Korean J Radiol.
2015 Apr;16(2):325-333. 10.3348/kjr.2015.16.2.325.
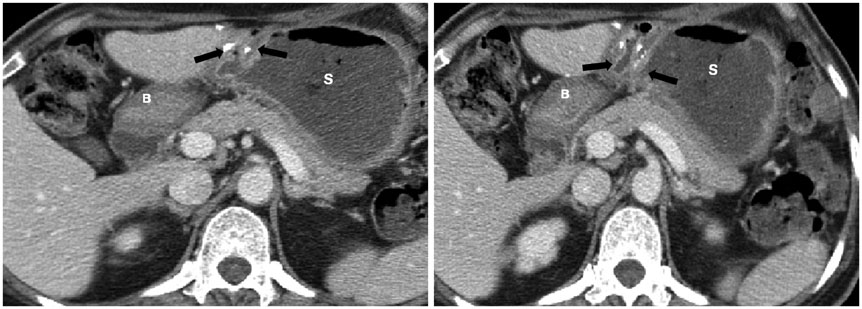
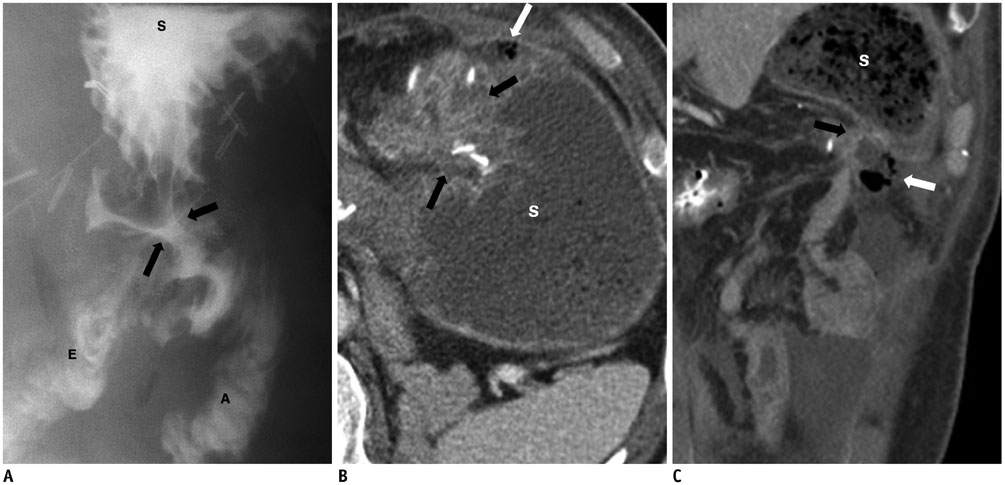
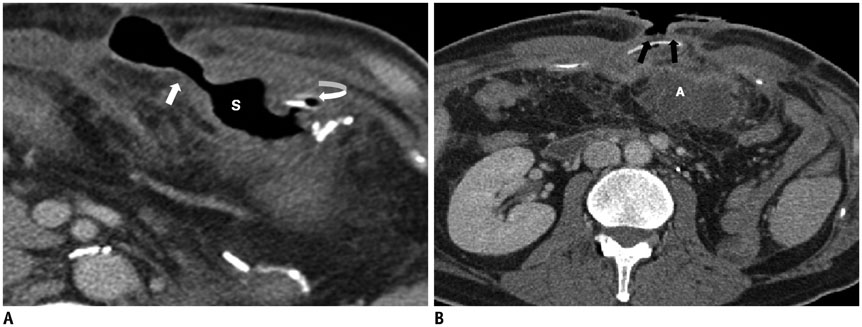
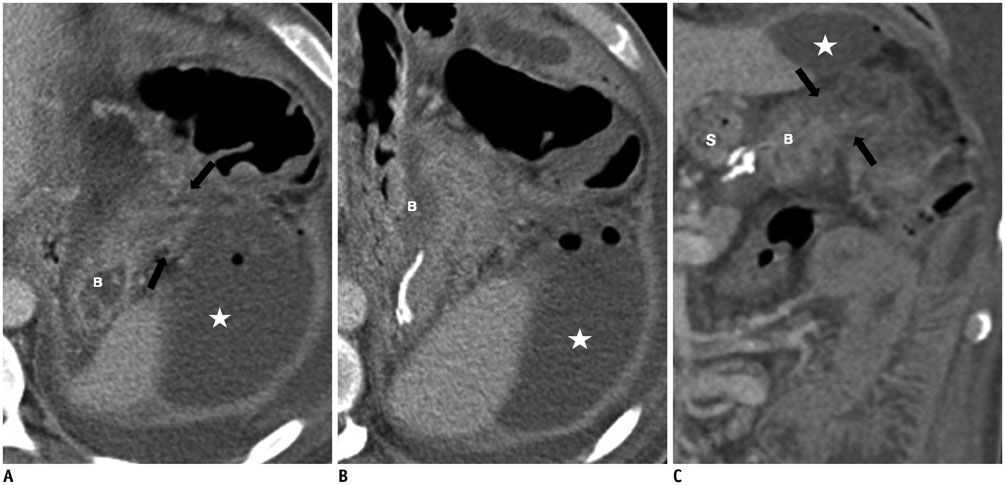
Mini-Gastric Bypass to Control Morbid Obesity and Diabetes Mellitus: What Radiologists Need to Know
- Affiliations
-
- 1Department of Radiology, Chung-Ang University Hospital, Seoul 156-755, Korea.
- 2Department of Radiology, Soonchunhyang University Seoul Hospital, Seoul 140-743, Korea. hongses@schmc.ac.kr
- 3Department of Surgery, Soonchunhyang University Seoul Hospital, Seoul 140-743, Korea.
- KMID: 2070176
- DOI: http://doi.org/10.3348/kjr.2015.16.2.325
Abstract
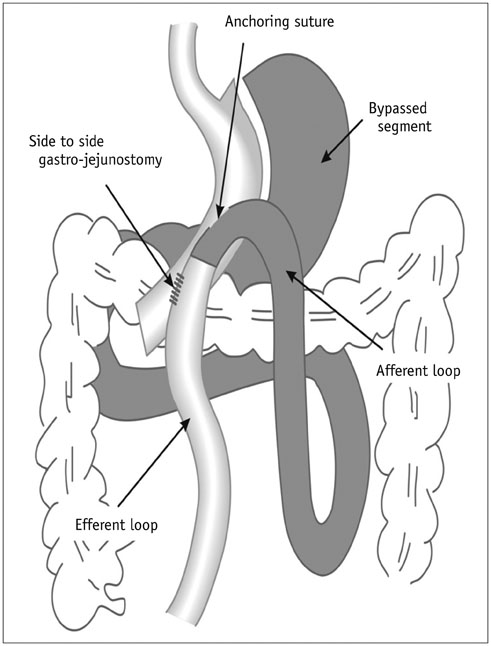
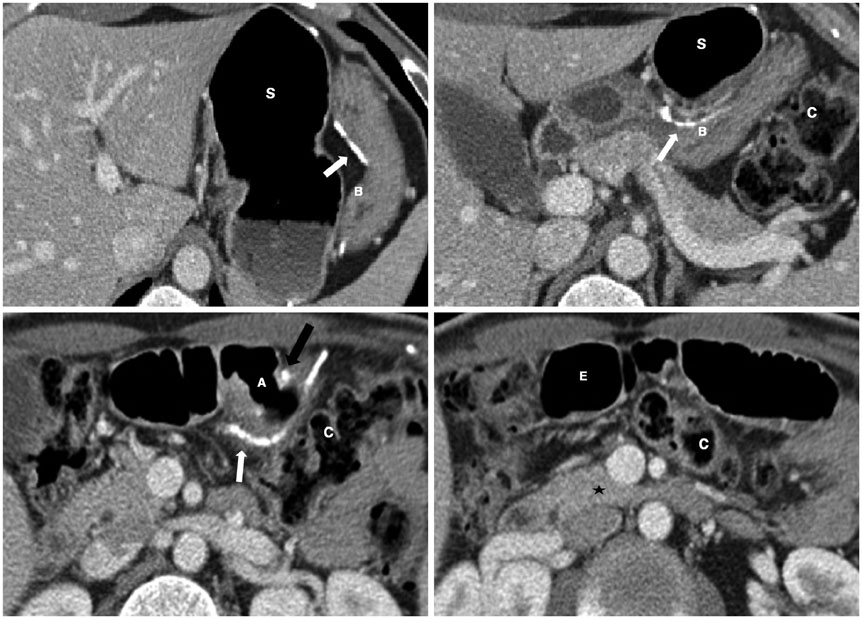
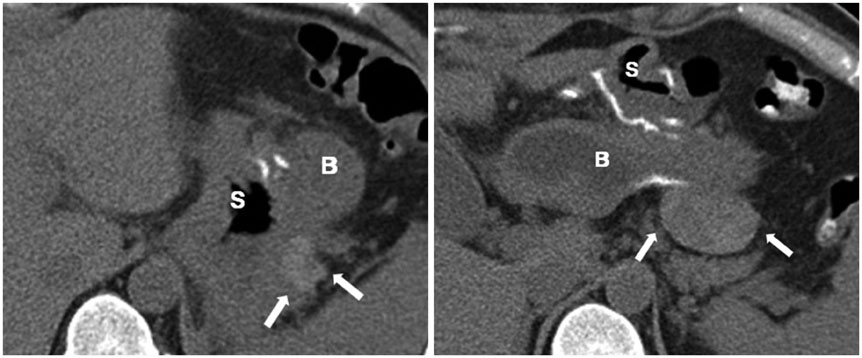
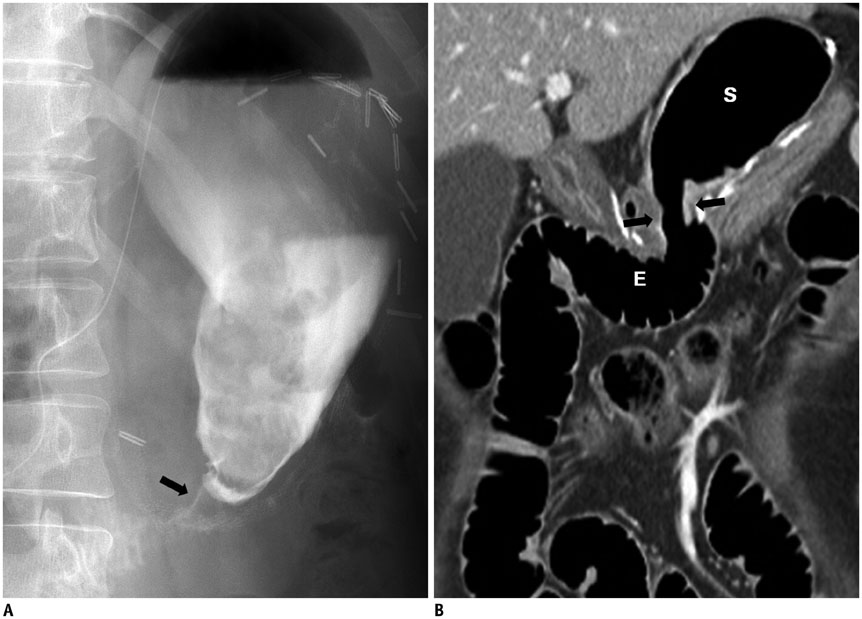
- Laparoscopic mini-gastric bypass surgery is a safe and simple surgical intervention for treating morbid obesity and diabetes mellitus and is now being performed more frequently. Radiologists must be critical in their postoperative evaluation of these patients. In this pictorial review, we explain and illustrate the surgical technique, normal postoperative anatomy, and associated complications as seen on imaging examinations, including fluoroscopy and computed tomography.
MeSH Terms
Figure
Reference
-
1. NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991; 115:956–961.2. Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995; 222:339–350. discussion 350-352.3. O'Brien PE, Dixon JB, Laurie C, Skinner S, Proietto J, McNeil J, et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med. 2006; 144:625–633.4. Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007; 357:753–761.5. Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, Hamad G, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003; 238:467–484. discussion 484-485.6. Lee WJ, Wang W, Lee YC, Huang MT, Ser KH, Chen JC. Effect of laparoscopic mini-gastric bypass for type 2 diabetes mellitus: comparison of BMI>35 and <35 kg/m2. J Gastrointest Surg. 2008; 12:945–952.7. Brethauer SA, Aminian A, Romero-Talamás H, Batayyah E, Mackey J, Kennedy L, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013; 258:628–636. discussion 636-637.8. Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, et al. Bariatric surgery versus intensive medical therapy for diabetes--3-year outcomes. N Engl J Med. 2014; 370:2002–2013.9. Lee WJ, Yu PJ, Wang W, Chen TC, Wei PL, Huang MT. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005; 242:20–28.10. Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SC, Chen JC. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012; 22:1827–1834.11. Musella M, Susa A, Greco F, De Luca M, Manno E, Di Stefano C, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014; 28:156–163.12. Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005; 15:1304–1308.13. Greenfield LJ. Complications of gastric surgery. In : Greenfield LJ, editor. Complications in surgery and trauma. Philadelphia: Lippincott;1990. p. 457–467.14. Yu J, Turner MA, Cho SR, Fulcher AS, DeMaria EJ, Kellum JM, et al. Normal anatomy and complications after gastric bypass surgery: helical CT findings. Radiology. 2004; 231:753–760.15. Byrne TK. Complications of surgery for obesity. Surg Clin North Am. 2001; 81:1181–1193. vii-viii.16. Akkary E, Duffy A, Bell R. Deciphering the sleeve: technique, indications, efficacy, and safety of sleeve gastrectomy. Obes Surg. 2008; 18:1323–1329.17. Koehler RE, Halverson JD. Radiographic abnormalities after gastric bypass. AJR Am J Roentgenol. 1982; 138:267–270.18. Blachar A, Federle MP. Gastrointestinal complications of laparoscopic roux-en-Y gastric bypass surgery in patients who are morbidly obese: findings on radiography and CT. AJR Am J Roentgenol. 2002; 179:1437–1442.19. Podnos YD, Jimenez JC, Wilson SE, Stevens CM, Nguyen NT. Complications after laparoscopic gastric bypass: a review of 3464 cases. Arch Surg. 2003; 138:957–961.20. Carbajo M, García-Caballero M, Toledano M, Osorio D, García-Lanza C, Carmona JA. One-anastomosis gastric bypass by laparoscopy: results of the first 209 patients. Obes Surg. 2005; 15:398–404.21. Noun R, Skaff J, Riachi E, Daher R, Antoun NA, Nasr M. One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg. 2012; 22:697–703.22. Csendes A, Burdiles P, Burgos AM, Maluenda F, Diaz JC. Conservative management of anastomotic leaks after 557 open gastric bypasses. Obes Surg. 2005; 15:1252–1256.23. Jordan JH, Hocking MP, Rout WR, Woodward ER. Marginal ulcer following gastric bypass for morbid obesity. Am Surg. 1991; 57:286–288.24. Rasmussen JJ, Fuller W, Ali MR. Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc. 2007; 21:1090–1094.25. Wang W, Wei PL, Lee YC, Huang MT, Chiu CC, Lee WJ. Short-term results of laparoscopic mini-gastric bypass. Obes Surg. 2005; 15:648–654.26. Papavramidis S, Deligianidis N, Papavramidis T, Sapalidis K, Katsamakas M, Gamvros O. Laparoscopic cholecystectomy after bariatric surgery. Surg Endosc. 2003; 17:1061–1064.27. Fidler J, Paulson EK, Layfield L. CT evaluation of acute cholecystitis: findings and usefulness in diagnosis. AJR Am J Roentgenol. 1996; 166:1085–1088.28. Macgregor AM, Pickens NE, Thoburn EK. Perforated peptic ulcer following gastric bypass for obesity. Am Surg. 1999; 65:222–225.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Morbid Obesity
- Metabolic Surgery and Diabetes Mellitus: Its Effects and Side Effects
- Mechanism of Metabolic Improvement After Bariatric Surgery
- Effects of Bariatric Surgery in Type 2 Diabetes Mellitus
- A Gut Feeling to Cure Diabetes: Potential Mechanisms of Diabetes Remission after Bariatric Surgery