J Korean Orthop Assoc.
2011 Feb;46(1):35-41. 10.4055/jkoa.2011.46.1.35.
Significance of Mal-alignment after Anterior Cervical Arthrodesis in Degenerative Cervical Spinal Disorders
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonbuk National University School of Medicine, Research Institute of Clinical Medicine, Chonbuk National University Hospital, Jeonju, Korea.
- 2Department of Orthopedic Surgery, Presbyterian Medical Center, Jeonju, Korea. docby@hanmail.net
- KMID: 2106569
- DOI: http://doi.org/10.4055/jkoa.2011.46.1.35
Abstract
- PURPOSE
The purpose of this study was to analyze the risk factors for postoperative sagittal mal-alignment after anterior cervical arthrodesis resulting from degenerative cervical disorders and its effect on radiological and clinical results.
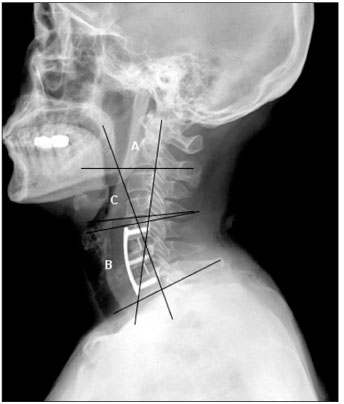
MATERIALS AND METHODS
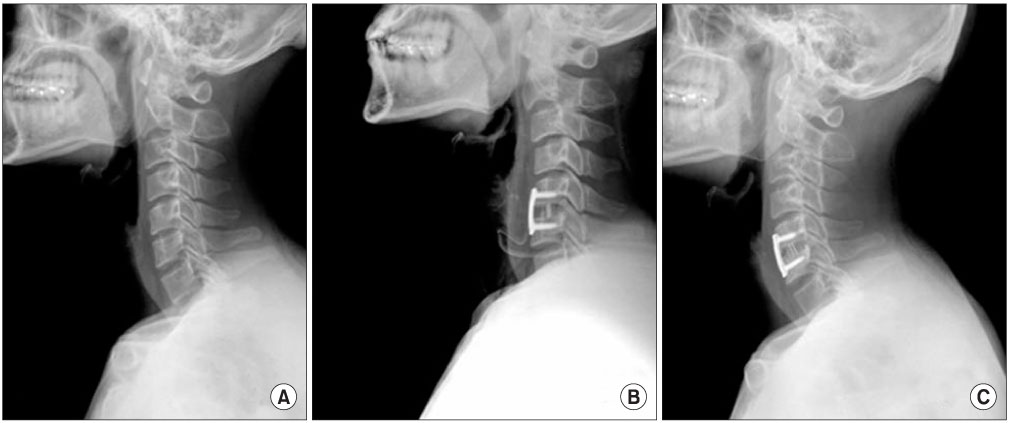
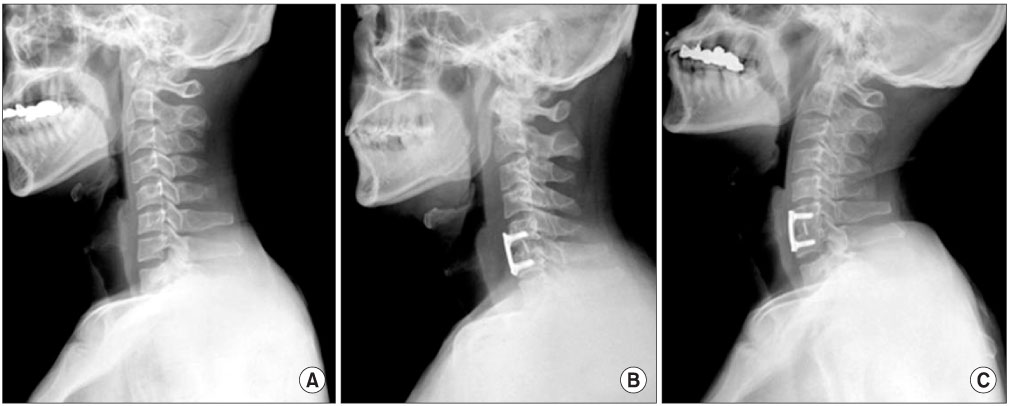
We evaluated 50 patients who underwent anterior cervical arthrodesis for degenerative cervical disorder retrospectively. We assigned 25 patients who had sagittal mal-alignment after surgery to group A and 25 patients who had improvement of lordosis after surgery to group B. We evaluated the change of cervical lordosis, lordosis at fused segments, and lordosis at unfused segments. In addition, we evaluated radiological and clinical results.
RESULTS
In group A, postoperative cervical lordosis worsened from 12.7+/-10.6 to 3.6+/-6.2degrees after surgery (p=0.002), but had recovered to 12.2+/-9.5degrees by the last Follow-up (p=0.859). In group B, cervical lordosis was improved from 9.6+/-10.5degrees to 22.5+/-9.7degrees (p=0.0003) after surgery and correction was maintained to 27.5+/-9.1degrees (p=0.0988) at the last follow up. Lordosis at fused segments were improved in both groups (p=0.001, 0.0001) but lordosis at unfused segments worsend in group A (p=0.0001). The factor associated with postoperative mal-alignment was symtoms of myelopathy (p=0.0436). Age, sex, fusion level, size of cage, and duration of symptoms were not significantly associated with postoperative changes in alignment. One nonunion occurred only in group A. Six cases of cage subsidences were found in group A, 3 cases in group B (p=0.4506). Adjacent segment degeneration was found in 8 segments in group A, 1 segment in group B (p=0.0048). The differences in clinical improvement evaluated by VAS, NDI between groups were not significant (p=0.88, p=0.91).
CONCLUSION
Postoperative sagittal malalignment was a temporary and reversible change, and was not related to clinical results. However, it might be a factor in the increased incidence of adjacent segment degeneration.
Keyword
MeSH Terms
Figure
Reference
-
1. Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955. 96:223–224.
Article2. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993. 75:1298–1307.
Article3. Braunstein EM, Hunter LY, Bailey RW. Long term radiographic changes following anterior cervical fusion. Clin Radiol. 1980. 31:201–203.
Article4. Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine (Phila Pa 1976). 1984. 9:667–671.5. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999. 81:519–528.
Article6. Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001. 10:320–324.
Article7. Katsuura A, Hukuda S, Imanaka T, Miyamoto K, Kanemoto M. Anterior cervical plate used in degenerative disease can maintain cervical lordosis. J Spinal Disord. 1996. 9:470–476.
Article8. Wang JC, McDonough PW, Endow K, Kanim LE, Delamarter RB. The effect of cervical plating on single-level anterior cervical discectomy and fusion. J Spinal Disord. 1999. 12:467–471.
Article9. Wang JC, McDonough PW, Endow KK, Delamarter RB. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2000. 25:41–45.
Article10. Song KJ, Choi BW, Kim KH, Lee KB. Anterior cervical fusion with autogenous iliac bone graft with or without plate fixation for degenerative cervical spinal disorders. J Korean Orthop Assoc. 2008. 43:338–346.
Article11. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986. 11:521–524.
Article12. Kim KT, Suk KS, Kim JM. Future development of interbody fusion cages. J Korean Soc Spine Surg. 2001. 8:386–391.
Article13. Grob D, Frauenfelder H, Mannion AF. The association between cervical spine curvature and neck pain. Eur Spine J. 2007. 16:669–678.
Article14. Takeshima T, Omokawa S, Takaoka T, Araki M, Ueda Y, Takakura Y. Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine (Phila Pa 1976). 2002. 27:E348–E355.15. Patwardhan AG, Havey RM, Ghanayem AJ, et al. Load-carrying capacity of the human cervical spine in compression is increased under a follower load. Spine (Phila Pa 1976). 2000. 25:1548–1554.
Article16. Hardacker JW, Shuford RF, Capicotto PN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976). 1997. 22:1472–1480.
Article17. Ganju A, Ondra SL, Shaffrey CI. Cervical kyphosis. Tech Orthop. 2003. 17:345–354.
Article18. Miyazaki M, Hymanson HJ, Morishita Y, et al. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine (Phila Pa 1976). 2008. 33:E870–E876.
Article19. Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord. 1999. 12:50–56.
Article20. Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002. 50:229–236.
Article21. Suk KS, Kim KT, Lee SH, Lim YJ, Lee KW. Changes of range of motion and sagittal alignment of the cervical spine after laminoplasty. J Korean Soc Spine Surg. 2005. 12:247–254.
Article22. Song KJ, Lee SK, Song JH, Choi BY. The comparison of multi-level fusion versus one-level fusion to the development of adjacent level degeneration in anterior cervical arthrodesis with PEEK cage and plate augmentation for the degenerative cervical spinal disorders. J Korean Orthop Assoc. 2009. 44:613–618.
Article23. Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976). 2005. 30:2138–2144.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Does Preoperative Cervical Sagittal Alignment And Range of Motion Affect Adjacent Segment Degeneration After Anterior Arthrodesis In Degenerative Cervical Spinal Disorders?: Midterm Follow up Study
- Anterior Cervical Fusion with Cervical Spine Locking Plate System
- The Comparison of Multi-level Fusion versus One-level Fusion to the Development of Adjacent Level Degeneration in Anterior Cervical Arthrodesis with PEEK Cage and Plate Augmentation for the Degenerative Cervical Spinal Disorders
- Efficacy of PEEK Cages and Plate Augmentation in Three-Level Anterior Cervical Fusion of Elderly Patients
- The Efficacy of the Unicortical Screw in the Anterior Cervical Fusion of the Degenerative Cervical Spine Disease