J Korean Orthop Assoc.
2015 Apr;50(2):93-106. 10.4055/jkoa.2015.50.2.93.
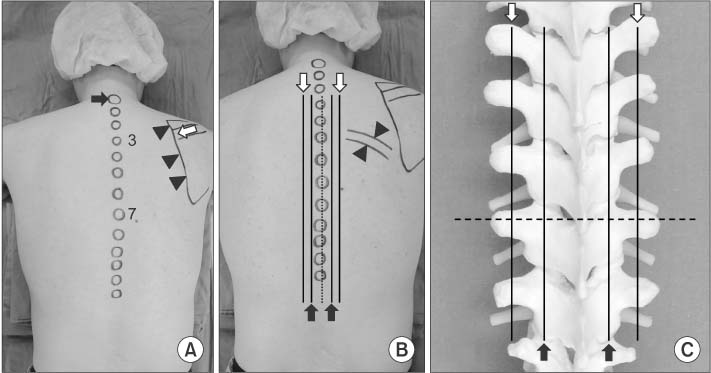
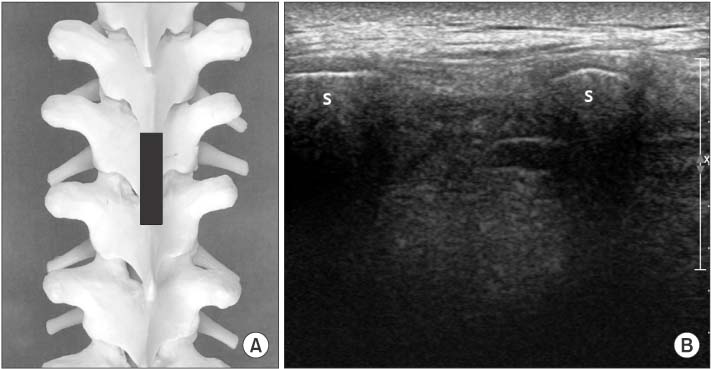
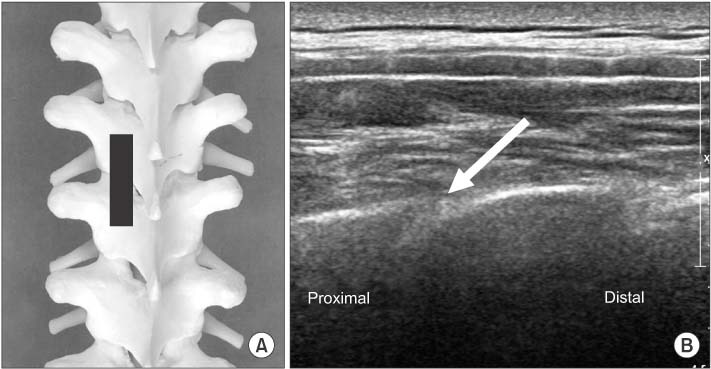
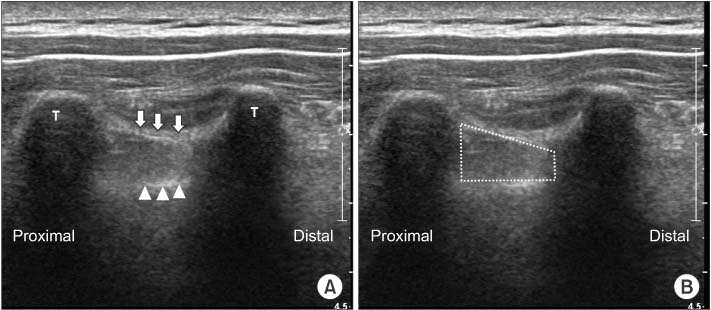
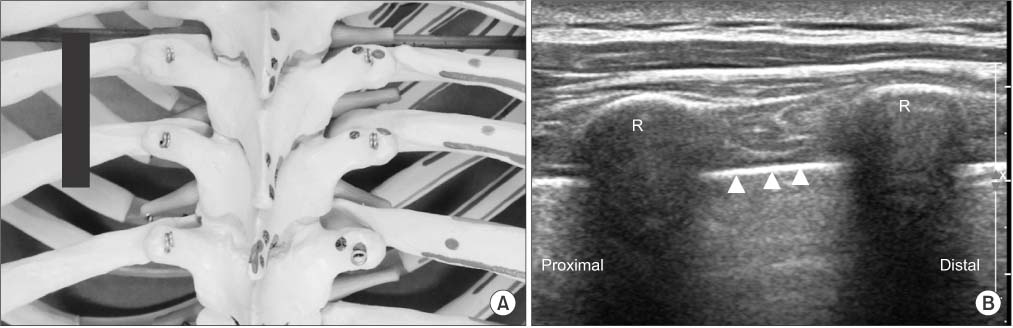
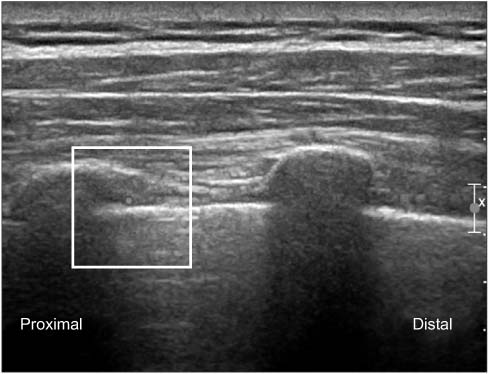
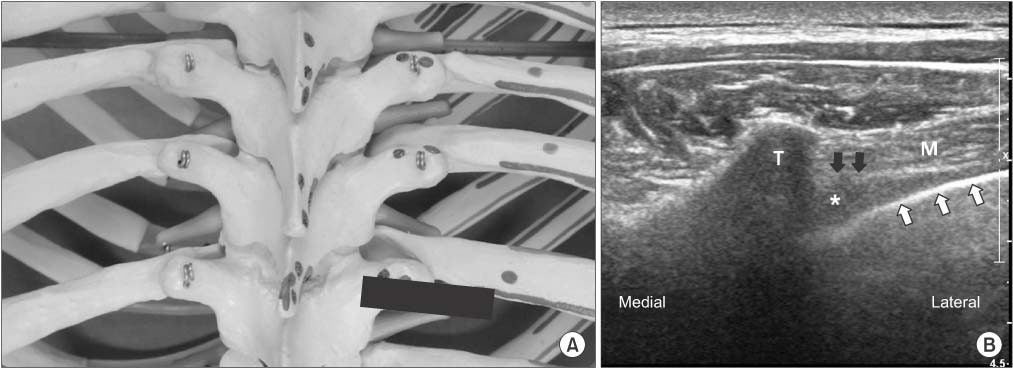
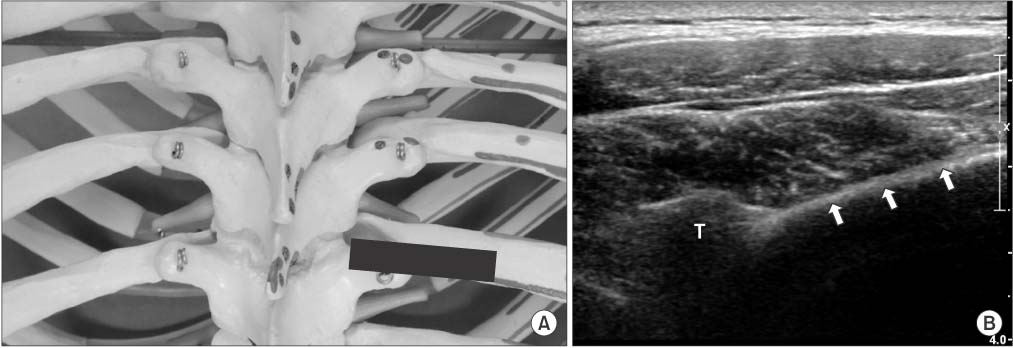
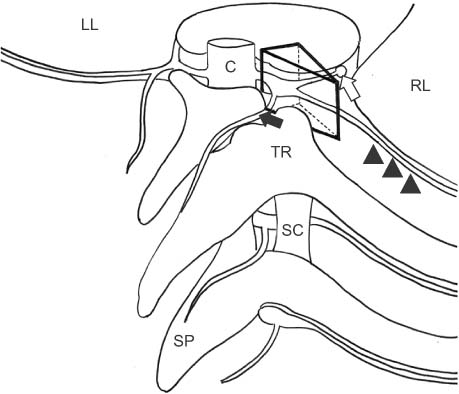
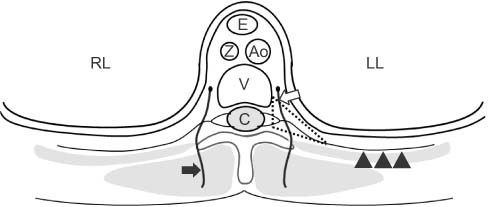
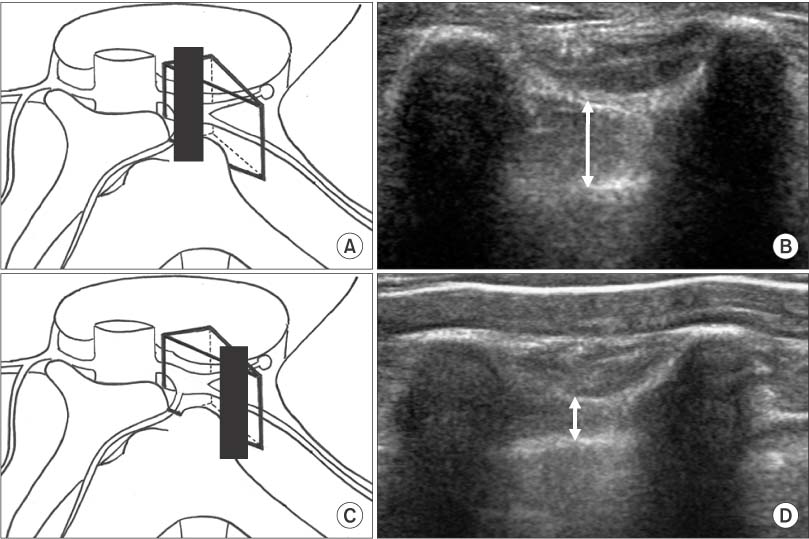
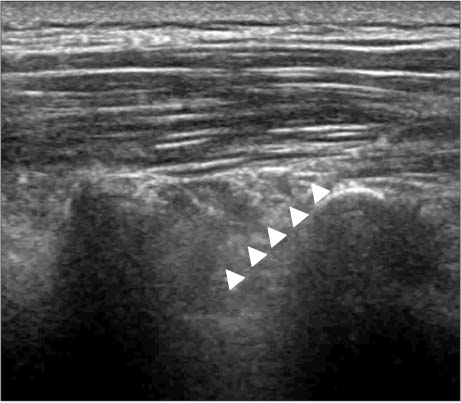
Ultrasound-Guided Intervention in Thoracic Spine
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea. msh124@paran.com
- KMID: 2106744
- DOI: http://doi.org/10.4055/jkoa.2015.50.2.93
Abstract
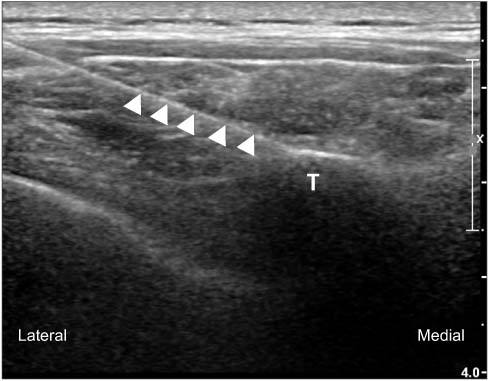
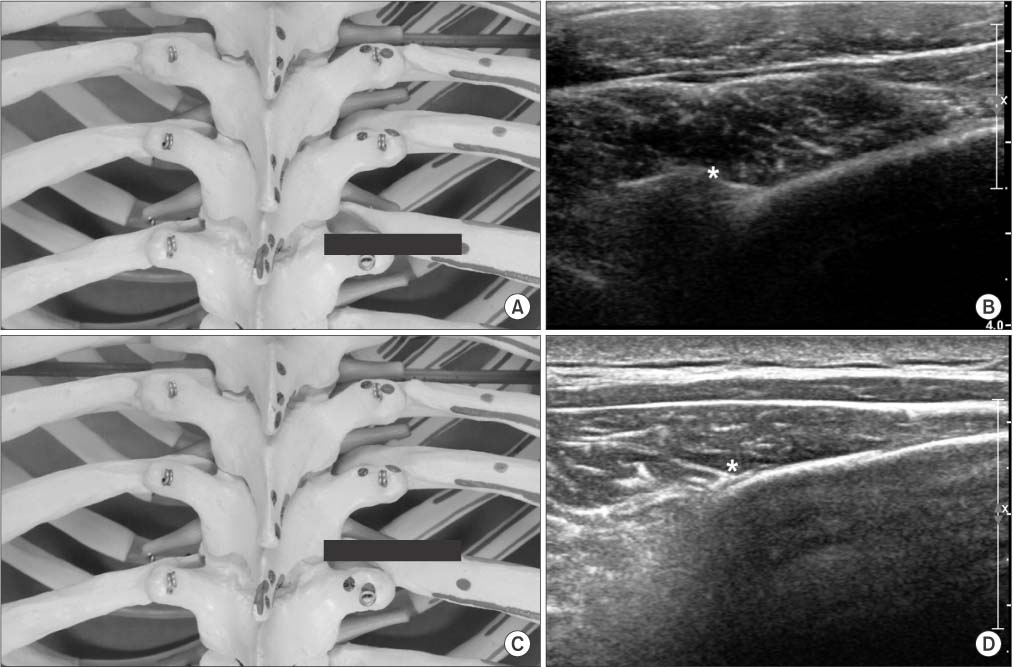
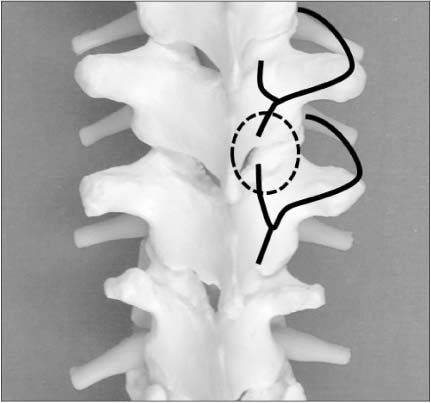
- Even though thoracic spinal pain may be less common than low back and neck pain, the prevalence of thoracic pain in the general population is 13% to 15% in the literature and it can be as disabling as lumbar or cervical pain. Although thoracic interventions have been reported to be effective, it is rarely performed due to concerns of creating iatrogenic pneumothorax. Fluoroscopy-guided interventions are more accurate procedures than blind technique but still cannot prevent pneumothorax. In recent reports in the literature, use of ultrasound-guided interventions minimized the risk of pneumothorax and vascular puncture because ultrasound can visualize lung with pleura and also detect vascular structures by Doppler scan. Compared with fluoroscopy, ultrasound imaging has no known contraindications, produces no ionizing radiation, enables direct visualization of neurovascular and soft tissue structures, and provides real-time visualization of needle passage toward the intended target. We therefore conducted a review to investigate the feasibility of performing thoracic interventions under real-time ultrasound guidance.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Validation of Ultrasound-Guided Target Segment Identification in Thoracic Spine as Confirmed by Fluoroscopy
Ju-Yeong Heo, Ji-Won Lee, Cheol-Hwan Kim, Sang-Min Lee, Yong-Soo Choi
Clin Orthop Surg. 2017;9(4):472-479. doi: 10.4055/cios.2017.9.4.472.
Reference
-
1. Linton SJ, Hellsing AL, Halldèn K. A population-based study of spinal pain among 35-45-year-old individuals. Prevalence, sick leave, and health care use. Spine (Phila Pa 1976). 1998; 23:1457–1463.2. Leboeuf-Yde C, Nielsen J, Kyvik KO, Fejer R, Hartvigsen J. Pain in the lumbar, thoracic or cervical regions: do age and gender matter? A population-based study of 34,902 Danish twins 20-71 years of age. BMC Musculoskelet Disord. 2009; 10:39.
Article3. Edmondston SJ, Singer KP. Thoracic spine: anatomical and biomechanical considerations for manual therapy. Man Ther. 1997; 2:132–143.
Article4. Moon SH. Ultrasound-guided intervention in lumbar spine. J Korean Orthop US Soc. 2013; 2:81–93.5. Moon SH. Ultrasound-guided intervention in cervical spine. J Korean Orthop US Soc. 2014; 1:49–66.6. Purcell-Jones G, Pither CE, Justins DM. Paravertebral somatic nerve block: a clinical, radiographic, and computed tomographic study in chronic pain patients. Anesth Analg. 1989; 68:32–39.7. Richardson J, Lönnqvist PA. Thoracic paravertebral block. Br J Anaesth. 1998; 81:230–238.
Article8. Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2006; 96:418–426.9. Joshi GP, Bonnet F, Shah R, et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg. 2008; 107:1026–1040.
Article10. Eason MJ, Wyatt R. Paravertebral thoracic block-a reappraisal. Anaesthesia. 1979; 34:638–642.
Article11. Lönnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade. Failure rate and complications. Anaesthesia. 1995; 50:813–815.12. Cowie B, McGlade D, Ivanusic J, Barrington MJ. Ultrasound-guided thoracic paravertebral blockade: a cadaveric study. Anesth Analg. 2010; 110:1735–1739.13. Renes SH, Bruhn J, Gielen MJ, Scheffer GJ, van Geffen GJ. In-plane ultrasound-guided thoracic paravertebral block: a preliminary report of 36 cases with radiologic confirmation of catheter position. Reg Anesth Pain Med. 2010; 35:212–216.14. O Riain SC, Donnell BO, Cuffe T, Harmon DC, Fraher JP, Shorten G. Thoracic paravertebral block using real-time ultrasound guidance. Anesth Analg. 2010; 110:248–251.15. Shanti CM, Carlin AM, Tyburski JG. Incidence of pneumothorax from intercostal nerve block for analgesia in rib fractures. J Trauma. 2001; 51:536–539.
Article16. Ozkan D, Akkaya T, Karakoyunlu N, et al. Effect of ultrasound-guided intercostal nerve block on postoperative pain after percutaneous nephrolithotomy: prospective randomized controlled study. Anaesthesist. 2013; 62:988–994.17. Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004; 5:15.
Article18. Manchikanti L, Singh V, Pampati V, Beyer CD, Damron KS. Evaluation of the prevalence of facet joint pain in chronic thoracic pain. Pain Physician. 2002; 5:354–359.
Article19. Manchikanti L, Singh V, Falco FJ, Cash KA, Pampati V, Fellows B. Comparative effectiveness of a one-year follow-up of thoracic medial branch blocks in management of chronic thoracic pain: a randomized, double-blind active controlled trial. Pain Physician. 2010; 13:535–548.20. Dreyfuss P, Tibiletti C, Dreyer SJ. Thoracic zygapophyseal joint pain patterns. A study in normal volunteers. Spine (Phila Pa 1976). 1994; 19:807–811.21. Fukui S, Ohseto K, Shiotani M. Patterns of pain induced by distending the thoracic zygapophyseal joints. Reg Anesth. 1997; 22:332–336.
Article22. Atluri S, Datta S, Falco FJ, Lee M. Systematic review of diagnostic utility and therapeutic effectiveness of thoracic facet joint interventions. Pain Physician. 2008; 11:611–629.23. Chua WH, Bogduk N. The surgical anatomy of thoracic facet denervation. Acta Neurochir (Wien). 1995; 136:140–144.
Article24. Manchikanti L, Manchikanti KN, Manchukonda R, Pampati V, Cash KA. Evaluation of therapeutic thoracic medial branch block effectiveness in chronic thoracic pain: a prospective outcome study with minimum 1-year follow up. Pain Physician. 2006; 9:97–105.25. Stulc SM, Hurdle MF, Pingree MJ, Brault JS, Porter CA. Ultrasound-guided thoracic facet injections: description of a technique. J Ultrasound Med. 2011; 30:357–362.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided interventions for controlling the thoracic spine and chest wall pain: a narrative review
- Ultrasound-Guided Intervention in Lumbar Spine
- Ultrasound-guided interventions for spinal pain
- The Validation of Ultrasound-Guided Target Segment Identification in Thoracic Spine as Confirmed by Fluoroscopy
- Ultrasound-Guided Injections in the Lumbar and Sacral Spine