J Korean Soc Spine Surg.
2008 Jun;15(2):106-110. 10.4184/jkss.2008.15.2.106.
Fusion of Pedicular Cleft Using Pedicle Screw Fixation: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Medical Center, Seoul, Korea. ljhos@khmc.or.kr
- 2Department of Orthopedic Surgery, College of Medicine, Kyung Hee University, Seoul, Korea.
- KMID: 2097840
- DOI: http://doi.org/10.4184/jkss.2008.15.2.106
Abstract
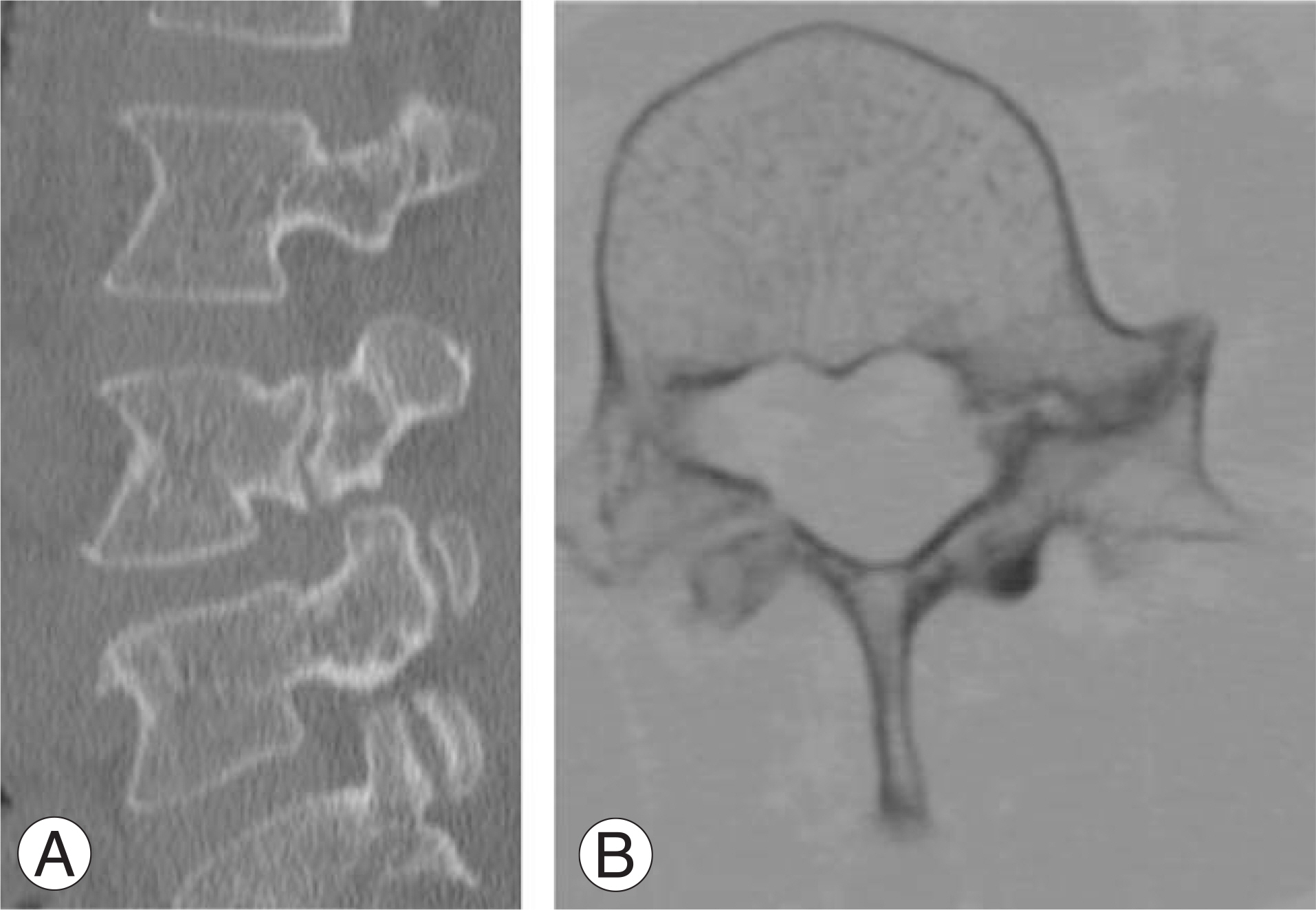
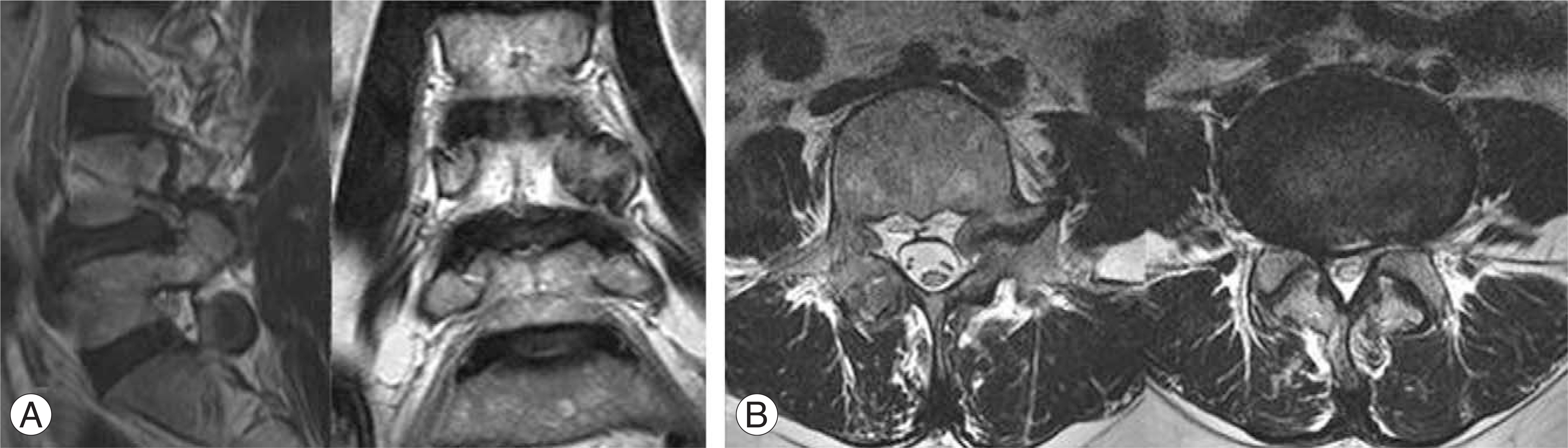
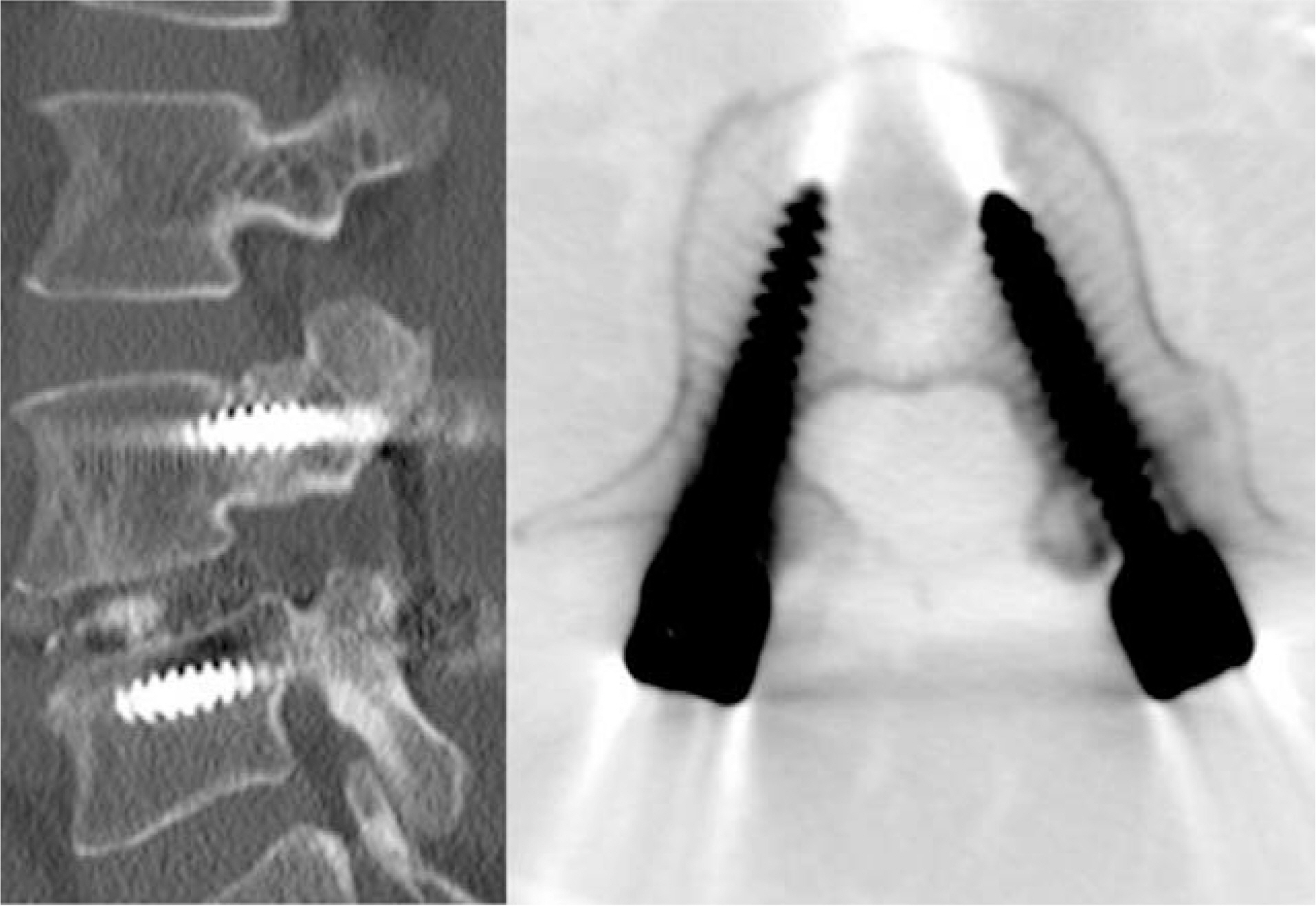
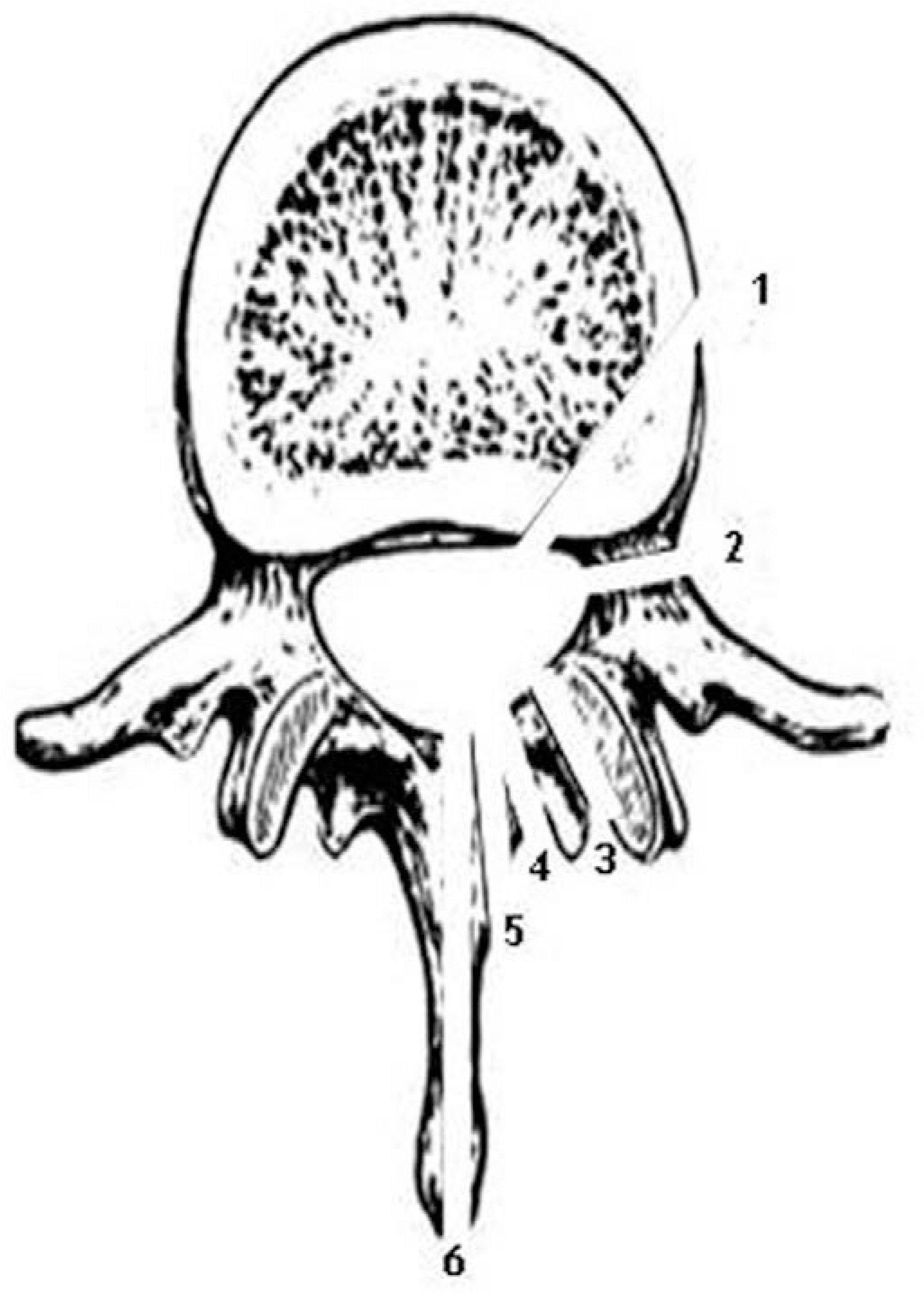
- There is a broad range of lumbar pedicular and neural arch anomalies, with spina bifida occulta and spondylolysis being especially common. It is very rare for a pedicular cleft to be associated with contralateral spondylolysis in the same vertebral segment. We observed L4 spondylolisthesis, clefting of the left L4 hypertrophied pedicle associated with contralateral spondylolysis, and spinal stenosis on a radiographic study of the lumbar spine. Operative treatment was performed, with posterior decompression, partial removal of the hypertrophied pedicle, posterior lumbar interbody fusion using a cage, and posterior instrumentation. The patient's neurologic symptoms resolved after operative treatment. Fusion of the left pedicle cleft was observed on 6-month follow-up CT. We report one case of pedicular cleft fusion using pedicle screw fixation and present a review of the relevant literature.
MeSH Terms
Figure
Reference
-
1). Kalideen JM, Satyapal KS, Bayat F. Case report: pedicular cleft associated with bilateral pars interarticularis defects and transverse process hypoplasia of a fifth lumbar vertebra. Br J Radiol. 1994; 67:1136–1138.2). Merki A. Unilateral retrosomatic vertebral arch cleft L4 associated with spondylolisthesis L5. Z Orthop Ihre Gren-zgeb. 1968; 104:394–398.3). Seegelken K, Schulte GA. Clefts of the vertebral arch (observation of a retrosomatic cleft). Fortschr Geb Ront-genstr Nuklearmed. 1972; 116:473–477.4). Dietemann JL, Macedo R, Medjek L, Babin E, Wack-enheim A. Bilateral pedicular cleft in a patient with neurofibromatosis. Ann Radiol (Paris). 1981; 24:665–667.5). Johansen JG, McCarty DJ, Haughton VM. Retrosomatic clefts: computed tomographic appearance. Radiology. 1983; 148:447–448.
Article6). Barclay-Smith E. Multiple Anomaly in a Vertebral Column. J Anat Physiol. 1911; 45:144–171.7). Stewart TD. The age incidence of neural-arch defects in Alaskan natives, considered from the standpoint of etiology. J Bone Joint Surg Am. 1953; 35:937–950.
Article8). Soleimanpour M, Gregg ML, Paraliticci R. Bilateral retrosomatic clefts at multiple lumbar levels. AJNR Am J Neuroradiol. 1995; 16:1616–1617.9). Ha KY, Park JS. Variant spondylolisthesis with unilateral spondylolysis and contralateral retrosomatic cleft (pedicular defect). J Korean Soc Spine Surg. 1997; 4:370–374.10). Abraham T, Holder L, Silberstein C. The retroisthmic cleft. Scintigraphic appearance and clinical relevance in patients with low back pain. Clin Nucl Med. 1997; 22:161–165.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of the Pedicle Screw Fixation on the Anterior Lumbar Interbody Fusion Using the Freeze - Dried Structural Allograft
- Rate of Pedicle Disruption after Screw Fixation
- Unilateral versus Bilateral Pedide Scrwe Fixation in Lumbar Spinal Fusion
- Comparison between Posterolateral Fusion with Pedicle Screw Fixation and Anterior Interbody Fusion with Pedicle Screw Fixation in Spondylolytic Spondylolisthesis of the Lumbar Spine
- Selective Pedicle Screw Fixation with Long Fusion in the Treatment of Spinal Stenosis with Degenerative Scoliosis