J Korean Soc Spine Surg.
2012 Mar;19(1):25-30. 10.4184/jkss.2012.19.1.25.
Tuberculosis Spondylitis T4-6 with Compression Fracture T5: A Case Report
- Affiliations
-
- 1Department of Rehabilitation, Gachon University of Medicine and Science, Korea. phmed@gilhospital.com
- KMID: 2097862
- DOI: http://doi.org/10.4184/jkss.2012.19.1.25
Abstract
- STUDY DESIGN: Case report
OBJECTIVES
We report a case of a female patient who had only upper back pain without neurological symptoms and was later diagnosed with spine tuberculosis in combination with a compression fracture. SUMMARY OF LITERATURE REVIEW: Spine tuberculosis is the most common type of musculoskeletal tuberculosis. However, the indolent nature of tuberculous bone and joint disease often leads to delayed diagnosis and severe neurologic complications. MATERIAL AND METHODS: A 37-year-old female with only upper back pain for five months was admitted. She had no signs, symptoms or past histories related to tuberculosis. She had taken conservative management, but symptoms persisted.
RESULTS
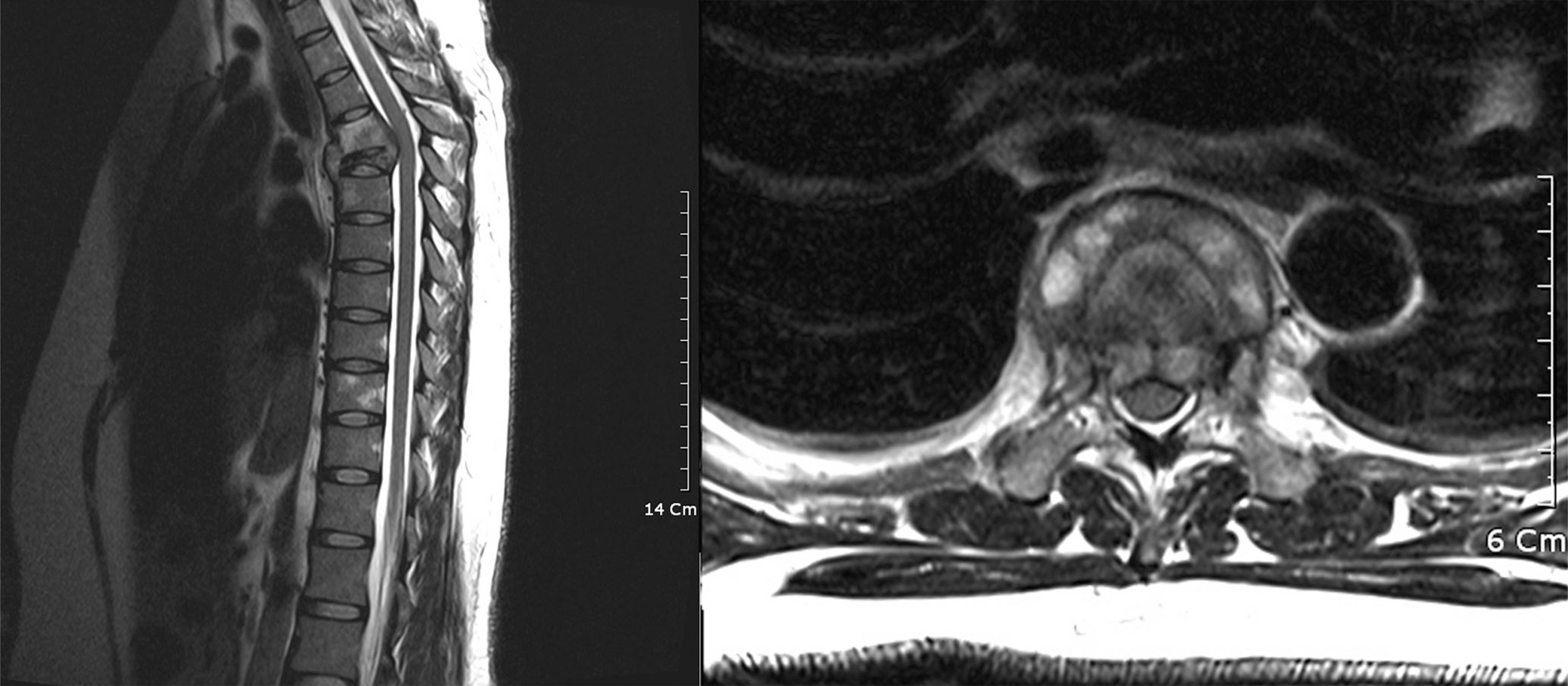
By doing motor and sensory evoked potential studies, we questioned spinal cord jury. Then, we confirmed spine tuberculosis T5 with T4 compression fracture by thoracic magnetic resonance imaging and pathologic findings.
CONCLUSIONS
When a patient presents constant back pain without neurological symptoms, image study and electromyography should be evaluated.
Keyword
MeSH Terms
Figure
Reference
-
1.WHO Library Cataloguing-in-Publication Data. World health statistics. 2010.2.Friedman B. Chemotherapy of tuberculosis of the spine. J Bone Joint Surg Am. 1966. 48:451–74.
Article3.Steven K., Denise IC., Joel AD. Spinal cord medicine. Philadelphia: Lippincott Williams & Wilkins;2002. p. 500–02.4.Du Plessis J., Andronikou S., Theron S., Wieselthaler N., Hayes M. Unusual forms of spinal tuberculosis. Childs Nerv Syst. 2008. 24:453–7.
Article5.Garg RK. Tuberculosis of the central nervous system. Postgrad Med J. 1999. 75:133–40.6.Teo EL., Peh WC. Imaging of tuberculosis of the spine. Singapore Med J. 2004. 45:43–4.7.Skendros P., Kamaria F., Kontopoulos V., Tsitouridis I., Sidiropoulos L. Intradural, extramedullary tuberculoma of the spinal cord as a complication of tuberculous meningitis. Infection. 2003. 31:115–7.8.Cruickshank GS., Johnston RA. Intradural, extramedullary spinal cord compression from tuberculous granuloma. Br J Neurosurg. 1996. 10:93–5.9.Chang DJ., Yoon DM., Kang YS., Yoon KB. Chronic Back Pain Proven to Be Spinal Tuberculosis: A report of 2 cases. Korean J Pain. 2008. 21(74):9.
Article10.Ahn JS., Lee JK., Jeon TS., Kwon YS., Kwak SK. Changes of Kyphotic Angle Following Operative Treatment of Tuberculous Spondylitis. J Korean Soc Spine Surg. 2001. 8:148–55.
Article11.Crenshaw AH. Campbell's Operative Orethopedics. 8th ed.Saint Louis:The CB Mosby company;1992. p. 3802–23.12.Liebenson Craig. Rehabilitation of the spine. 2nd ed.Baltimore: Lippincott Williams & Wilkins;2007. p. 586–611.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Upper Thoracic Spinal Tuberculosis(T2-8) with T5,6 Compression Fracture in Pulmonary Tuberculosis Patient
- Post tetanic thoracic vertebral change
- Multidrug-resistant Tuberculosis Spondylitis: A Case Report
- Thoracic Vertebral Fracture due to Spinal Tuberculosis which was Misdiagnosed as Matastatic Cancer: A Case Report
- Osteoporotic Lumbar Compression Fracture in Patient with Ankylosing Spondylitis Treated with Kyphoplasty