Clin Exp Otorhinolaryngol.
2015 Dec;8(4):303-311. 10.3342/ceo.2015.8.4.303.
Otoacoustic Emissions in Smoking and Nonsmoking Young Adults
- Affiliations
-
- 1Institute of Physiology and Pathology of Hearing, Warsaw, Poland. w.jedrzejczak@ifps.org.pl
- 2World Hearing Center, Kajetany, Poland.
- 3Institute of Sensory Organs, Kajetany, Poland.
- KMID: 2128902
- DOI: http://doi.org/10.3342/ceo.2015.8.4.303
Abstract
OBJECTIVES
The present study investigates the usefulness of transiently evoked otoacoustic emissions (TEOAEs) and distortion product OAEs (DPOAEs) in detecting small changes in the hearing of young smoking adults.
METHODS
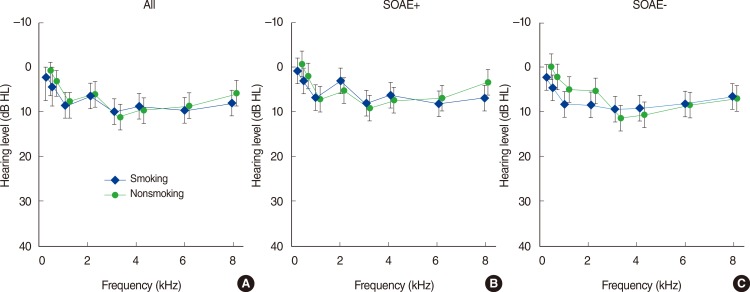
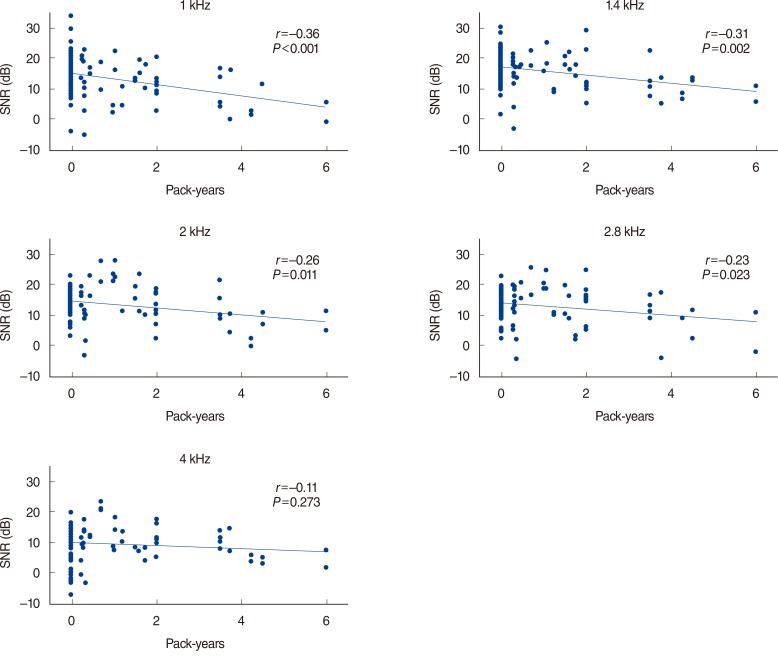
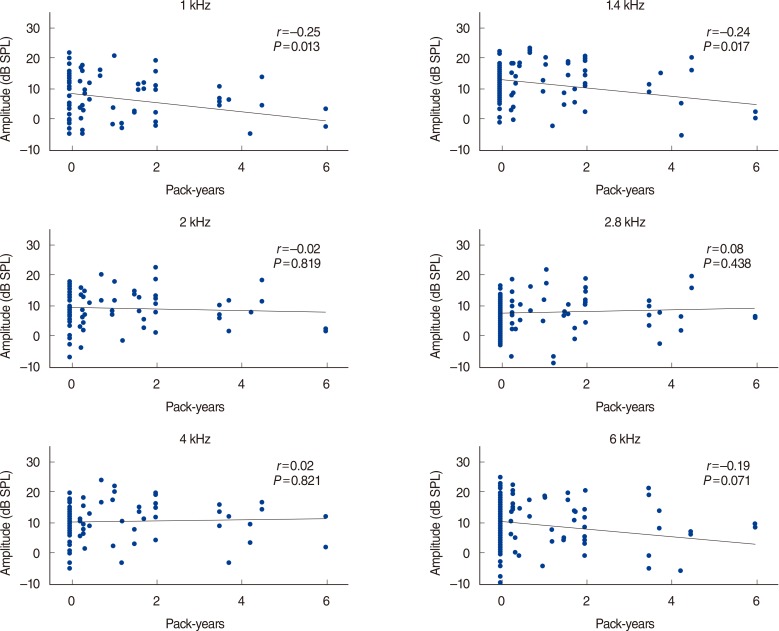
Otoacoustic emissions were acquired from the ears of 48 young adults (age, 20 to 27 years). The dataset was divided into two groups, smoking (24 persons/48 ears) and nonsmoking (24 persons/48 ears). The level of smoking was relatively small in comparison to previous studies, an average of 3.8 years and 8.7 cigarettes per day. In each ear three OAE measurements were made: TEOAEs, DPOAEs, and spontaneous OAEs (SOAEs). Pure tone audiometry and tympanometry were also conducted. Audiometric thresholds did not differ significantly between the datasets. Half-octave-band values of OAE signal to noise ratios and response levels were used to assess statistical differences.
RESULTS
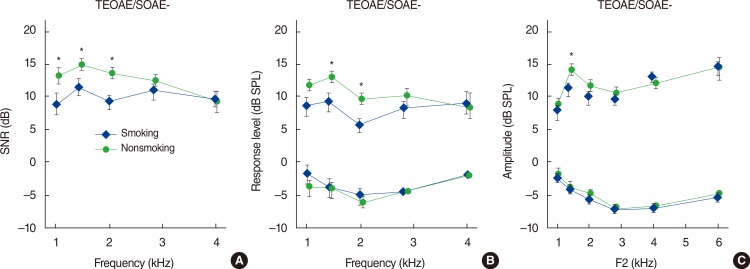
Averaged data initially revealed that differences between the two study groups occurred only for TEOAEs at 1 kHz. However when the datasets were divided into ears with and without SOAEs more differences became apparent, both for TEOAEs and DPOAEs. In ears that exhibited SOAEs, both smokers and nonsmokers, there were no statistically significant differences between evoked OAEs; however in all ears without SOAEs, evoked OAEs were higher in the ears of nonsmokers, by as much as 5 dB. These differences were most prominent in the 1-2 kHz range.
CONCLUSION
A general decrease in OAE levels was found in the group of smokers. However, in ears which exhibited SOAEs, there was no difference between the evoked OAEs of smokers and nonsmokers. We conclude that smoking had not yet measurably affected the ears of those with acute hearing (i.e., those who exhibit SOAEs). However, in ears without SOAEs, smokers exhibited smaller evoked OAE amplitudes than nonsmokers, even though their audiometric thresholds were within the norm.
MeSH Terms
Figure
Reference
-
1. Jha P, Ranson MK, Nguyen SN, Yach D. Estimates of global and regional smoking prevalence in 1995, by age and sex. Am J Public Health. 2002; 6. 92(6):1002–1006. PMID: 12036796.
Article2. Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. 2004; 5. 43(10):1731–1737. PMID: 15145091.3. Shargorodsky J, Curhan SG, Henderson E, Eavey R, Curhan GC. Heavy metals exposure and hearing loss in US adolescents. Arch Otolaryngol Head Neck Surg. 2011; 12. 137(12):1183–1189. PMID: 22183895.
Article4. Rybak LP. Hearing: the effects of chemicals. Otolaryngol Head Neck Surg. 1992; 6. 106(6):677–686. PMID: 1608633.
Article5. Cruickshanks KJ, Klein R, Klein BE, Wiley TL, Nondahl DM, Tweed TS. Cigarette smoking and hearing loss: the epidemiology of hearing loss study. JAMA. 1998; 6. 279(21):1715–1719. PMID: 9624024.6. Sharabi Y, Reshef-Haran I, Burstein M, Eldad A. Cigarette smoking and hearing loss: lessons from the young adult periodic examinations in Israel (YAPEIS) database. Isr Med Assoc J. 2002; 12. 4(12):1118–1120. PMID: 12516904.7. Fabry DA, Davila EP, Arheart KL, Serdar B, Dietz NA, Bandiera FC, et al. Secondhand smoke exposure and the risk of hearing loss. Tob Control. 2011; 1. 20(1):82–85. PMID: 21081307.
Article8. Kemp DT. Stimulated acoustic emissions from within the human auditory system. J Acoust Soc Am. 1978; 11. 64(5):1386–1391. PMID: 744838.
Article9. Probst R, Lonsbury-Martin BL, Martin GK. A review of otoacoustic emissions. J Acoust Soc Am. 1991; 5. 89(5):2027–2067. PMID: 1860995.
Article10. Jedrzejczak WW, Kochanek K, Trzaskowski B, Pilka E, Skarzynski PH, Skarzynski H. Tone-burst and click-evoked otoacoustic emissions in subjects with hearing loss above 0.25, 0.5, and 1 kHz. Ear Hear. 2012; Nov-Dec. 33(6):757–767. PMID: 22710662.
Article11. Hatzopoulos S, Di Stefano M, Albertin A, Martini A. Evaluation of cisplatin ototoxicity in a rat animal model. Ann N Y Acad Sci. 1999; 11. 884:211–225. PMID: 10842595.
Article12. Konopka W, Zalewski P, Pietkiewicz P. Evaluation of transient and distortion product otoacoustic emissions before and after shooting practice. Noise Health. 2001; 3(10):29–37. PMID: 12689453.13. Paschoal CP, Azevedo MF. Cigarette smoking as a risk factor for auditory problems. Braz J Otorhinolaryngol. 2009; Nov-Dec. 75(6):893–902. PMID: 20209294.
Article14. Vinay . Effect of smoking on transient evoked otoacoustic emissions and contralateral suppression. Auris Nasus Larynx. 2010; 6. 37(3):299–302. PMID: 19864089.
Article15. Mustafa MW. Transient evoked otoacoustic emissions and vestibular evoked myogenic potentials in cigarette and water pipe smokers. Eur Arch Otorhinolaryngol. 2014; 10. 271(10):2669–2673. PMID: 24121784.
Article16. Negley C, Katbamna B, Crumpton T, Lawson GD. Effects of cigarette smoking on distortion product otoacoustic emissions. J Am Acad Audiol. 2007; 9. 18(8):665–674. PMID: 18326153.
Article17. Durante AS, Pucci B, Gudayol N, Massa B, Gameiro M, Lopes C. Tobacco smoke exposure during childhood: effect on cochlear physiology. Int J Environ Res Public Health. 2013; 10. 10(11):5257–5265. PMID: 24284348.
Article18. Korres S, Riga M, Balatsouras D, Papadakis C, Kanellos P, Ferekidis E. Influence of smoking on developing cochlea. Does smoking during pregnancy affect the amplitudes of transient evoked otoacoustic emissions in newborns? Int J Pediatr Otorhinolaryngol. 2007; 5. 71(5):781–786. PMID: 17343925.19. Durante AS, Ibidi SM, Lotufo JP, Carvallo RM. Maternal smoking during pregnancy: impact on otoacoustic emissions in neonates. Int J Pediatr Otorhinolaryngol. 2011; 9. 75(9):1093–1098. PMID: 21719121.
Article20. Kemp DT. Evidence of mechanical nonlinearity and frequency selective wave amplification in the cochlea. Arch Otorhinolaryngol. 1979; 224(1-2):37–45. PMID: 485948.
Article21. McFadden D, Mishra R. On the relation between hearing sensitivity and otoacoustic emissions. Hear Res. 1993; 12. 71(1-2):208–213. PMID: 8113138.
Article22. Jedrzejczak WW, Bell A, Skarzynski PH, Kochanek K, Skarzynski H. Time-frequency analysis of linear and nonlinear otoacoustic emissions and removal of a short-latency stimulus artifact. J Acoust Soc Am. 2012; 3. 131(3):2200–2208. PMID: 22423716.
Article23. Jedrzejczak WW, Kochanek K, Sliwa L, Pilka E, Piotrowska A, Skarzynski H. Chirp-evoked otoacoustic emissions in children. Int J Pediatr Otorhinolaryngol. 2013; 1. 77(1):101–106. PMID: 23116905.
Article24. Kulawiec JT, Orlando MS. The contribution of spontaneous otoacoustic emissions to the click evoked otoacoustic emissions. Ear Hear. 1995; 10. 16(5):515–520. PMID: 8654906.
Article25. Smith W, Mitchell P, Leeder SR. Smoking and age-related maculopathy. The Blue Mountains Eye Study. Arch Ophthalmol. 1996; 12. 114(12):1518–1523. PMID: 8953988.26. Torre P 3rd, Dreisbach LE, Kopke R, Jackson R, Balough B. Risk factors for distortion product otoacoustic emissions in young men with normal hearing. J Am Acad Audiol. 2007; 10. 18(9):749–759. PMID: 18354884.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Valuation of Transient Evoked Otoacoustic Emissions and Distortion Product Otoacoustic Emissions in Tinnitus Patients with Normal Hearing
- Nonauditory Factors on Distortion Product Otoacoustic Emissions
- The Effect of Middle Ear Effusion on Otoacoustic Emissions
- Contralateral Suppression of Transient Evoked Otoacoustic Emission in Vestibular Neuritis
- Measurement of the spontaneous otoacoustic emission in normal hearers