and beyond. Am J Cardiol. 2007; 99(11A):5H–11H.19. Nissen SE, Tuzcu EM, Schoenhagen P, et al. Statin therapy, LDL cholesterol, C-reactive protein, and coronary artery disease. N Engl J Med. 2005; 352:29–38.20. Nissen SE, Nicholls SJ, Sipahi I, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA. 2006; 295:1556–1565.21. Nicholls SJ, Tuzcu EM, Sipahi I, et al. Statins, high-density lipoprotein cholesterol, and regression of coronary atherosclerosis. JAMA. 2007; 297:499–508.22. Hong YJ, Jeong MH, Ahn Y, et al. Effect of pitavastatin treatment on changes of plaque volume and composition according to the reduction of high-sensitivity C-reactive protein levels. J Cardiol. 2012; 60:277–282.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors of Angiographic Restenosis after Intracoronary Stenting according to Stent Lumen Cross Sectional Area and Stent Length in Native Coronary Artery Lesions: An Intravascular Ultrasound Study
- Lesion Characteristics in Patients with Acute Coronary Syndrome: A Comparison with Lesion in Patients with Stable Angina by Intravascular Ultrasound
- Predictors of Clinical Outcome in Patients with Angiographically Intermediate Lesions with Minimum Lumen Area Less than 4 mm² Using Intravascular Ultrasound in Non-Proximal Epicardial Coronary Artery
- Long-term Outcome of Minor Plaque Prolapsed within Stents Documented with Intravascular Ultrasound
- Roles of Intravascular Ultrasound in Patients with Acute Myocardial Infarction