J Korean Orthop Assoc.
2015 Apr;50(2):77-92. 10.4055/jkoa.2015.50.2.77.
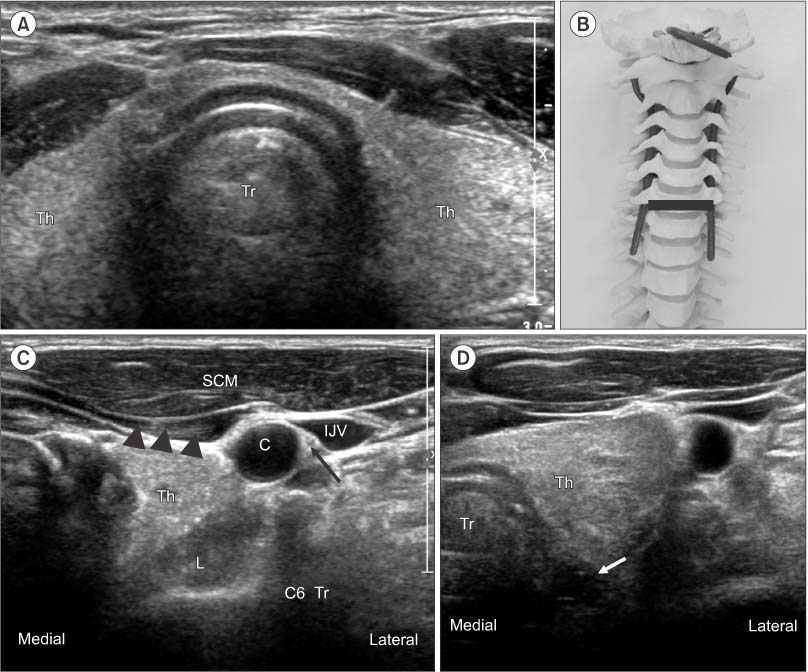
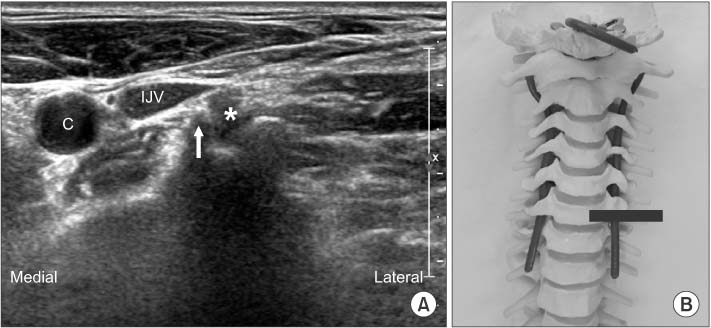
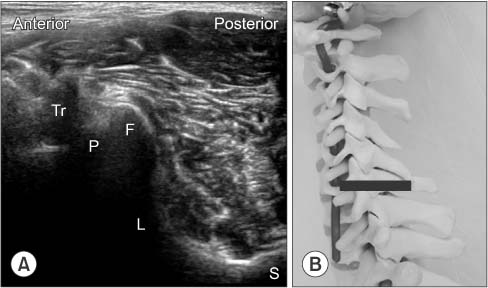
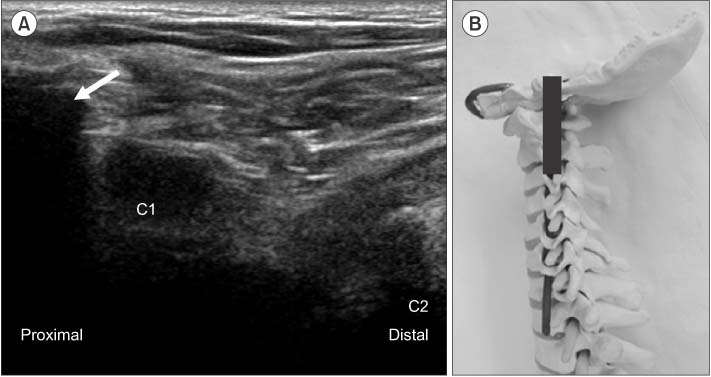
Ultrasound-Guided Intervention in Cervical Spine
- Affiliations
-
- 1Sun's Orthopaedic Clinic, Seoul, Korea.
- 2Department of Orthopedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea. msh124@paran.com
- KMID: 2106743
- DOI: http://doi.org/10.4055/jkoa.2015.50.2.77
Abstract
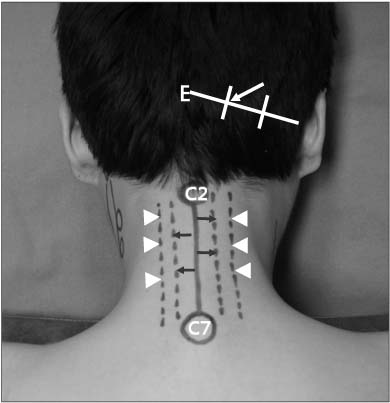
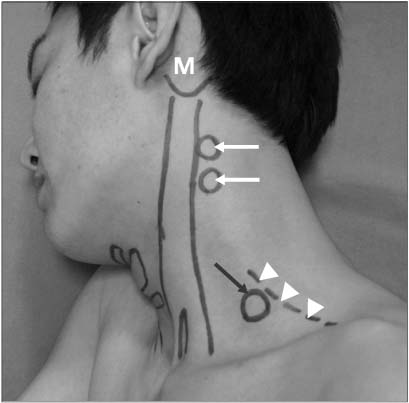
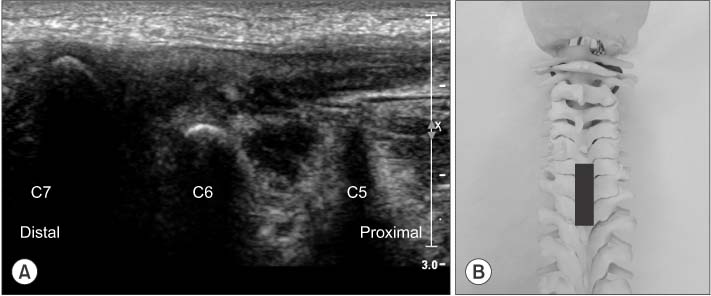
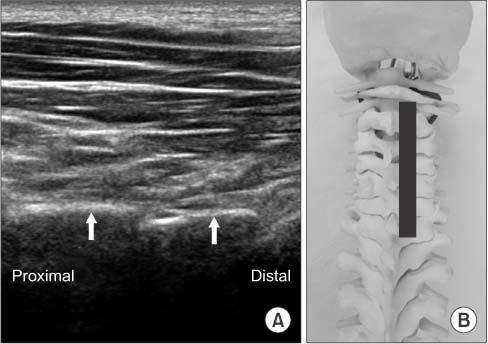
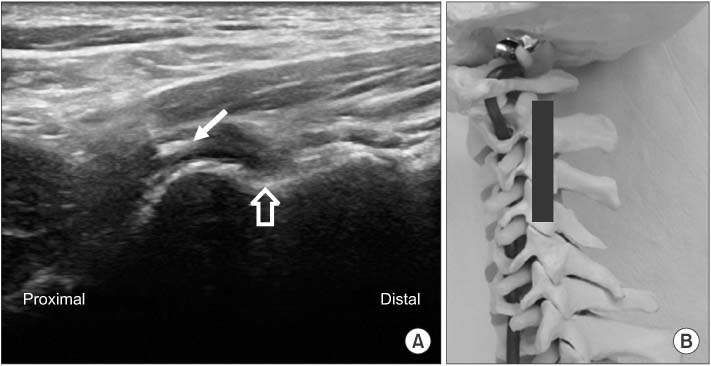
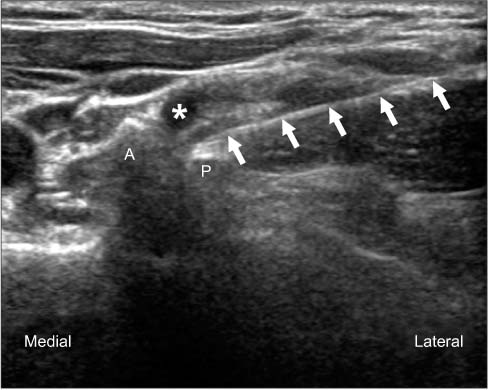
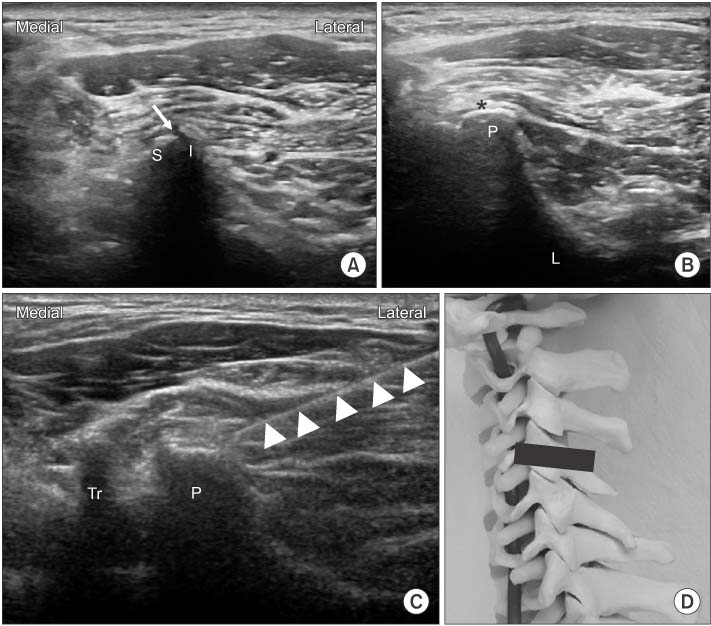
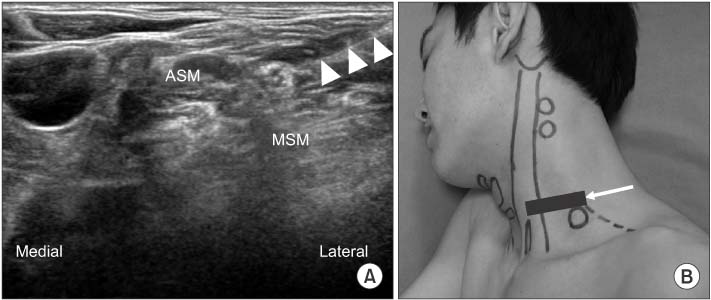
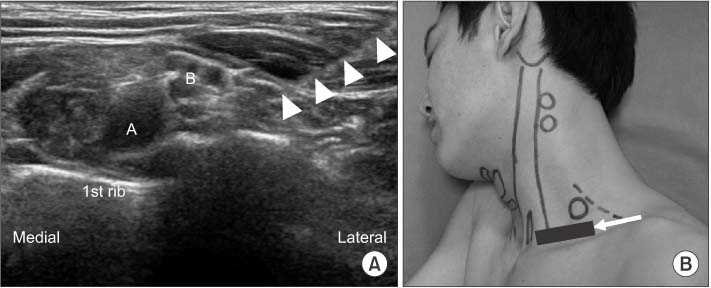
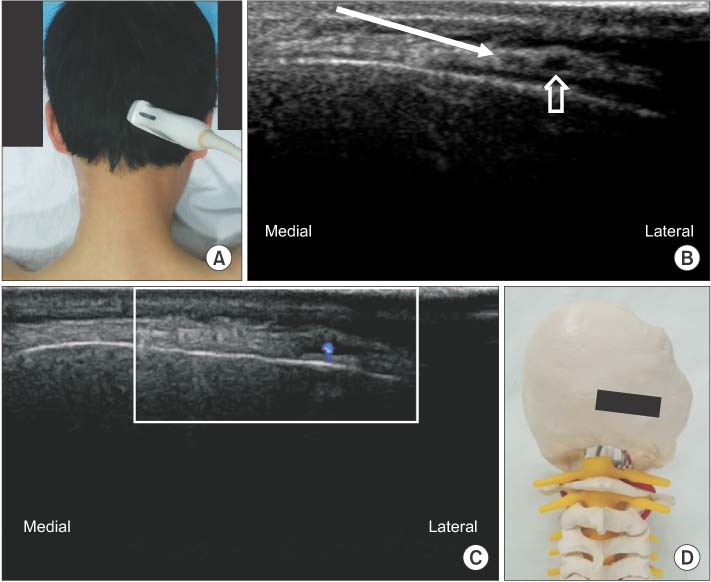
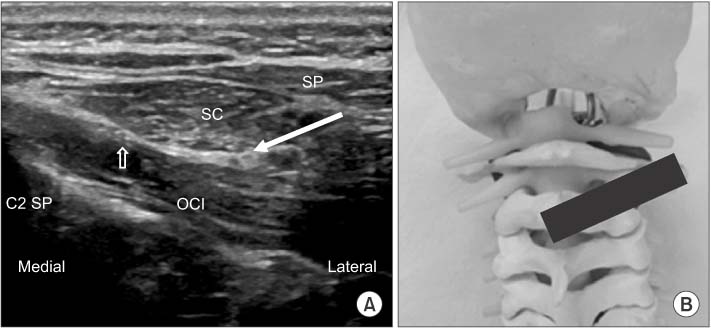
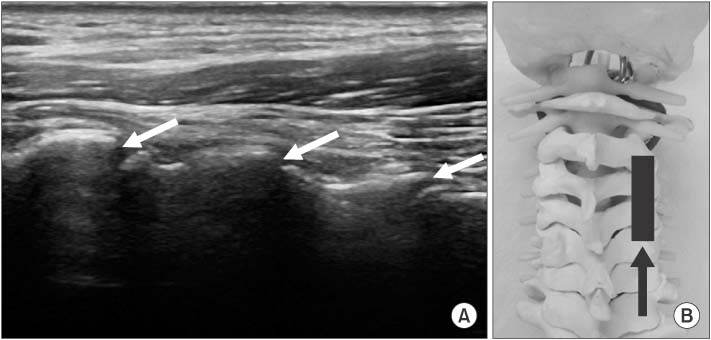
- Interventional procedures around the cervical spine have been classically performed under the guidance of fluoroscopy with radiation hazards to patients and doctors. Even though under fluoroscopic guidance, vascular and nerve structures cannot be shown and there are actual risks for the patient. Nowadays, we can use high resolution image ultrasound around cervical spine procedures. Real time imaging is possible. Cervical root block, medial branch block and many other interventions can be performed under ultrasound guidance. In out-patient clinics, ultrasound is very helpful in management of cervical problems in differentiating the origin of pain and treatment for the pain. Ultrasound is radiation free, easy to use and the imaging can be performed continuously while the injectant is visualized in real-time, increasing the precision of injection. Importantly, ultrasound enables visualization of major nerves and vessels and thus leads to improved safety of cervical interventions by decreasing the incidence of injury or injection into nearby vasculature. We therefore performed a review to investigate the feasibility of performing cervical interventions under real-time ultrasound guidance.
Keyword
Figure
Cited by 1 articles
-
Comparison of the Clinical Outcomes of an Ultrasound-Guided and C-Arm Guided Cervical Nerve Root Block
Dae Ho Ha, Dae Moo Shim, Tae Kyun Kim, Sung Kyun Oh, Hyun Jun Lee
J Korean Orthop Assoc. 2020;55(1):78-84. doi: 10.4055/jkoa.2020.55.1.78.
Reference
-
1. Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004; 100:1595–1600.
Article2. Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004; 4:468–474.3. Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215.
Article4. Provenzano DA, Fanciullo G. Cervical transforaminal epidural steroid injections: should we be performing them? Reg Anesth Pain Med. 2007; 32:168.
Article5. Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine (Phila Pa 1976). 2007; 32:1249–1256.6. Suresh S, Berman J, Connell DA. Cerebellar and brainstem infarction as a complication of CT-guided transforaminal cervical nerve root block. Skeletal Radiol. 2007; 36:449–452.
Article7. Moon SH. Ultrasound-guided intervention in cervical spine. J Korean Orthop US Soc. 2014; 1:49–66.8. Nakagawa M, Shinbori H, Ohseto K. Ultrasound-guided and fluoroscopy-assisted selective cervical nerve root blocks. Masui. 2009; 58:1506–1511.9. Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009; 34:343–348.10. Razzaq AA, O'Brien D, Mathew B, Bartlett R, Taylor D. Efficacy and durability of fluoroscopically guided cervical nerve root block. Br J Neurosurg. 2007; 21:365–369.
Article11. Martin DC, Willis ML, Mullinax LA, Clarke NL, Homburger JA, Berger IH. Pulsed radiofrequency application in the treatment of chronic pain. Pain Pract. 2007; 7:31–35.
Article12. Anderberg L, Annertz M, Rydholm U, Brandt L, Säveland H. Selective diagnostic nerve root block for the evaluation of radicular pain in the multilevel degenerated cervical spine. Eur Spine J. 2006; 15:794–801.
Article13. Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med. 2005; 30:391–396.
Article14. Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasoundguided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013; 42:69–78.
Article15. Yamauchi M, Suzuki D, Niiya T, et al. Ultrasound-guided cervical nerve root block: spread of solution and clinical effect. Pain Med. 2011; 12:1190–1195.
Article16. Manchikanti L, Singh V, Falco FJ, Cash KA, Fellows B. Comparative outcomes of a 2-year follow-up of cervical medial branch blocks in management of chronic neck pain: a randomized, double-blind controlled trial. Pain Physician. 2010; 13:437–450.17. Siegenthaler A, Mlekusch S, Trelle S, Schliessbach J, Curatolo M, Eichenberger U. Accuracy of ultrasound-guided nerve blocks of the cervical zygapophysial joints. Anesthesiology. 2012; 117:347–352.
Article18. Greher M, Moriggl B, Curatolo M, Kirchmair L, Eichenberger U. Sonographic visualization and ultrasound-guided blockade of the greater occipital nerve: a comparison of two selective techniques confirmed by anatomical dissection. Br J Anaesth. 2010; 104:637–642.
Article19. Loukas M, El-Sedfy A, Tubbs RS, et al. Identification of greater occipital nerve landmarks for the treatment of occipital neuralgia. Folia Morphol (Warsz). 2006; 65:337–342.20. Narouze SN, Provenzano DA. Sonographically guided cervical facet nerve and joint injections: why sonography? J Ultrasound Med. 2013; 32:1885–1896.21. Obernauer J, Galiano K, Gruber H, et al. Ultrasound-guided versus Computed Tomography-controlled facet joint injections in the middle and lower cervical spine: a prospective randomized clinical trial. Med Ultrason. 2013; 15:10–15.
Article