Korean J Hematol.
2005 Dec;40(4):274-277. 10.5045/kjh.2005.40.4.274.
Peripheral Blood Eosinophilia: An Unusual Presentation of Bone Marrow Involvement in a Patient with Relapsed Thyroid Papillary Carcinoma
- Affiliations
-
- 1Department of Internal Medicine, Korea University Medical Center, Seoul, Korea. kbs0309@korea.ac.kr
- 2Department of Laboratory Medicine, Korea University Medical Center, Seoul, Korea.
- KMID: 2083467
- DOI: http://doi.org/10.5045/kjh.2005.40.4.274
Abstract
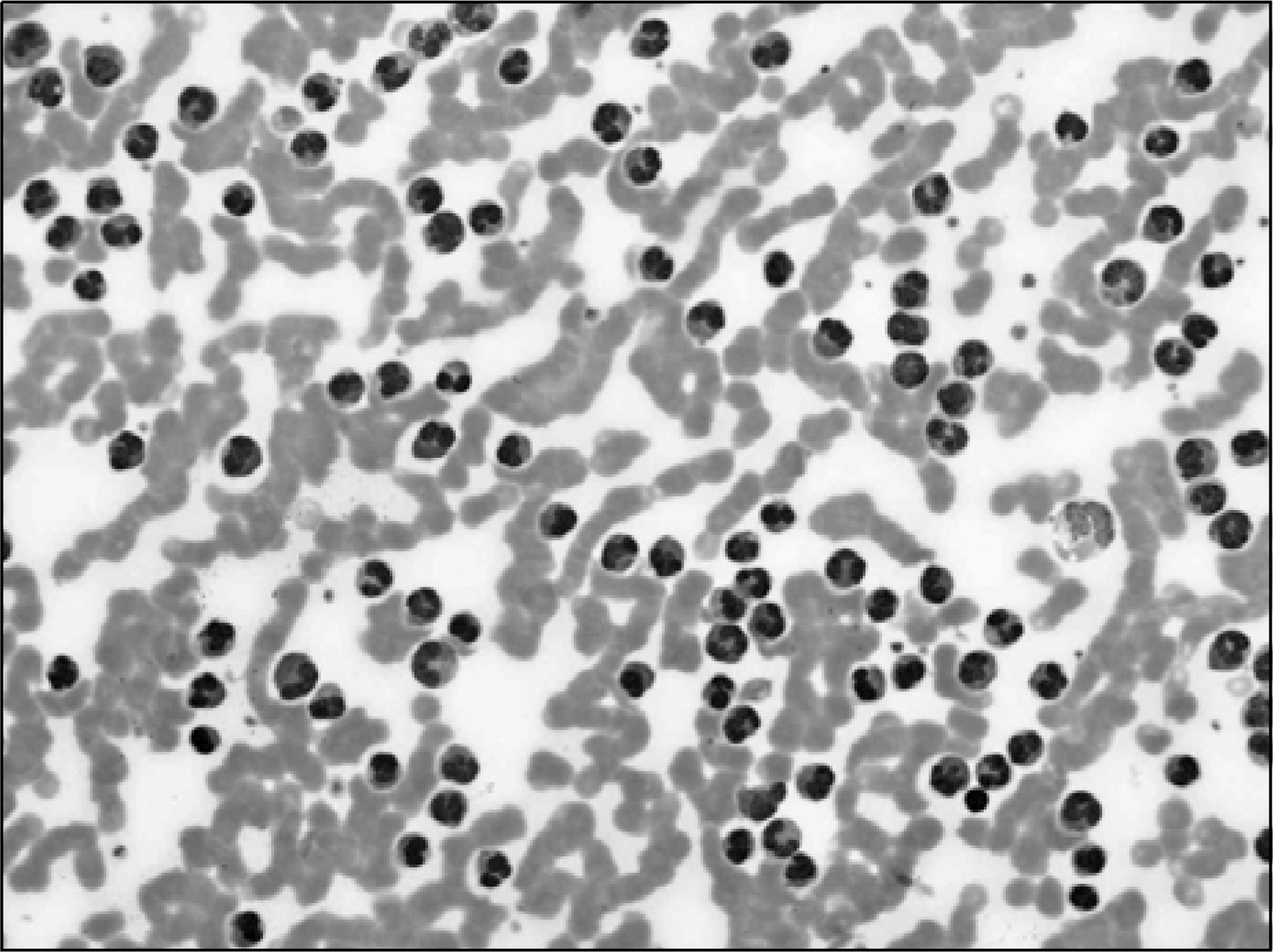
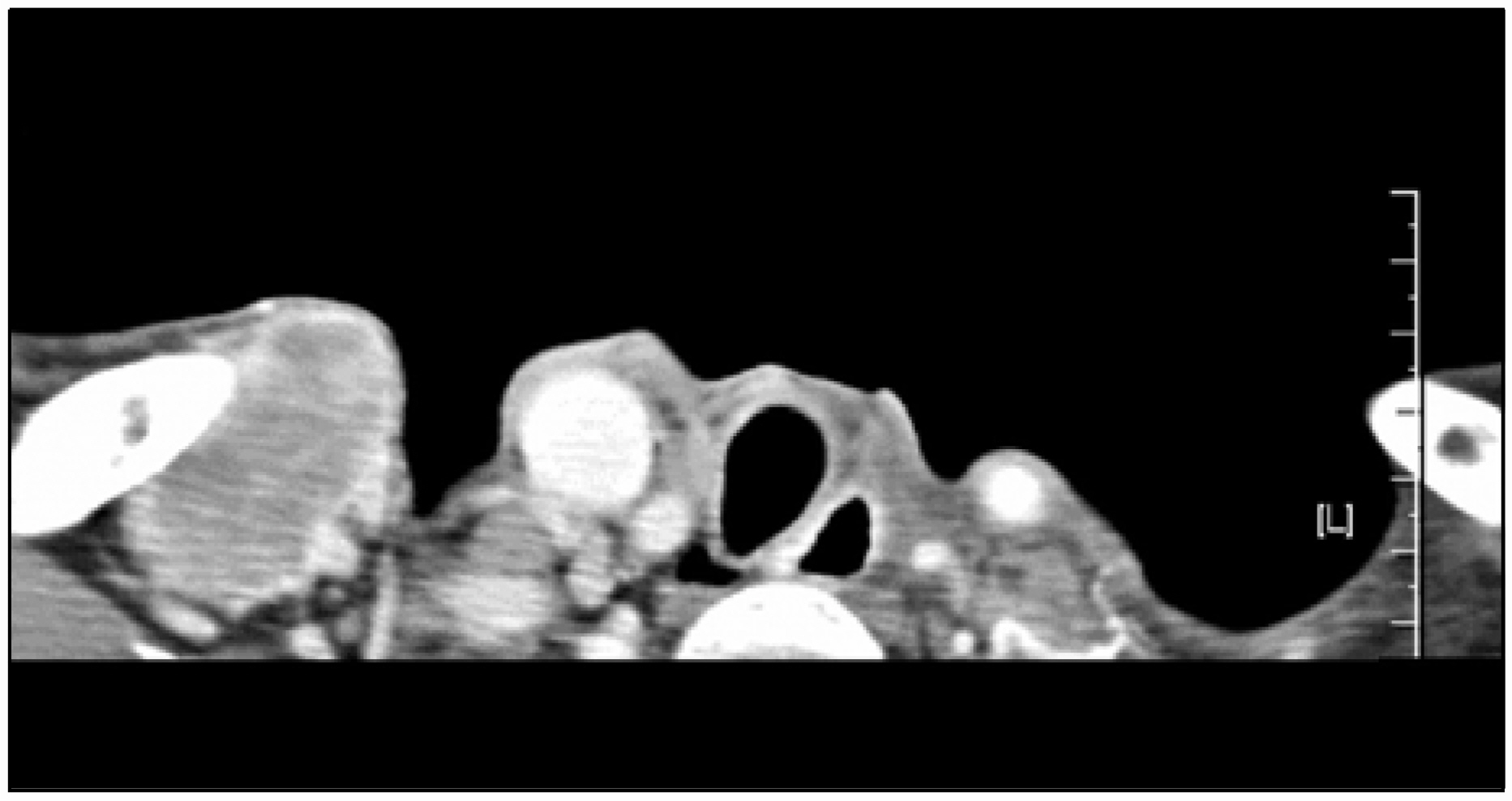
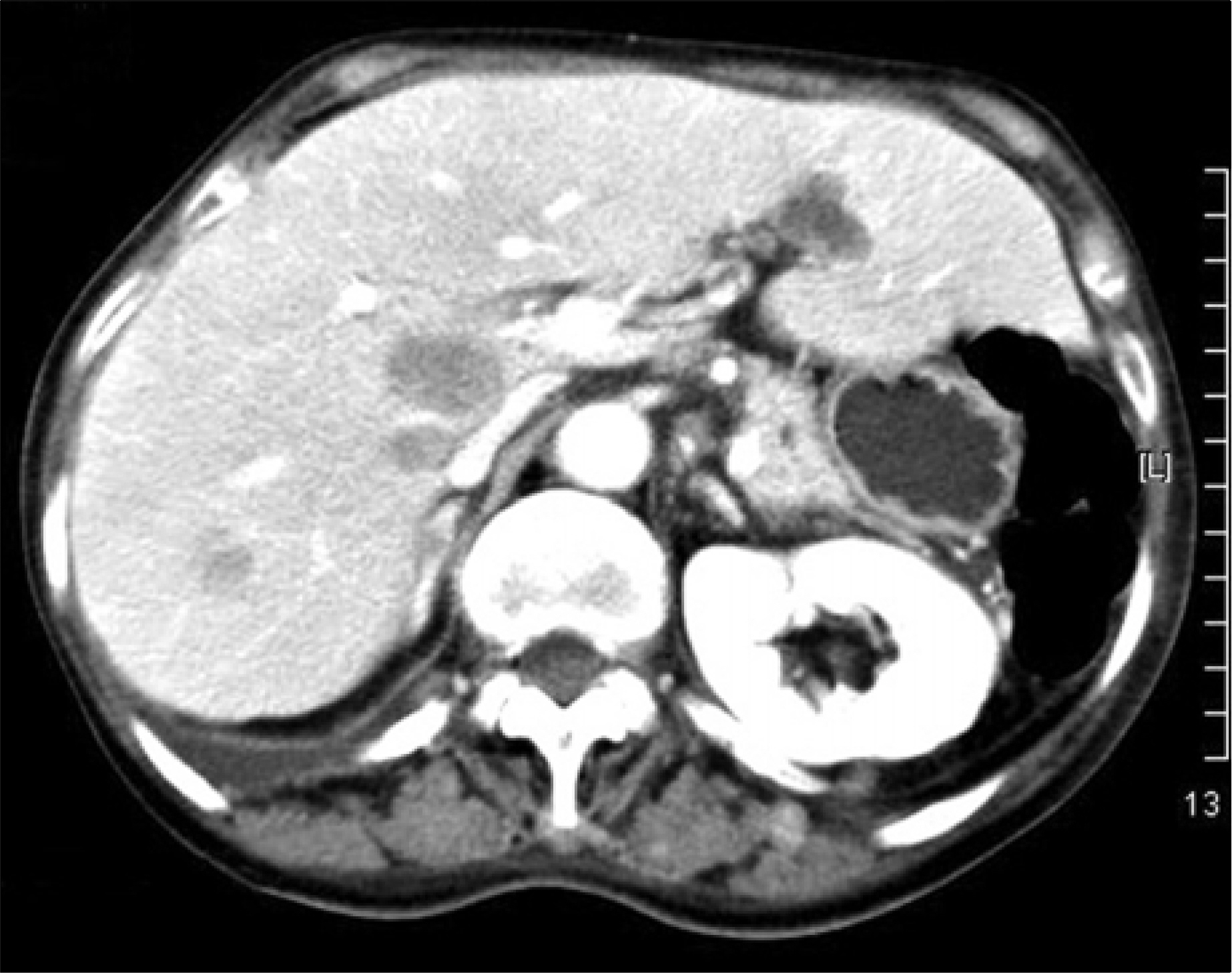
- Peripheral blood eosinophilia is a well-known paraneoplastic manifestation, but its underlying mechanism is still unclear. Bone marrow metastasis may be a cause of malignancy-associated eosinophilia. However, there is limited evidence of the relationship between bone marrow metastasis and eosinophilia. Herein, we present a unique case of peripheral blood eosinophilia associated with bone marrow invasion in a patient having a history of papillary thyroid carcinoma. A 68-year old woman showed peripheral blood eosinophilia (91,525/mm3). Since the time she was initially diagnosed as having papillary thyroid carcinoma, eosinophilia had never been found and the other causes of eosinophilia were excluded. A bone marrow study revealed cancer cell infiltration; multiple lymphadenopathies and liver metastasis were also detected. We treated her with steroid; however, her eosinophilia did not respond to steroid and the patient died due to disease progression. Although peripheral blood eosinophilia and bone marrow metastasis are rare findings in patients with papillary thyroid carcinoma, we suggest that eosinophilia might be a sign of the bone marrow metastasis of papillary thyroid carcinoma.
Keyword
MeSH Terms
Figure
Reference
-
1). Devita VT, Samuel H, Rosenberg SA. Cancer principles and practice of oncology. 7th ed.Philadelphia, Pa: Lippincott Willwams & Wilkins;2005. p. 2194.2). Haskell CM, Berek JS. Cancer treatment. 5th ed.Philadelphia: W.B. Saunders Company;2001. p. 249.3). Matsumoto S, Tamai T, Yanagisawa K, Kawamura S, Fujita S. Lung cancer with eosinophilia in the peripheral blood and the pleural fluid. Intern Med. 1992; 31:525–9.
Article4). Reddy SS, Hyland RH, Alison RE, Sturgeon JF, Hutcheon MA. Tumor-associated peripheral eosinophilia: two unusual cases. J Clin Oncol. 1984; 2:1165–9.
Article5). Yuen BH, Reyes CV, Rawal PA, Sosman J, Jensen J. Severe eosinophilia and hepatocellular carcinoma: an unusual association. Diagn Cytopathol. 1995; 13.
Article6). Hirata J, Koga T, Nishimura J, Ibayashi H. Pancreatic carcinoma associated with marked eosinophilia: a case report. Eur J Haematol. 1987; 39:462–6.
Article7). Balducci L, Chapman SW, Little DD, Hardy CL. Paraneoplastic eosinophilia. Report of a case with in vitro studies of hemopoiesis. Cancer. 1989; 64:2250–3.8). Van Crombrugge P, Pauwels R, Van der Straeten M. Thyroid carcinoma and eosinophilia. Ann Clin Res. 1983; 15:128–30.9). Miller WM, Adcook KJ, Moniot AL, Raymond LW, Hutcheson J, Elliott RC. Progressive hypereosinophilia with lung nodules due to thyroid carcinoma. Chest. 1997; 71:789–91.
Article10). Jung WY, Yang WI, Park CS. A case of sclerosing mucoepidermoid thyroid carcinoma with eosinophilia (SMECE). Korean J Head & Neck Oncol. 2001; 17:48–51.11). Haldane JH, Kapoor H, Morris J. Severe eosinophilia associated with a malignant islet cell tumour. CMAJ. 1989; 140:1061–3.12). Lowe D, Jorizzo J, Hutt MS. Tumour-associated eosinophilia: a review. J Clin Pathol. 1981; 34:1343–8.
Article13). Chang WC, Liaw CC, Wang PN, Tsai YH, Hsueh S. Tumor-associated hypereosinophilia: report of four cases. Changgeng Yi Xue Za Zhi. 1996; 19:66–70.14). Voutilainen PE, Multanen MM, Leppaniemi AK, Haglund CH, Haapiainen RK, Franssila KO. Prognosis after lymph node recurrence in papillary thyroid carcinoma depends on age. Thyroid. 2001; 11:953–7.
Article15). Chung JP, Nam DK, Lee SJ. A clinical study on eosinophilia; with a report of 5 cases of hypereosinophilic syndrome. Korean J Hematol. 1988; 23:127–37.16). Haskell CM, Berek JS. Cancer treatment:. 5th ed.Philadelphia: W.B. Saunders company;2001. p. 1559.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- A Case of Cystic Lymph Node Metastasis from Thyroid Papillary Microcarcinoma
- Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- A case of myelodysplastic syndrome with marked eosinophilia showing favorable prognosis
- A Case of Ectopic Thyroid Papillary Carcinoma with Incidental Papillary Thyroid Microcarcinoma