J Yeungnam Med Sci.
2022 Jul;39(3):190-199. 10.12701/jyms.2022.00192.
Ultrasound-guided interventions for controlling the thoracic spine and chest wall pain: a narrative review
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 2Department of Physical Medicine and Rehabilitation, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2532071
- DOI: http://doi.org/10.12701/jyms.2022.00192
Abstract
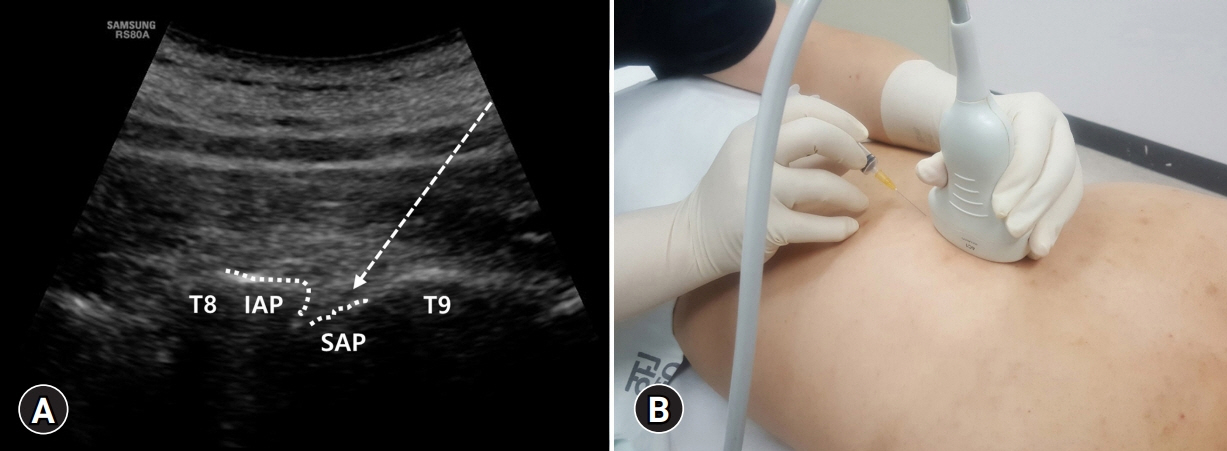
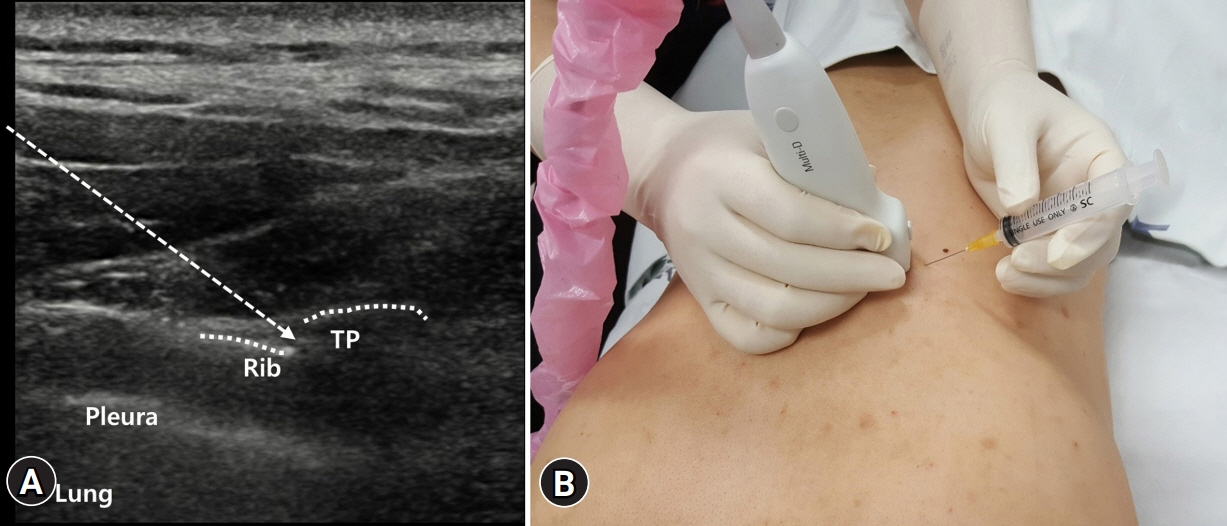
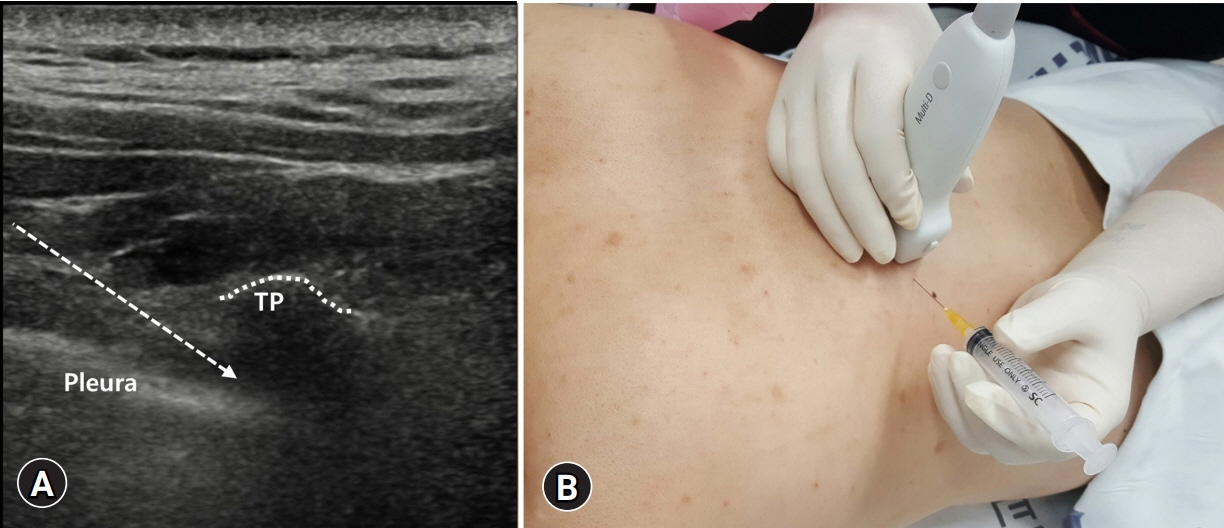
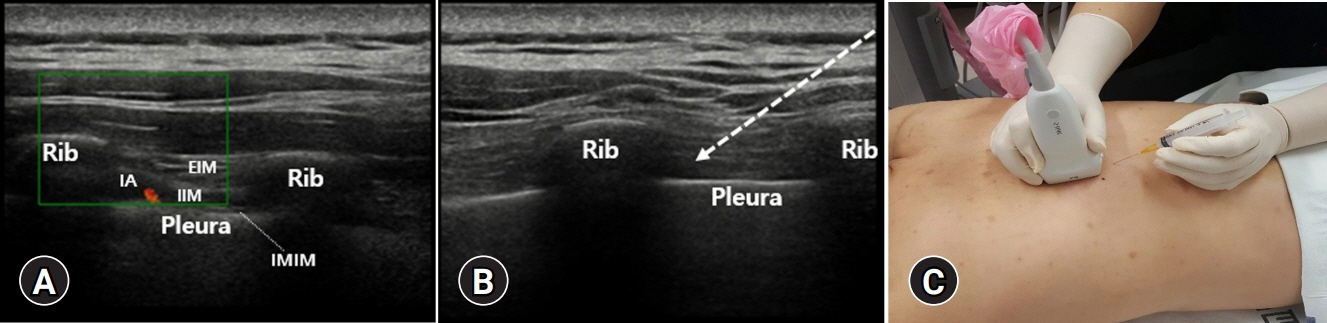
- Ultrasound-guided injection is useful for managing thoracic spine and chest wall pain. With ultrasound, pain physicians perform the injection with real-time viewing of major structures, such as the pleura, vasculature, and nerves. Therefore, the ultrasound-guided injection procedure not only prevents procedure-related adverse events but also increases the accuracy of the procedure. Here, ultrasound-guided interventions that could be applied for thoracic spine and chest wall pain were described. We presented ultrasound-guided thoracic facet joint and costotransverse joint injections and thoracic paravertebral, intercostal nerve, erector spinae plane, and pectoralis and serratus plane blocks. The indication, anatomy, Sonoanatomy, and technique for each procedure were also described. We believe that our article is helpful for clinicians to conduct ultrasound-guided injections for controlling thoracic spine and chest wall pain precisely and safely.
Keyword
Figure
Cited by 1 articles
-
The blind spot and challenges in pain management
Min Cheol Chang
J Yeungnam Med Sci. 2022;39(3):179-180. doi: 10.12701/jyms.2022.00339.
Reference
-
References
1. Kim D. Bipolar intra-articular radiofrequency thermocoagulation of the thoracic facet joints: a case series of a new technique. Korean J Pain. 2014; 27:43–8.
Article2. Suzuki N, Ogikubo O, Hansson T. The prognosis for pain, disability, activities of daily living and quality of life after an acute osteoporotic vertebral body fracture: its relation to fracture level, type of fracture and grade of fracture deformation. Eur Spine J. 2009; 18:77–88.
Article3. Lee DG, Ahn SH, Cho YW, Do KH, Kwak SG, Chang MC. Comparison of intra-articular thoracic facet joint steroid injection and thoracic medial branch block for the management of thoracic facet joint pain. Spine (Phila Pa 1976). 2018; 43:76–80.
Article4. Chang MC, Boudier-Revéret M, Hsiao MY. Ultrasound-guided three-in-one trigger point injection for muscles of the posterior axillary fold. Pain Pract. 2020; 20:110–1.
Article5. Fujii T, Shibata Y, Shinya S, Nishiwaki K. Transverse vs. parasagittal in-plane approaches in ultrasound-guided paravertebral block using a microconvex probe: a randomised controlled trial. Eur J Anaesthesiol. 2020; 37:752–7.6. Park D. Ultrasonography of the transverse movement and deformation of the median nerve and its relationships with electrophysiological severity in the early stages of carpal tunnel syndrome. PM R. 2017; 9:1085–94.
Article7. Lee DH, Hong SK, Lee YS, Kim CH, Hwang JM, Lee Z, et al. Is abdominal hollowing exercise using real-time ultrasound imaging feedback helpful for selective strengthening of the transversus abdominis muscle?: a prospective, randomized, parallel-group, comparative study. Medicine (Baltimore). 2018; 97:e11369.8. Waxenbaum JA, Reddy V, Futterman B. Anatomy, back, thoracic vertebrae. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;2022. [cited 2021 Aug 12]. https://www.ncbi.nlm.nih.gov/books/NBK459153/.9. Jaumard NV, Welch WC, Winkelstein BA. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng. 2011; 133:071010.
Article10. Chang MC. Effect of pulsed radiofrequency treatment on the thoracic medial branch for managing chronic thoracic facet joint pain refractory to medial branch block with local anesthetics. World Neurosurg. 2018; 111:e644–8.
Article11. Lau LS, Littlejohn GO. Costotransverse joint injection description of technique. Australas Radiol. 1987; 31:47–9.
Article12. Ardon AE, Lee J, Franco CD, Riutort KT, Greengrass RA. Paravertebral block: anatomy and relevant safety issues. Korean J Anesthesiol. 2020; 73:394–400.
Article13. Karmakar MK. Thoracic paravertebral block. Anesthesiology. 2001; 95:771–80.
Article14. Hetta DF, Rezk KM. Pectoralis-serratus interfascial plane block vs thoracic paravertebral block for unilateral radical mastectomy with axillary evacuation. J Clin Anesth. 2016; 34:91–7.
Article15. Lopez-Rincon RM, Kumar V. Ultrasound-guided intercostal nerve block. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;2022. [cited 2021 Jul 31]. https://www.ncbi.nlm.nih.gov/books/NBK555900/.16. Glenesk NL, Rahman S, Lopez PP. Anatomy, thorax, intercostal nerves. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;2022. [cited 2021 Jul 26]. https://www.ncbi.nlm.nih.gov/books/NBK538238/.17. Tulgar S, Ahiskalioglu A, De Cassai A, Gurkan Y. Efficacy of bilateral erector spinae plane block in the management of pain: current insights. J Pain Res. 2019; 12:2597–613.18. Tulgar S, Kose HC, Selvi O, Senturk O, Thomas DT, Ermis MN, et al. Comparison of ultrasound-guided lumbar erector spinae plane block and transmuscular quadratus lumborum block for postoperative analgesia in hip and proximal femur surgery: a prospective randomized feasibility study. Anesth Essays Res. 2018; 12:825–31.
Article19. Ibbotson WJ, Greenberg R, Brendt P. Erector spinae block for chest trauma in aeromedical prehospital and retrieval medicine. Prehosp Disaster Med. 2020; 35:454–6.
Article20. Elkoundi A, El Koraichi A. Erector spinae plane block dilemma. Reg Anesth Pain Med. 2020; 45:842–3.
Article21. Czuczman M, Shanthanna H, Alolabi B, Moisiuk P, O’Hare T, Khan M, et al. Randomized control trial of ultrasound-guided erector spinae block versus shoulder periarticular anesthetic infiltration for pain control after arthroscopic shoulder surgery: study protocol clinical trial (SPIRIT compliant). Medicine (Baltimore). 2020; 99:e19721.22. Hong B, Bang S, Chung W, Yoo S, Chung J, Kim S. Multimodal analgesia with multiple intermittent doses of erector spinae plane block through a catheter after total mastectomy: a retrospective observational study. Korean J Pain. 2019; 32:206–14.
Article23. Tulgar S, Selvi O, Senturk O, Serifsoy TE, Thomas DT. Ultrasound-guided erector spinae plane block: indications, complications, and effects on acute and chronic pain based on a single-center experience. Cureus. 2019; 11:e3815.
Article24. Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013; 68:1107–13.
Article25. Kunhabdulla NP, Agarwal A, Gaur A, Gautam SK, Gupta R, Agarwal A. Serratus anterior plane block for multiple rib fractures. Pain Physician. 2014; 17:E651–3.26. Fu P, Weyker PD, Webb CA. Case report of serratus plane catheter for pain management in a patient with multiple rib fractures and an inferior scapular fracture. A A Case Rep. 2017; 8:132–5.
Article27. Kiss G, Castillo M. Non-intubated anesthesia in thoracic surgery-technical issues. Ann Transl Med. 2015; 3:109.28. Kaushal B, Chauhan S, Saini K, Bhoi D, Bisoi AK, Sangdup T, et al. Comparison of the efficacy of ultrasound-guided serratus anterior plane block, pectoral nerves II block, and intercostal nerve block for the management of postoperative thoracotomy pain after pediatric cardiac surgery. J Cardiothorac Vasc Anesth. 2019; 33:418–25.
Article29. Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician. 2015; 18:E421–4.30. Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015; 40:68–74.31. Maldonado KA, Tadi P. Anatomy, thorax, medial pectoral nerves. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;2022. [cited 2021 Sep 3]. https://www.ncbi.nlm.nih.gov/books/NBK556059/.32. Tigga SR, Wadhwa S, Goswami P. Unusual communications of the brachial plexus. Int J Appl Basic Med Res. 2016; 6:68–70.
Article33. Polcaro L, Charlick M, Daly DT. Anatomy, head and neck, brachial plexus. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;2022. [cited 2021 Aug 25]. https://www.ncbi.nlm.nih.gov/books/NBK531473/.34. Fujiwara A, Komasawa N, Minami T. Pectoral nerves (PECS) and intercostal nerve block for cardiac resynchronization therapy device implantation. Springerplus. 2014; 3:409.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-Guided Intervention in Thoracic Spine
- Ultrasound-guided interventions for spinal pain
- Ultrasound-Guided Intervention in Lumbar Spine
- Treatment of Isolated Sternal Fracture with Ultrasound-Guided Paravertebral Nerve Block: a Case Report and Literature Review
- Ultrasound-Guided Lumbar Transforaminal Epidural Injection: A Narrative Review