J Adv Prosthodont.
2015 Apr;7(2):115-121. 10.4047/jap.2015.7.2.115.
The effect of the thread depth on the mechanical properties of the dental implant
- Affiliations
-
- 1Institute of Science & Technology, Megagen Implant, Gyeongsan, Republic of Korea.
- 2Department of Periodontology, School of Dentistry, Kyungpook National University, Daegu, Republic of Korea.
- 3MIR Dental Hospital, Daegu, Republic of Korea. periopkb@hanmail.net
- KMID: 2118241
- DOI: http://doi.org/10.4047/jap.2015.7.2.115
Abstract
- PURPOSE
This study aimed to evaluate the effect of implant thread depth on primary stability in low density bone.
MATERIALS AND METHODS
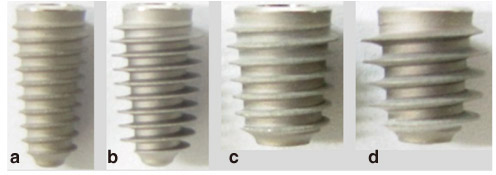
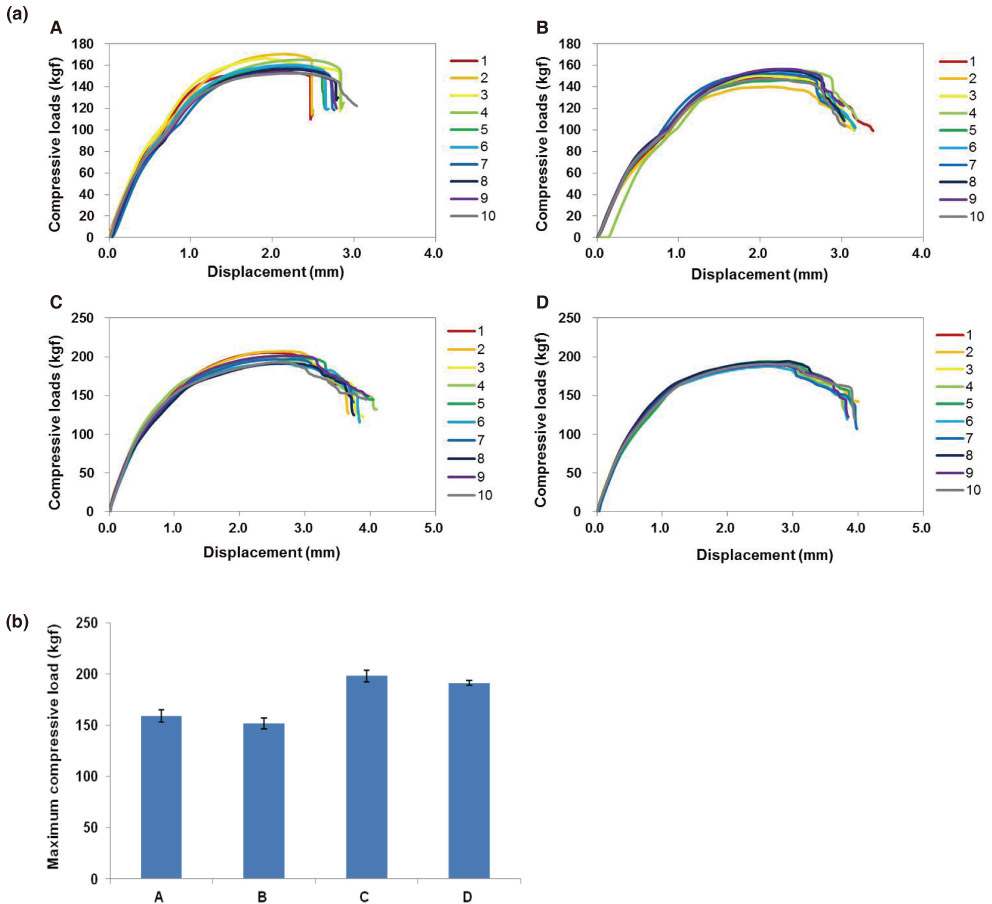
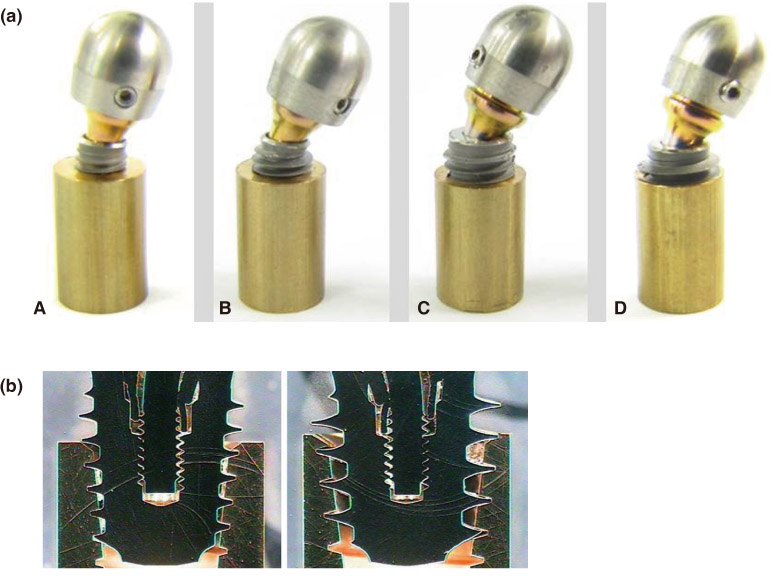
The insertion torque was measured by inserting Ti implants with different thread depths into solid rigid polyurethane blocks (Sawbones) with three different bone densities (0.16 g/cm3, 0.24 g/cm3, and 0.32 g/cm3). The insertion torque value was evaluated with a surgical engine. The static compressive strength was measured with a universal testing machine (UTM) and the Ti implants were aligned at 30degrees against the loading direction of the UTM. After the static compressive strength test, the Ti implants were analyzed with a Measurescope.
RESULTS
The Ti implants with deeper thread depth showed statistically higher mean insertion torque values (P<.001). Groups A and group B had similar maximum static compressive strengths, as did groups C and D (P>.05). After the static compressive strength, the thread shape of the Ti implants with deeper thread depth did not show any breakage but did show deformation of the implant body and abutment.
CONCLUSION
The implants with deeper thread depth had higher mean insertion torque values but not lower compressive strength. The deep threads had a mechanical stability. Implants with deeper thread depth may increase the primary stability in areas of poor quality bone without decreasing mechanical strength.
Keyword
MeSH Terms
Figure
Reference
-
1. Heschl A, Payer M, Platzer S, Wegscheider W, Pertl C, Lorenzoni M. Immediate rehabilitation of the edentulous mandible with screw type implants: results after up to 10 years of clinical function. Clin Oral Implants Res. 2012; 23:1217–1223.2. Testori T, Wiseman L, Woolfe S, Porter SS. A prospective multicenter clinical study of the Osseotite implant: four-year interim report. Int J Oral Maxillofac Implants. 2001; 16:193–200.3. Friberg B, Ekestubbe A, Sennerby L. Clinical outcome of Brånemark System implants of various diameters: a retrospective study. Int J Oral Maxillofac Implants. 2002; 17:671–677.4. Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991; 62:2–4.5. Tabassum A, Meijer GJ, Wolke JG, Jansen JA. Influence of the surgical technique and surface roughness on the primary stability of an implant in artificial bone with a density equivalent to maxillary bone: a laboratory study. Clin Oral Implants Res. 2009; 20:327–332.6. Lioubavina-Hack N, Lang NP, Karring T. Significance of primary stability for osseointegration of dental implants. Clin Oral Implants Res. 2006; 17:244–250.7. Tabassum A, Walboomers XF, Wolke JG, Meijer GJ, Jansen JA. Bone particles and the undersized surgical technique. J Dent Res. 2010; 89:581–586.8. Fanuscu MI, Chang TL, Akça K. Effect of surgical techniques on primary implant stability and peri-implant bone. J Oral Maxillofac Surg. 2007; 65:2487–2491.9. Marković A, Calasan D, Colić S, Stojčev-Stajčić L, Janjić B, Mišić T. Implant stability in posterior maxilla: bone-condensing versus bone-drilling: a clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112:557–563.10. Cehreli MC, Kökat AM, Comert A, Akkocaoğlu M, Tekdemir I, Akça K. Implant stability and bone density: assessment of correlation in fresh cadavers using conventional and osteotome implant sockets. Clin Oral Implants Res. 2009; 20:1163–1169.11. Padmanabhan TV, Gupta RK. Comparison of crestal bone loss and implant stability among the implants placed with conventional procedure and using osteotome technique: a clinical study. J Oral Implantol. 2010; 36:475–483.12. Dos Santos MV, Elias CN, Cavalcanti Lima JH. The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res. 2011; 13:215–223.13. Tabassum A, Meijer GJ, Wolke JG, Jansen JA. Influence of surgical technique and surface roughness on the primary stability of an implant in artificial bone with different cortical thickness: a laboratory study. Clin Oral Implants Res. 2010; 21:213–220.14. Schwartz Z, Raz P, Zhao G, Barak Y, Tauber M, Yao H, Boyan BD. Effect of micrometer-scale roughness of the surface of Ti6Al4V pedicle screws in vitro and in vivo. J Bone Joint Surg Am. 2008; 90:2485–2498.15. Wennerberg A, Albrektsson T, Johansson C, Andersson B. Experimental study of turned and grit-blasted screw-shaped implants with special emphasis on effects of blasting material and surface topography. Biomaterials. 1996; 17:15–22.16. Wennerberg A, Albrektsson T, Lausmaa J. Torque and histomorphometric evaluation of c.p. titanium screws blasted with 25- and 75-microns-sized particles of Al2O3. J Biomed Mater Res. 1996; 30:251–260.17. Kim YK, Kim YJ, Yun PY, Kim JW. Effects of the taper shape, dual-thread, and length on the mechanical properties of mini-implants. Angle Orthod. 2009; 79:908–914.18. Sakoh J, Wahlmann U, Stender E, Nat R, Al-Nawas B, Wagner W. Primary stability of a conical implant and a hybrid, cylindric screw-type implant in vitro. Int J Oral Maxillofac Implants. 2006; 21:560–566.19. Wilmes B, Ottenstreuer S, Su YY, Drescher D. Impact of implant design on primary stability of orthodontic mini-implants. J Orofac Orthop. 2008; 69:42–50.20. Kim YS, Lim YJ. Primary stability and self-tapping blades: biomechanical assessment of dental implants in medium-density bone. Clin Oral Implants Res. 2011; 22:1179–1184.21. Ao J, Li T, Liu Y, Ding Y, Wu G, Hu K, Kong L. Optimal design of thread height and width on an immediately loaded cylinder implant: a finite element analysis. Comput Biol Med. 2010; 40:681–686.22. Chun HJ, Cheong SY, Han JH, Heo SJ, Chung JP, Rhyu IC, Choi YC, Baik HK, Ku Y, Kim MH. Evaluation of design parameters of osseointegrated dental implants using finite element analysis. J Oral Rehabil. 2002; 29:565–574.23. Kong L, Hu K, Li D, Song Y, Yang J, Wu Z, Liu B. Evaluation of the cylinder implant thread height and width: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2008; 23:65–74.24. Abuhussein H, Pagni G, Rebaudi A, Wang HL. The effect of thread pattern upon implant osseointegration. Clin Oral Implants Res. 2010; 21:129–136.25. Carr AB, Papazoglou E, Larsen PE. The relationship of Periotest values, biomaterial, and torque to failure in adult baboons. Int J Prosthodont. 1995; 8:15–20.26. Isidor F. Mobility assessment with the Periotest system in relation to histologic findings of oral implants. Int J Oral Maxillofac Implants. 1998; 13:377–383.27. Rabel A, Köhler SG, Schmidt-Westhausen AM. Clinical study on the primary stability of two dental implant systems with resonance frequency analysis. Clin Oral Investig. 2007; 11:257–265.28. Trisi P, De Benedittis S, Perfetti G, Berardi D. Primary stability, insertion torque and bone density of cylindric implant ad modum Branemark: is there a relationship? An in vitro study. Clin Oral Implants Res. 2011; 22:567–570.29. Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006; 17:109–114.30. Wiskott HW, Nicholls JI, Belser UC. Stress fatigue: basic principles and prosthodontic implications. Int J Prosthodont. 1995; 8:105–116.31. Lee SY, Yang DJ, Yeo S, An HW, Kim SJ, Choi WM, Park KB. Effect of XPEED® on Ti implants with deep threads. Key Eng Mater. 2012; 493-4:442–446.32. Isidor F. Loss of osseointegration caused by occlusal load of oral implants. A clinical and radiographic study in monkeys. Clin Oral Implants Res. 1996; 7:143–152.33. Isidor F. Histological evaluation of peri-implant bone at implants subjected to occlusal overload or plaque accumulation. Clin Oral Implants Res. 1997; 8:1–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The influence of thread geometry on implant osseointegration under immediate loading: a literature review
- Three-dimensional optimization and sensitivity analysis of dental implant thread parameters using finite element analysis
- studies of Osseointegrated Implant-Models on Stress Distribution
- The Three Dimensional Finite Element Analysis of Stress according to Implant Thread Design under the Axial Load
- Alternative Method to Salvage an Internally Damaged Implant using Cast Post