Korean J Urol.
2015 Mar;56(3):240-247. 10.4111/kju.2015.56.3.240.
Effect of weight reduction on the severity of lower urinary tract symptoms in obese male patients with benign prostatic hyperplasia: A randomized controlled trial
- Affiliations
-
- 1Department of Surgery, The Chinese University of Hong Kong, Hong Kong, China. ngcf@surgery.cuhk.edu.hk
- 2Department of Surgery, Prince of Wales Hospital, Hong Kong, China.
- KMID: 2133293
- DOI: http://doi.org/10.4111/kju.2015.56.3.240
Abstract
- PURPOSE
We assessed whether weight reduction is an effective intervention for the management of lower urinary tract symptoms (LUTS) and investigated the relationship between obesity and LUTS.
MATERIALS AND METHODS
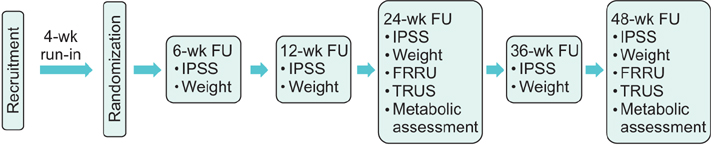
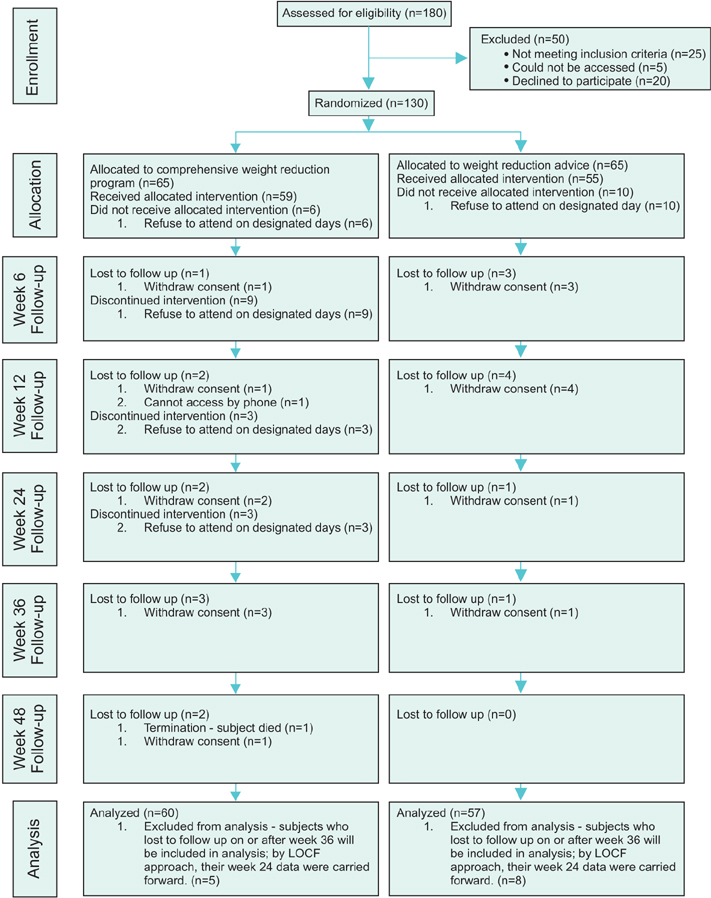
This was a prospective randomized controlled trial that enrolled obese men older than 50 years with LUTS. The study period was 52 weeks. All patients received standardized alpha-adrenergic blocker therapy for the treatment of benign prostatic hyperplasia (BPH) during the run-in period. Patients were randomized to receive either a standardized prerecorded video program on the general principle of weight reduction or a comprehensive weight reduction program. Patients were assessed at different time points with symptom assessment, uroflowmetry, transrectal ultrasound, and metabolic assessment.
RESULTS
Sixty-five patients were allocated to each study arm. After the study period, no significant difference in weight reduction was found between the two arms. When the pre- and postintervention parameters were compared, none were statistically different between the 2 arms, namely nocturia, International Prostate Symptom Score, quality of life assessment, and uroflowmetry parameters. When the whole study population was taken as a single cohort, these parameters were also not significantly different between the group with a body mass index of 25 to <30 kg/m2 and the group with a BMI of 30 to 35 kg/m2.
CONCLUSIONS
We found no association between obesity and LUTS. This could have been due to the less marked weight difference in our cohort. Whereas weight reduction may be an effective measure to improve LUTS, the implementation of a successful program remains a challenge.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Correlation between Body Mass Index and Routine Parameters in Men Over Fifty
Deok Ha Seo, Sol Yoon, Jae Hwi Choi, Jungmo Do, Sin Woo Lee, Chunwoo Lee, Seong Uk Jeh, See Min Choi, Sung Chul Kam, Jeong Seok Hwa, Ky Hyun Chung, Sung Won Kwon, Sae Chul Kim, Dong Soo Park, Jae Mann Song, Kyung Seop Lee, Jae Seog Hyun
World J Mens Health. 2017;35(3):178-185. doi: 10.5534/wjmh.16032.
Reference
-
1. Yee CH, Li JK, Lam HC, Chan ES, Hou SS, Ng CF. The prevalence of lower urinary tract symptoms in a Chinese population, and the correlation with uroflowmetry and disease perception. Int Urol Nephrol. 2014; 46:703–710.2. Bushman W. Etiology, epidemiology, and natural history of benign prostatic hyperplasia. Urol Clin North Am. 2009; 36(4):403–415.3. Parsons JK, Carter HB, Partin AW, Windham BG, Metter EJ, Ferrucci L, et al. Metabolic factors associated with benign prostatic hyperplasia. J Clin Endocrinol Metab. 2006; 91:2562–2568.4. Parsons JK, Messer K, White M, Barrett-Connor E, Bauer DC, Marshall LM, et al. Obesity increases and physical activity decreases lower urinary tract symptom risk in older men: the Osteoporotic Fractures in Men study. Eur Urol. 2011; 60:1173–1180.5. Wang S, Mao Q, Lin Y, Wu J, Wang X, Zheng X, et al. Body mass index and risk of BPH: a meta-analysis. Prostate Cancer Prostatic Dis. 2012; 15:265–272.6. St Sauver JL, Sarma AV, Hollingsworth JM, Jacobson DJ, Mc-Gree ME, Dunn RL, et al. Associations between modest weight changes and onset and progression of lower urinary tract symptoms in two population-based cohorts. Urology. 2011; 78:437–441.7. Kristal AR, Arnold KB, Schenk JM, Neuhouser ML, Weiss N, Goodman P, et al. Race/ethnicity, obesity, health related behaviors and the risk of symptomatic benign prostatic hyperplasia: results from the prostate cancer prevention trial. J Urol. 2007; 177:1395–1400.8. Mondul AM, Giovannucci E, Platz EA. A prospective study of obesity, and the incidence and progression of lower urinary tract symptoms. J Urol. 2014; 191:715–721.9. Giovannucci E, Rimm EB, Chute CG, Kawachi I, Colditz GA, Stampfer MJ, et al. Obesity and benign prostatic hyperplasia. Am J Epidemiol. 1994; 140:989–1002.10. Kok ET, Schouten BW, Bohnen AM, Groeneveld FP, Thomas S, Bosch JL. Risk factors for lower urinary tract symptoms suggestive of benign prostatic hyperplasia in a community based population of healthy aging men: the Krimpen Study. J Urol. 2009; 181:710–716.11. Wong SY, Woo J, Leung JC, Leung PC. Depressive symptoms and lifestyle factors as risk factors of lower urinary tract symptoms in Southern Chinese men: a prospective study. Aging Male. 2010; 13:113–119.12. El-Sayed AM, Scarborough P, Galea S. Ethnic inequalities in obesity among children and adults in the UK: a systematic review of the literature. Obes Rev. 2011; 12:e516–e534.13. Barte JC, ter Bogt NC, Bogers RP, Teixeira PJ, Blissmer B, Mori TA, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010; 11:899–906.14. Wadden TA, Neiberg RH, Wing RR, Clark JM, Delahanty LM, Hill JO, et al. Four-year weight losses in the Look AHEAD study: factors associated with long-term success. Obesity (Silver Spring). 2011; 19:1987–1998.15. Hunt K, Wyke S, Gray CM, Anderson AS, Brady A, Bunn C, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet. 2014; 383:1211–1221.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Trend of the Primary Treatment in Lower Urinary Tract Symptom/Benign Prostatic Hyperplasia
- A Study on Physiological Index, Anxiety and Depression by the Severity of Lower Urinary Tract Symptoms in Patients with Benign Prostatic Hyperplasia
- Benign Prostatic Hyperplasia and Sexual Dysfunction
- The Relationship between Benign Prostate Hyperplasia and Erectile Dysfunction: What is Reality?
- A Clinical Observation on Benign Prostatic Hyperplasia