J Korean Soc Transplant.
2009 Sep;23(2):172-176. 10.4285/jkstn.2009.23.2.172.
Invasive Gastrointestinal and Cutaneous Mucormycosis in Deceased Donor Small Bowel Transplantation: Case Report and Review of Literature
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunwan University School of Medicine, Seoul, Korea. sukkoo.lee@samsung.com
- KMID: 2097087
- DOI: http://doi.org/10.4285/jkstn.2009.23.2.172
Abstract
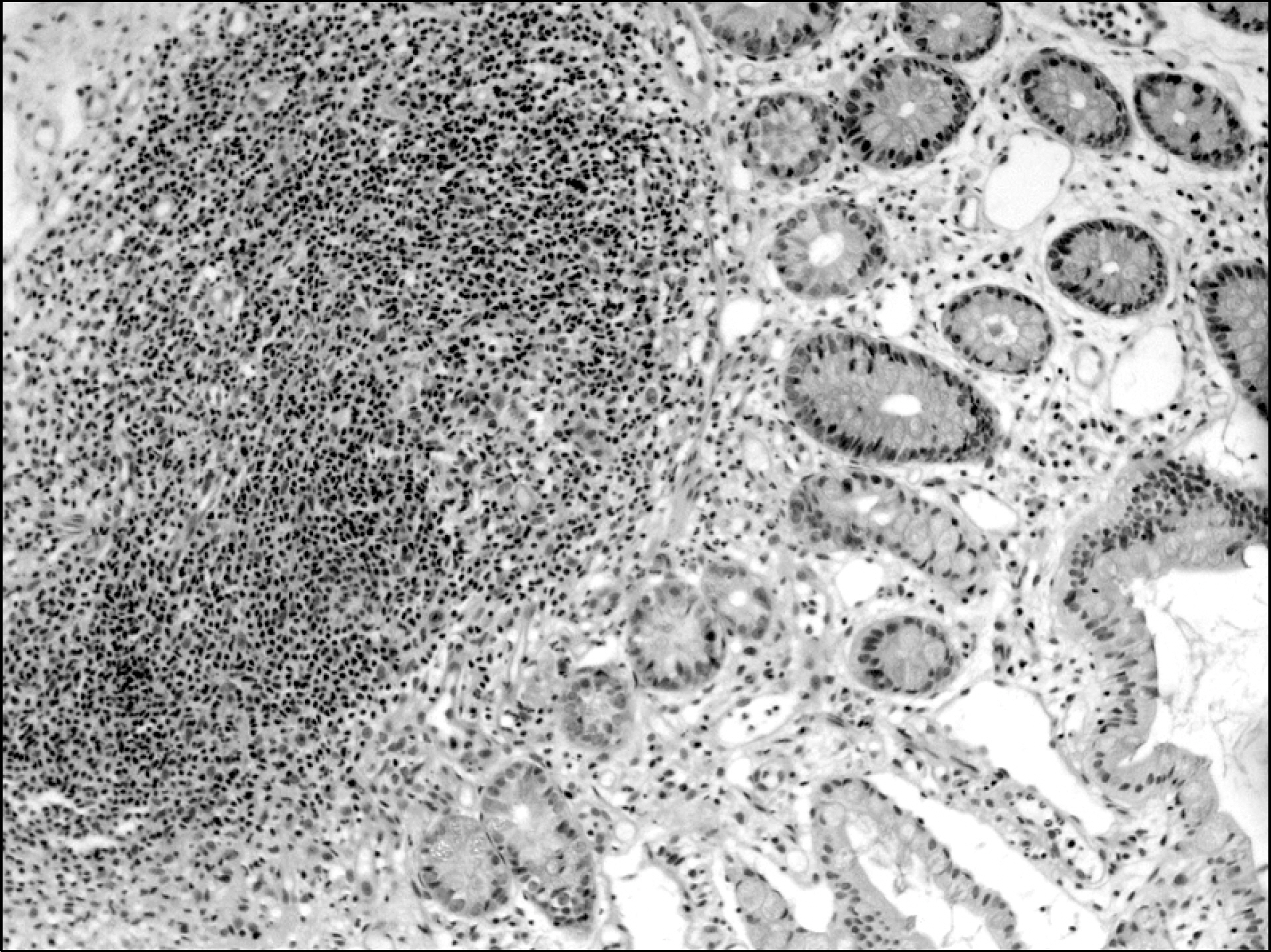
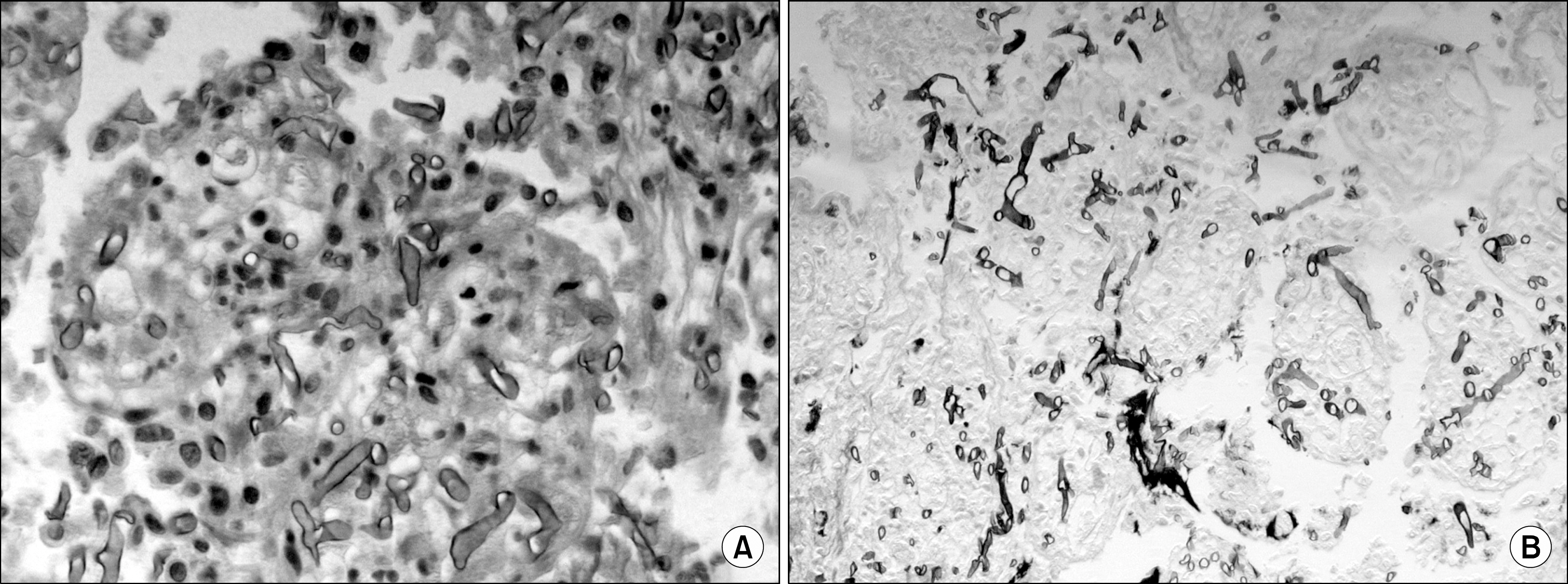
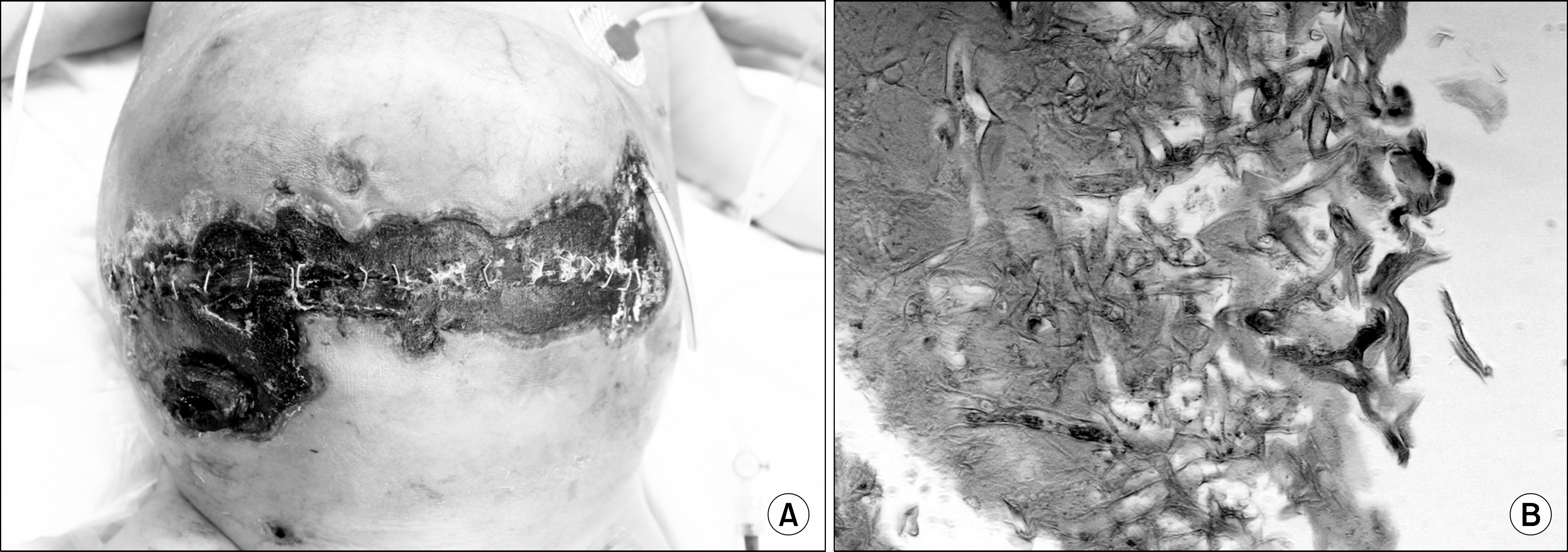
- Fungal infection is an uncommon complication after small bowel transplantation. We present a rare form of mucormycosis found in the small bowel graft and in the skin of a recipient. We reviewed chart data and performed MEDLINE searches and found that this case was the first to report 2 kinds of mucormycosis to be found after organ transplantation. The patient was a 12 month old female baby who underwent small bowel transplantation due to short bowel syndrome. After 12 days she experienced acute cellular rejection which responded to steroid. 6 days later due to sustained fever, poor feeding and abdominal distention endoscopic biopsy was done which revealed mucormycosis. Antifungal treatment with lipo-amphotericin B was initiated, yet there was no improvement of clinical symptoms. On the 23 post operative day a black eschar developed on the incision site of the skin and biopsy was done which revealed cutaneous mucormycosis. Infected skin debridement and graftectomy was done but our patient expired because of septic shock.
MeSH Terms
Figure
Cited by 1 articles
-
Colonic Mucormycosis Mimicking Ischemic Colitis in Kidney Transplant Recipient
Hyun Woo Kim, Young Min Yoon, Mi Ja Lee, Nam Gyu Choi, Sung Pyo Moon, Na Ra Yoon, Sun Ae Han, Hyung Nam Kim, Jun Hyung Lee, Da Yeong Kang, Hee Jung Ahn, Byung Chul Shin, Hyun Lee Kim, Jong Hoon Chung
J Korean Soc Transplant. 2016;30(2):98-102. doi: 10.4285/jkstn.2016.30.2.98.
Reference
-
1). Tedder M, Spratt JA, Anstadt MP, Hegde SS, Tedder SD, Lowe JE. Pulmonary mucormycosis: results of medi-cal and surgical therapy. Ann Thorac Surg. 1994; 57:1044–50.
Article2). Meyer RD, Rosen P, Armstong D. Phycomycosis com-plicating leukemia and lymphoma. Ann Intern Med. 1972; 77:981–9.
Article3). Wajszczuk CP, Dummer JS, Ho M, van Thiel DH, Starzl TE, Iwatsuki S, et al. Fungal infections in the liver transplants. Transplantation. 1985; 40:347–53.4). Castaldo P, Stratta RJ, Wood RP, Markin RS, Patil KD, Shaefer MS, et al. Clinical spectrum of fungal infections after orthototic liver transplantation. Arch Surg. 1991; 126:149–56.5). Jee MS, Choi HJ, Choi JH, Sung KJ, Moon KC, Koh JK. A case of mucormycosis involving the skin in renal transplant recipient. Korean J Dermatol. 2003; 41:501–4.6). Almyroudis NG, Sutton DA, Linden P, Rinaldi MG, Fung J, Kusne S. Zygomycosis in solid organ transplant recipients in a tertiary transplant center and review of the literature. Am J Transplant. 2006; 6:2365–74.
Article7). Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and out-come of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005; 41:634–53.
Article8). Kontoyiannis DP, Lionakis MS, Lewis RE, Chamilos G, Healy M, Perego C, et al. Zygomycosis in a tertiary-care cancer center in the era of Aspergillus-active antifungal therapy: a case-control observational study of 27 recent cases. J Infect Dis. 2005; 191:1350–60.9). Singh N, Gayowski T, Singh J, Yu VL. Invasive gastro-intestinal zygomycosis in a liver transplant recipient: case report and review of zygomycosis in solid organ transplant recipients. Clin Infect Dis. 1995; 20:617–20.10). Winkler S, Susani S, Willnger B, Apsner R, Rosenkranz AR, Potzi R, et al. Gastric mucormycosis due to due to Rhizopus oryzae in a renal transplant recipient. J Clin Microbiol. 1996; 34:2585–7.11). Maertens J, Demuynck H, Verbeken EK, Zachee P, Verhoef GE, Vandenberghe P, et al. Mucormycosis in al-logenic bone marrow transplant recipient: report of five cases and review of the role of iron overload in the pathogenesis. Bone Marrow transplant. 1999; 24:307–12.12). Morrison VA, McGlave PB. Mucormycosis in the BMT population. Bone Marrow Transplant. 1993; 11:383–8.13). Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000; 13:236–301.
Article14). van Burik JA, Hare RS, Solomon HF, Corrado ML, Kontoyiannis DP. Posaconazole is effective as salvage therapy in zygomycosis: a retrospective summary 91 cases. Clin Infect Dis. 2006; 42:e61–5.15). Greenberg RN, Mullane K, van Burik JA, Raad I, Abzug MJ, Anstead G, et al. Posaconazole as salvage therapy of zygomycosis. Antimicrob Agent Chemother. 2006; 50:126–33.16). Sung TY, Kim YS, Ahn HJ, Lee YH, Ju MK, Hyung WJ. Gastric Perforation Associated with Vascular Invasive Mucormycosis in a Renal Transplant Recipient. J Korean Surg Soc. 2006; 71:376–8.17). Kim SH, Kim KB, Choo YM, Chang WI, Kim YS, Lee DG, et al. A Case of Disseminated Mucormycosis after Allogenic Bone Marrow Transplantation. Korean J Infect Dis. 2000; 32:73–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deceased donor liver transplantation performed one week after small bowel resection for complicated umbilical hernia: a case report
- A Case of Cutaneous Mucormycosis Mimicking Sporotrichosis
- Current Status of Deceased Donor Organ Recovery and Sharing in Korea
- Primary Cutaneous Mucormycosis Associated with Trauma
- A Case of Cutaneous Mucormycosis