J Korean Soc Radiol.
2015 Nov;73(5):292-299. 10.3348/jksr.2015.73.5.292.
Symptomatic Isolated Middle Cerebral Artery Dissection: High Resolution MR Findings
- Affiliations
-
- 1Department of Radiology, Chonbuk National University Medical School, Jeonju, Korea. kwak8140@jbnu.ac.kr
- 2Research Institute of Clinical Medicine, Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2079563
- DOI: http://doi.org/10.3348/jksr.2015.73.5.292
Abstract
- PURPOSE
To perform high-resolution magnetic resonance imaging (HRMRI) and determine clinical features of patients with acute symptomatic middle cerebral artery (MCA) dissection.
MATERIALS AND METHODS
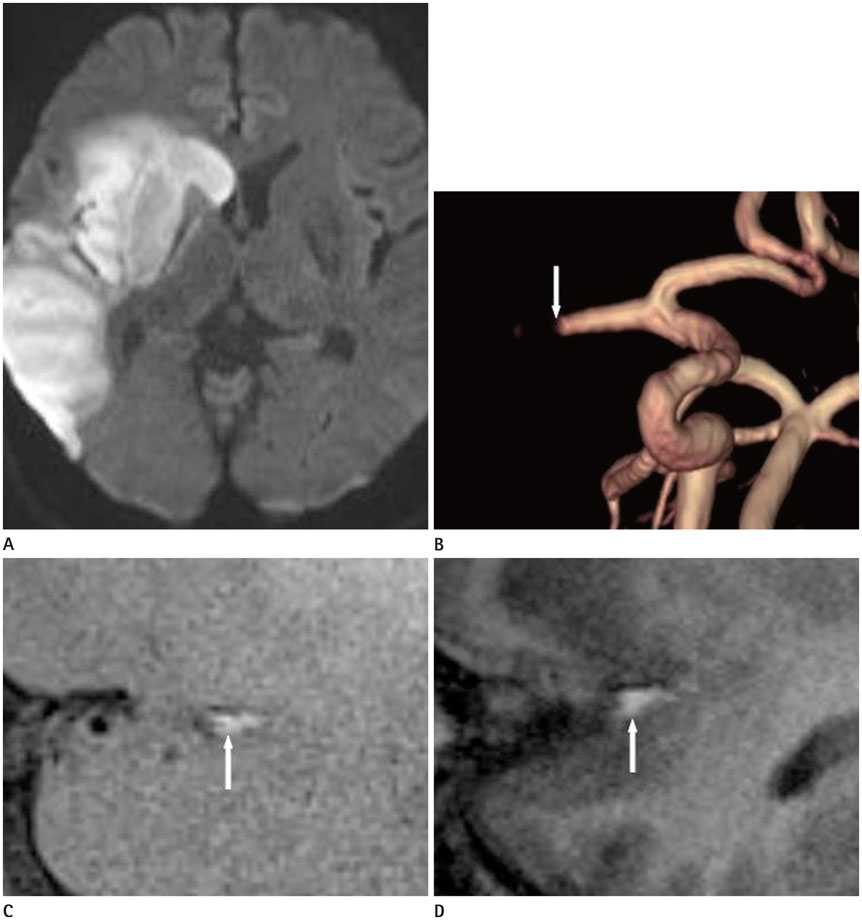
Thirteen patients with acute symptomatic MCA dissection underwent HRMRI within 3 days after initial clinical onset. They also underwent routine brain MR imaging. HRMRI examinations included time-of-flight MR angiography (MRA), T2-weighted, T1-weighted, proton-density-weighted, and three-dimensional magnetization-prepared rapid acquisition gradient-echo (MPRAGE) sequences. Conventional angiography and MRA were used as reference standard to establish the diagnosis of MCA dissection. The angiographic findings and HRMRI findings such as intimal flap, double lumen, and intramural hematoma were analyzed in this study.
RESULTS
All patients presented cerebral ischemia (median National Institutes of Health Stroke Scale score = 4, range = 0-18). String sign was seen on MRA in seven patients. However, double lumen was seen in all patients on HRMRI by intimal flap. High signal lesion on MPRAGE sequences around the dissection lumen due to intramural hematoma was seen in three patients.
CONCLUSION
HRMRI can be used to easily detect the wall structure of MCA such as the intimal flap and double lumen in patients with acute symptomatic MCA dissection. MPRAGE can detect hemorrhage in false lumen of MCA dissection.
MeSH Terms
Figure
Reference
-
1. Li S, Yan B, Kaye A, Mitchell P, Dowling R, Collins M, et al. Prognosis of intracranial dissection relates to site and presenting features. J Clin Neurosci. 2011; 18:789–793.2. Kurino M, Yoshioka S, Ushio Y. Spontaneous dissecting aneurysms of anterior and middle cerebral artery associated with brain infarction: a case report and review of the literature. Surg Neurol. 2002; 57:428–436. discussion 436-4383. Vertinsky AT, Schwartz NE, Fischbein NJ, Rosenberg J, Albers GW, Zaharchuk G. Comparison of multidetector CT angiography and MR imaging of cervical artery dissection. AJNR Am J Neuroradiol. 2008; 29:1753–1760.4. Lee HO, Kwak HS, Chung GH, Hwang SB. Diagnostic usefulness of high resolution cross sectional MRI in symptomatic middle cerabral arterial dissection. J Korean Neurosurg Soc. 2011; 49:370–372.5. Bachmann R, Nassenstein I, Kooijman H, Dittrich R, Stehling C, Kugel H, et al. High-resolution magnetic resonance imaging (MRI) at 3.0 Tesla in the short-term follow-up of patients with proven cervical artery dissection. Invest Radiol. 2007; 42:460–446.6. Chung GH, Kwak HS, Hwang SB, Jin GY. High resolution MR imaging in patients with symptomatic middle cerebral artery stenosis. Eur J Radiol. 2012; 81:4069–4074.7. Li ML, Xu WH, Song L, Feng F, You H, Ni J, et al. Atherosclerosis of middle cerebral artery: evaluation with high-resolution MR imaging at 3T. Atherosclerosis. 2009; 204:447–452.8. Ryu CW, Jahng GH, Kim EJ, Choi WS, Yang DM. High resolution wall and lumen MRI of the middle cerebral arteries at 3 tesla. Cerebrovasc Dis. 2009; 27:433–442.9. Xu WH, Li ML, Gao S, Ni J, Zhou LX, Yao M, et al. In vivo high-resolution MR imaging of symptomatic and asymptomatic middle cerebral artery atherosclerotic stenosis. Atherosclerosis. 2010; 212:507–511.10. Dziewas R, Konrad C, Dräger B, Evers S, Besselmann M, Lüdemann P, et al. Cervical artery dissection--clinical features, risk factors, therapy and outcome in 126 patients. J Neurol. 2003; 250:1179–1184.11. Asaithambi G, Saravanapavan P, Rastogi V, Khan S, Bidari S, Khanna AY, et al. Isolated middle cerebral artery dissection: a systematic review. Int J Emerg Med. 2014; 7:44.12. Ohkuma H, Suzuki S, Shimamura N, Nakano T. Dissecting aneurysms of the middle cerebral artery: neuroradiological and clinical features. Neuroradiology. 2003; 45:143–148.13. Ohkuma H, Suzuki S, Kikkawa T, Shimamura N. Neuroradiologic and clinical features of arterial dissection of the anterior cerebral artery. AJNR Am J Neuroradiol. 2003; 24:691–699.14. Ota H, Yarnykh VL, Ferguson MS, Underhill HR, Demarco JK, Zhu DC, et al. Carotid intraplaque hemorrhage imaging at 3.0-T MR imaging: comparison of the diagnostic performance of three T1-weighted sequences. Radiology. 2010; 254:551–556.15. Turan TN, Bonilha L, Morgan PS, Adams RJ, Chimowitz MI. Intraplaque hemorrhage in symptomatic intracranial atherosclerotic disease. J Neuroimaging. 2011; 21:e159–e161.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Usefulness of High Resolution Cross Sectional MRI in Symptomatic Middle Cerabral Arterial Dissection
- Childhood Primary Angiitis of the Central Nervous System Presenting as Isolated Middle Cerebral Artery Dissection
- Various treatment modalities for isolated intracranial middle cerebral arterial dissection with progressive ischemic symptoms: 2 case reports of endovascular stent and bypass surgery
- Bilateral Vertebral Artery Dissection Involving the Basilar Artery: the Role of High-Resolution MR Imaging
- Post-Traumatic Middle Cerebral Artery Dissection: A Case Report