Brain Tumor Res Treat.
2014 Oct;2(2):102-107. 10.14791/btrt.2014.2.2.102.
Procarbazine, CCNU, and Vincristine Chemotherapy in Gliomatosis Cerebri
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Inje University, Busan Paik Hospital, Busan, Korea. auferstehung@hanmail.net
- KMID: 2134280
- DOI: http://doi.org/10.14791/btrt.2014.2.2.102
Abstract
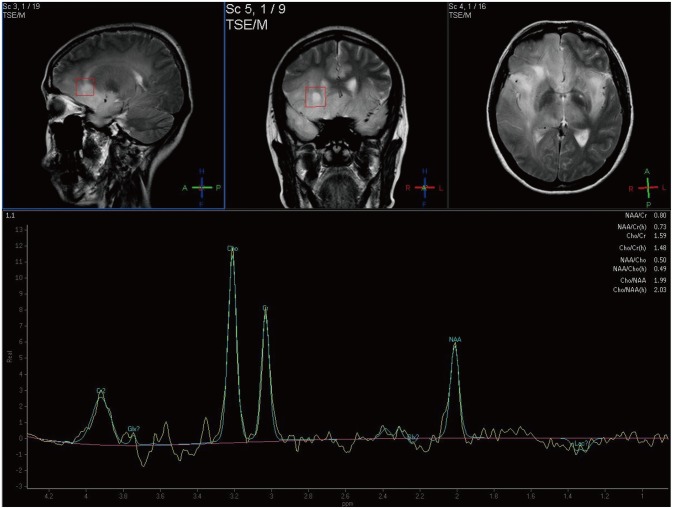
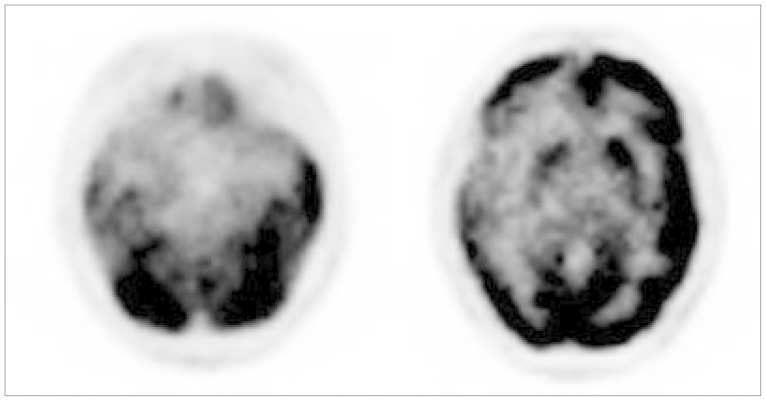
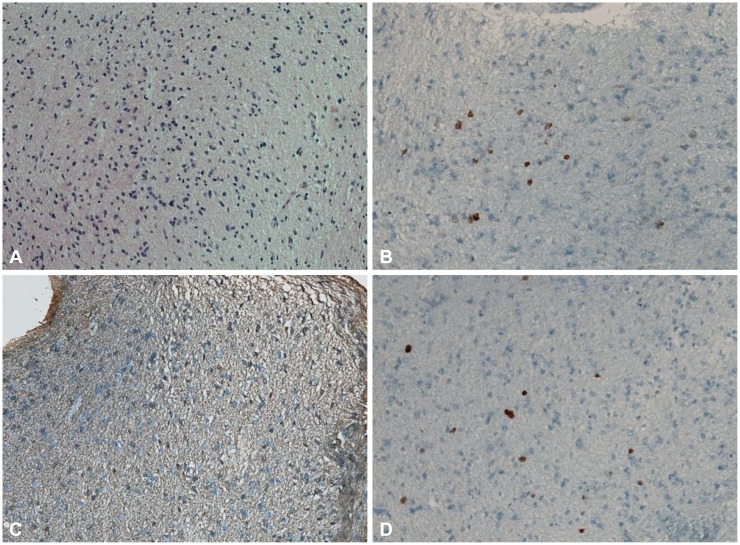
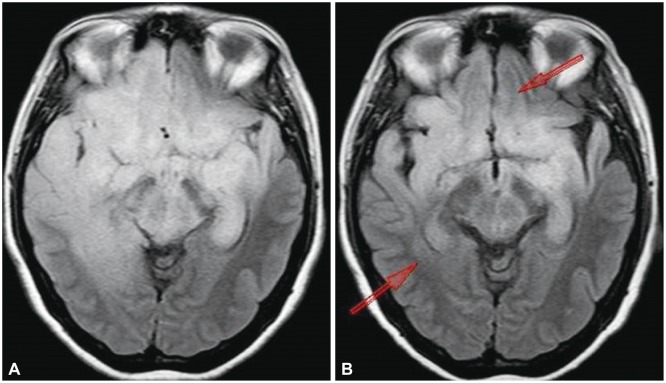
- A 49-year-old female patient was admitted due to memory disturbances. Magnetic resonance (MR) imaging suggested gliomatosis cerebri (GC), which had spread to both insular lobes, both frontal and basal ganglia and the brain stem. A stereotactic biopsy was performed at the high signal intensity area of the T2-weighted MR image, and the revealed a diffuse astrocytoma. Radiation therapy was judged not to be an appropriate treatment for the patient because of her cognitive impairment. A combinatorial chemotherapy regiment consisting of Procarbazine, CCNU, and Vincristine (PCV) was agreed upon after discussion. The patient underwent six cycles of PCV chemotherapy (a full dose was applied until the 3rd cycle, and dose then was reduced to 75% for the remaining cycles). Although the patient exhibited side effects such as bone marrow suppression and gastrointestinal symptoms, these were managed by medication. Over the 28 months following initiation of treatment, the high signal area in the right frontal and temporal lobes in the T2-weighted MR image decreased, and the patient's cognitive function [global deterioration scale (GDS) 4 points, mini-mental state examination (MMSE) 25 point] also improved (GDS 1 points, MMSE 29 points). PCV chemotherapy can therefore be an alternative therapeutic option for patients with GC who cannot be treated with radiation therapy or other chemotherapies.
Keyword
MeSH Terms
Figure
Reference
-
1. Kleihues P, Cavenee WK. World Health Organization classification of tumours. Pathology and genetics of tumours of the central nervous system. Lyon: IARC Press;2000.2. Nevin S. Gliomatosis cerebri. Brain. 1938; 61:170–191.
Article3. Kleihues P, Burger PC, Scheithauer BW. The new WHO classification of brain tumours. Brain Pathol. 1993; 3:255–268. PMID: 8293185.
Article4. Crossen JR, Garwood D, Glatstein E, Neuwelt EA. Neurobehavioral sequelae of cranial irradiation in adults: a review of radiation-induced encephalopathy. J Clin Oncol. 1994; 12:627–642. PMID: 8120563.
Article5. Imperato JP, Paleologos NA, Vick NA. Effects of treatment on long-term survivors with malignant astrocytomas. Ann Neurol. 1990; 28:818–822. PMID: 2178330.
Article6. Sanson M, Cartalat-Carel S, Taillibert S, et al. Initial chemotherapy in gliomatosis cerebri. Neurology. 2004; 63:270–275. PMID: 15277619.
Article7. Herrlinger U, Felsberg J, Küker W, et al. Gliomatosis cerebri: molecular pathology and clinical course. Ann Neurol. 2002; 52:390–399. PMID: 12325066.
Article8. Taillibert S, Chodkiewicz C, Laigle-Donadey F, Napolitano M, Cartalat-Carel S, Sanson M. Gliomatosis cerebri: a review of 296 cases from the ANOCEF database and the literature. J Neurooncol. 2006; 76:201–205. PMID: 16200347.
Article9. Chen S, Tanaka S, Giannini C, et al. Gliomatosis cerebri: clinical characteristics, management, and outcomes. J Neurooncol. 2013; 112:267–275. PMID: 23341100.
Article10. Seol HJ, Jung HW, Kim DG, Hwang SK, Yang HJ, Kim MK. Gliomatosis cerebri: clinical features and prognostic factors of long-term survival. J Korean Neurosurg Soc. 2002; 32:125–130.11. Romero FJ, Ortega A, Titus F, Ibarra B, Navarro C, Rovira M. Gliomatosis cerebri with formation of a glioblastoma multiform. Study and follow-up by magnetic resonance and computed tomography. J Comput Tomogr. 1988; 12:253–257. PMID: 2848658.
Article12. Shin YM, Chang KH, Han MH, et al. Gliomatosis cerebri: comparison of MR and CT features. AJR Am J Roentgenol. 1993; 161:859–862. PMID: 8372774.
Article13. Ponce P, Alvarez-Santullano MV, Otermin E, Santana MA, García Ludeña MV. Gliomatosis cerebri: findings with computed tomography and magnetic resonance imaging. Eur J Radiol. 1998; 28:226–229. PMID: 9881257.
Article14. Bendszus M, Warmuth-Metz M, Klein R, et al. MR spectroscopy in gliomatosis cerebri. AJNR Am J Neuroradiol. 2000; 21:375–380. PMID: 10696026.15. Osborn A, Blaser S, Salzman K. Diagnostic imaging: brain. 1st ed. Salt Lake City, UT: Amirsys Inc;2004. p. I–6. p. 26p. 2916. Elshaikh MA, Stevens GH, Peereboom DM, et al. Gliomatosis cerebri: treatment results with radiotherapy alone. Cancer. 2002; 95:2027–2031. PMID: 12404298.17. Levin N, Gomori JM, Siegal T. Chemotherapy as initial treatment in gliomatosis cerebri: results with temozolomide. Neurology. 2004; 63:354–356. PMID: 15277636.
Article18. Glas M, Rasch K, Wiewrodt D, Weller M, Herrlinger U. Procarbazine and CCNU as initial treatment in gliomatosis cerebri. Oncology. 2008; 75:182–185. PMID: 18841032.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Procarbazine and CCNU Chemotherapy for Recurrent Glioblastoma with MGMT Promoter Methylation
- Gliomatosis Cerebri in the Brain Stem and Unilateral Cerebellar Hemisphere: Case Report
- Combination chemotherapy with cyclophosphamide, vincristine, procarbazine, prednisolone(C-MOPP) in Hodgkin's disease
- A Case of Malignant Histiocytosis : Complete Remission with COPP Combination Chemotherapy
- A Case of Gliomatosis Cerebri with Serial MRI Findings