J Cardiovasc Ultrasound.
2015 Mar;23(1):32-35. 10.4250/jcu.2015.23.1.32.
Persistent Truncus Arteriosus with Aortic Dominance in Female Adult Patient
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea.
- 2Department of Pediatrics, Kyungpook National University School of Medicine, Daegu, Korea. kimyhmd@knu.ac.kr
- KMID: 2135404
- DOI: http://doi.org/10.4250/jcu.2015.23.1.32
Abstract
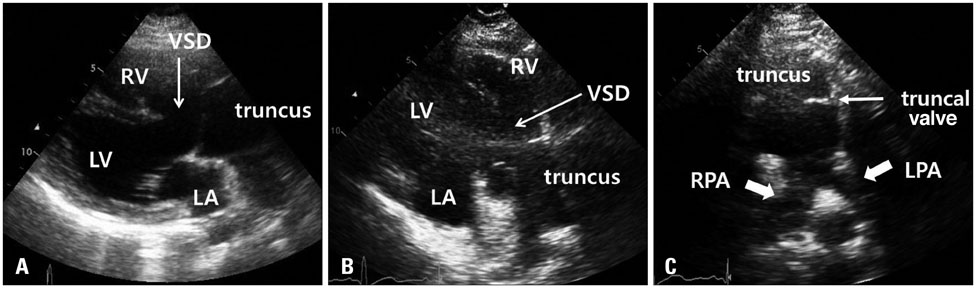
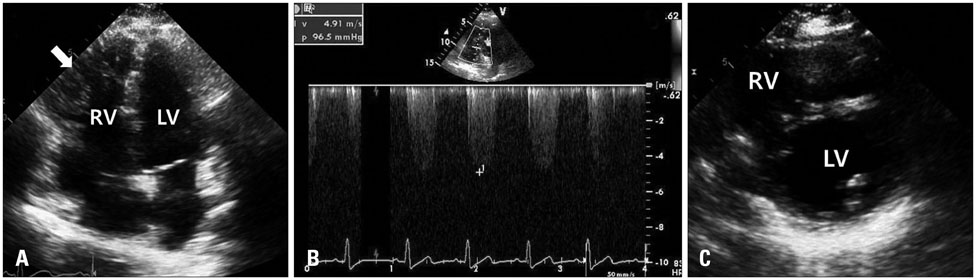
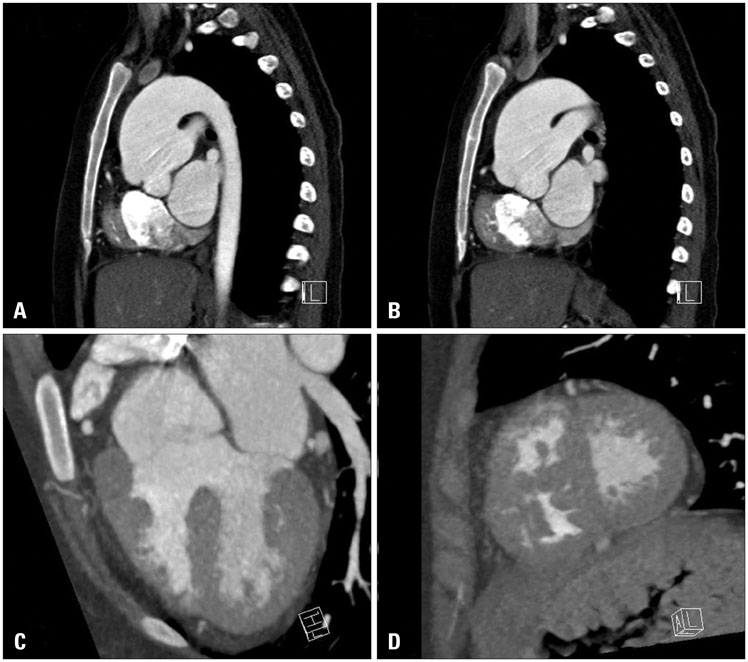
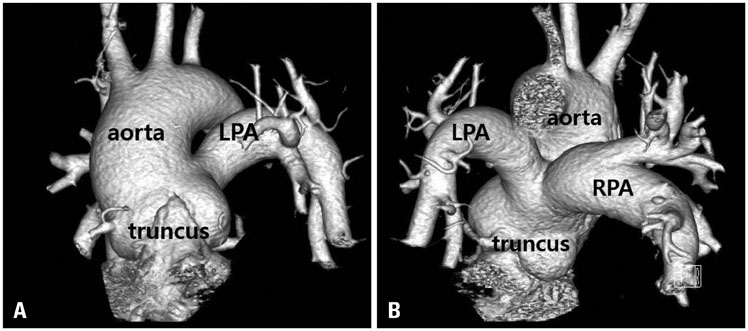
- Persistent truncus arteriosus categories associated with different natural histories and various surgical approaches were reported. Although pulmonary overflow and severe heart failure are common, some patients who have hypoplastic pulmonary artery systems may show lesser symptoms of heart failure and remain in relatively stable condition. We experienced a 33-year-old woman with uncorrected type II persistent truncus arteriosus who presented with cyanosis rather than congestive heart failure, and are presenting her images.
Keyword
MeSH Terms
Figure
Reference
-
1. Slavik Z, Keeton BR, Salmon AP, Sutherland GR, Fong LV, Monro JL. Persistent truncus arteriosus operated during infancy: long-term follow-up. Pediatr Cardiol. 1994; 15:112–115.2. Bodí V, Insa L, Sanchis J, Ibáñez M, Losada A, Chorro FJ. Persistent truncus arteriosus type 4 with survival to the age of 54 years. Int J Cardiol. 2002; 82:75–77.3. Hicken P, Evans D, Heath D. Persistent truncus arteriosus with survival to the age of 38 years. Br Heart J. 1966; 28:284–286.4. Guenther F, Frydrychowicz A, Bode C, Geibel A. Cardiovascular flashlight. Persistent truncus arteriosus: a rare finding in adults. Eur Heart J. 2009; 30:1154.5. Espínola-Zavaleta N, Muñoz-Castellanos L, González-Flores R, Kuri-Nivón M. [Common truncus arteriosus in adults]. Arch Cardiol Mex. 2008; 78:210–216.6. Russell HM, Jacobs ML, Anderson RH, Mavroudis C, Spicer D, Corcrain E, Backer CL. A simplified categorization for common arterial trunk. J Thorac Cardiovasc Surg. 2011; 141:645–653.7. Marcelletti C, McGoon DC, Mair DD. The natural history of truncus arteriosus. Circulation. 1976; 54:108–111.8. Boris JR. Primary care management of patients with common arterial trunk and transposition of the great arteries. Cardiol Young. 2012; 22:761–767.