Korean J Pain.
2013 Oct;26(4):396-400. 10.3344/kjp.2013.26.4.396.
Computed Tomography (CT) Simulated Fluoroscopy-Guided Transdiscal Approach in Transcrural Celiac Plexus Block
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. paindrsuh@gmail.com
- KMID: 2074050
- DOI: http://doi.org/10.3344/kjp.2013.26.4.396
Abstract
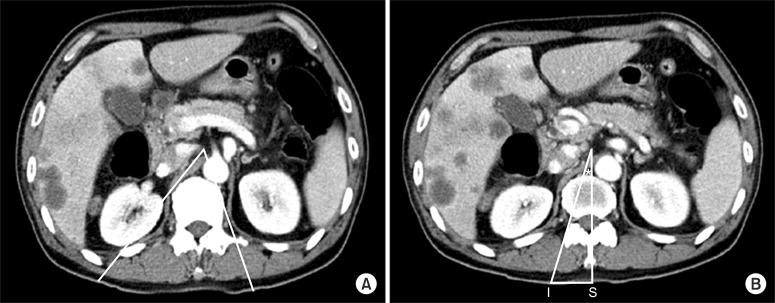
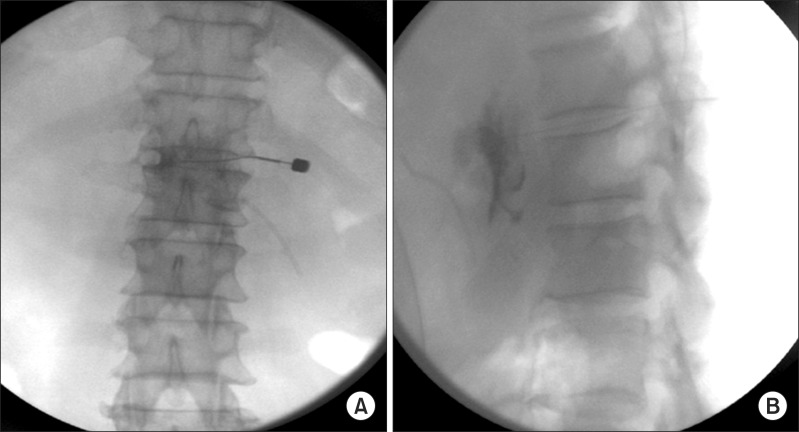
- Conventional transcrural CPB via the "walking off" the vertebra technique may injure vital organs while attempting to proximally spread injectate around the celiac plexus. Therefore, we attempted the CT-simulated fluoroscopy-guided transdiscal approach to carry out transcrural CPB in a safer manner, spreading the injectate more completely and closely within the celiac plexus area. A 54-year-old male patient with pancreatic cancer suffered from severe epigastric pain. The conventional transcrural approach was simulated, but the needle pathway was impeded by the kidney on the right side and by the aorta on the left side. After simulating the transdiscal pathway through the T11-12 intervertebral disc, we predetermined the optimal insertion point (3.6 cm from the midline), insertion angle (18 degrees), and advancement plane, as well as the proper depth. With the transdiscal approach, we successfully performed transcrural CPB within a narrow angle, and the bilateral approach was not necessary as we were able to achieve the bilateral spread of the injectate with the single approach.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Factors associated with successful response to neurolytic celiac plexus block in patients with upper abdominal cancer-related pain: a retrospective study
Hyun-Jung Kwon, Kyunghwan Jang, Jeong-Gil Leem, Jin-Woo Shin, Doo-Hwan Kim, Seong-Soo Choi
Korean J Pain. 2021;34(4):479-486. doi: 10.3344/kjp.2021.34.4.479.Splanchnic nerve neurolysis via the transdiscal approach under fluoroscopic guidance: a retrospective study
Zhenhua Cai, Xiaolin Zhou, Mengli Wang, Jiyu Kang, Mingshuo Zhang, Huacheng Zhou
Korean J Pain. 2022;35(2):202-208. doi: 10.3344/kjp.2022.35.2.202.
Reference
-
1. Bahn BM, Erdek MA. Celiac plexus block and neurolysis for pancreatic cancer. Curr Pain Headache Rep. 2013; 17:310. PMID: 23299904.
Article2. Kim WH, Lee CJ, Sim WS, Shin BS, Ahn HJ, Lim HY. Anatomical analysis of computed tomography images for determining the optimal oblique fluoroscope angle for percutaneous coeliac plexus block. J Int Med Res. 2011; 39:1798–1807. PMID: 22117980.
Article3. Moore DC, Bush WH, Burnett LL. Celiac plexus block: a roentgenographic, anatomic study of technique and spread of solution in patients and corpses. Anesth Analg. 1981; 60:369–379. PMID: 7195158.4. Ischia S, Luzzani A, Ischia A, Faggion S. A new approach to the neurolytic block of the coeliac plexus: the transaortic technique. Pain. 1983; 16:333–341. PMID: 6194498.
Article5. Ischia S, Ischia A, Polati E, Finco G. Three posterior percutaneous celiac plexus block techniques. A prospective, randomized study in 61 patients with pancreatic cancer pain. Anesthesiology. 1992; 76:534–540. PMID: 1550278.
Article6. Garcia-Eroles X, Mayoral V, Montero A, Serra J, Porta J. Celiac plexus block: a new technique using the left lateral approach. Clin J Pain. 2007; 23:635–637. PMID: 17710015.
Article7. De Cicco M, Matovic M, Bortolussi R, Coran F, Fantin D, Fabiani F, et al. Celiac plexus block: injectate spread and pain relief in patients with regional anatomic distortions. Anesthesiology. 2001; 94:561–565. PMID: 11379673.8. Loukas M, Klaassen Z, Merbs W, Tubbs RS, Gielecki J, Zurada A. A review of the thoracic splanchnic nerves and celiac ganglia. Clin Anat. 2010; 23:512–522. PMID: 20235178.
Article9. Hilgier M, Rykowski JJ. One needle transcrural celiac plexus block. Single shot or continuous technique, or both. Reg Anesth. 1994; 19:277–283. PMID: 7947429.10. Noble M, Gress FG. Techniques and results of neurolysis for chronic pancreatitis and pancreatic cancer pain. Curr Gastroenterol Rep. 2006; 8:99–103. PMID: 16533471.
Article11. Yang IY, Oraee S, Viejo C, Stern H. Computed tomography celiac trunk topography relating to celiac plexus block. Reg Anesth Pain Med. 2011; 36:21–25. PMID: 21455084.
Article