Yonsei Med J.
2015 Mar;56(2):503-509. 10.3349/ymj.2015.56.2.503.
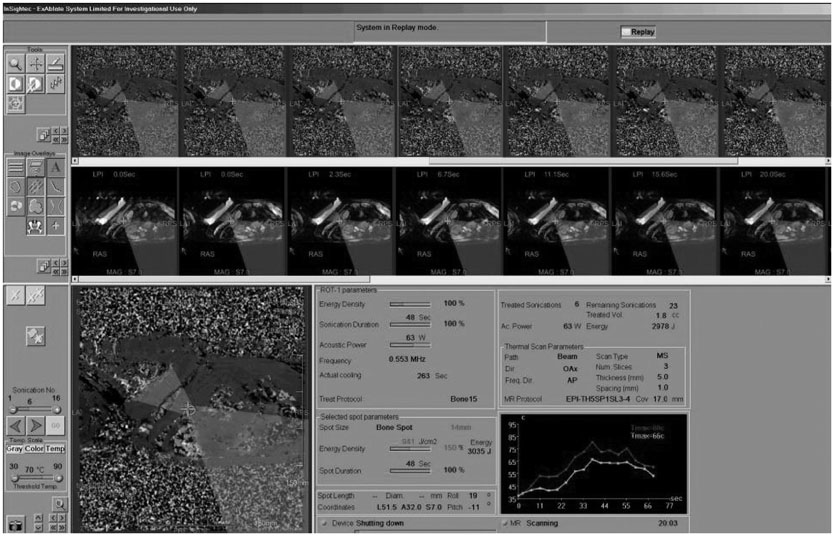
Pain Palliation in Patients with Bone Metastases Using Magnetic Resonance-Guided Focused Ultrasound with Conformal Bone System: A Preliminary Report
- Affiliations
-
- 1Department of Diagnostic Radiology, Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. radpms@yuhs.ac
- 2Pfizer Oncology, Seoul, Korea.
- 3Institute of Oncology, Yonsei University College of Medicine, Seoul, Korea.
- 4InSightec, Haifa, Israel.
- KMID: 2070031
- DOI: http://doi.org/10.3349/ymj.2015.56.2.503
Abstract
- PURPOSE
We evaluated the safety and effectiveness of the Magnetic Resonance-guided Focused Ultrasound (MRgFUS) with the ExAblate Conformal Bone System for the palliation of painful bone metastases.
MATERIALS AND METHODS
Our Institutional Review Board approved this study, and all patients gave informed consent prior to enrollment. A total of six painful metastatic bone lesions in five patients were treated using MRgFUS with the ExAblate Conformal Bone System for pain palliation. The follow-up sessions were at 3 days, 2 weeks, 1, 2, and 3 months, and 1 year after treatment. Efficacy was evaluated by the changes in visual analog scale (VAS) scores. At 3-months and 1-year follow-ups, unenhanced computed tomography and contrast-enhanced MR imaging examinations were performed. All adverse events were assessed to evaluate treatment safety.
RESULTS
All patients showed significant pain relief within 2 weeks. Two patients experienced complete pain reduction that lasted for 1 year. Two other patients showed pain relief measured as VAS scores of 2 and 4 on their last follow-up. Although the remaining patient had experienced significant pain relief in two lesions, the VAS score re-increased on his last follow-up. The size of the enhancing soft tissue mass in metastatic lesions decreased, and new bone formation was seen on follow-up images. Although adverse events were not serious, non-specific leg pain and second degree skin burn were noted.
CONCLUSION
MRgFUS was demonstrated to be effective palliative treatment within 2 weeks in selected patients with painful bone metastases.
Keyword
MeSH Terms
-
Adult
Aged
Bone Neoplasms/secondary/*therapy
Contrast Media
Female
High-Intensity Focused Ultrasound Ablation/adverse effects/*methods
Humans
Magnetic Resonance Imaging, Interventional/*methods
Magnetic Resonance Spectroscopy
Male
Middle Aged
Pain
*Pain Management
*Palliative Care
Prospective Studies
Tomography, X-Ray Computed
Treatment Outcome
Young Adult
Contrast Media
Figure
Reference
-
1. Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 2004; 350:1655–1664.2. Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. 1997; 69:1–18.3. Rades D, Schild SE, Abrahm JL. Treatment of painful bone metastases. Nat Rev Clin Oncol. 2010; 7:220–229.
Article4. Sze WM, Shelley MD, Held I, Wilt TJ, Mason MD. Palliation of metastatic bone pain: single fraction versus multifraction radiotherapy--a systematic review of randomised trials. Clin Oncol (R Coll Radiol). 2003; 15:345–352.
Article5. Callstrom MR, Charboneau JW, Goetz MP, Rubin J, Atwell TD, Farrell MA, et al. Image-guided ablation of painful metastatic bone tumors: a new and effective approach to a difficult problem. Skeletal Radiol. 2006; 35:1–15.
Article6. Cole DJ. A randomized trial of a single treatment versus conventional fractionation in the palliative radiotherapy of painful bone metastases. Clin Oncol (R Coll Radiol). 1989; 1:59–62.
Article7. 8 Gy single fraction radiotherapy for the treatment of metastatic skeletal pain: randomised comparison with a multifraction schedule over 12 months of patient follow-up. Bone Pain Trial Working Party. Radiother Oncol. 1999; 52:111–121.8. Gianfelice D, Gupta C, Kucharczyk W, Bret P, Havill D, Clemons M. Palliative treatment of painful bone metastases with MR imaging--guided focused ultrasound. Radiology. 2008; 249:355–363.
Article9. Saarto T, Janes R, Tenhunen M, Kouri M. Palliative radiotherapy in the treatment of skeletal metastases. Eur J Pain. 2002; 6:323–330.
Article10. Goetz MP, Callstrom MR, Charboneau JW, Farrell MA, Maus TP, Welch TJ, et al. Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: a multicenter study. J Clin Oncol. 2004; 22:300–306.
Article11. Liberman B, Gianfelice D, Inbar Y, Beck A, Rabin T, Shabshin N, et al. Pain palliation in patients with bone metastases using MR-guided focused ultrasound surgery: a multicenter study. Ann Surg Oncol. 2009; 16:140–146.
Article12. Napoli A, Anzidei M, Marincola BC, Brachetti G, Ciolina F, Cartocci G, et al. Primary pain palliation and local tumor control in bone metastases treated with magnetic resonance-guided focused ultrasound. Invest Radiol. 2013; 48:351–358.
Article13. Ishihara Y, Calderon A, Watanabe H, Okamoto K, Suzuki Y, Kuroda K, et al. A precise and fast temperature mapping using water proton chemical shift. Magn Reson Med. 1995; 34:814–823.
Article14. Chung AH, Jolesz FA, Hynynen K. Thermal dosimetry of a focused ultrasound beam in vivo by magnetic resonance imaging. Med Phys. 1999; 26:2017–2026.
Article15. McDannold N, King RL, Jolesz FA, Hynynen K. The use of quantitative temperature images to predict the optimal power for focused ultrasound surgery: in vivo verification in rabbit muscle and brain. Med Phys. 2002; 29:356–365.
Article16. Hindley J, Gedroyc WM, Regan L, Stewart E, Tempany C, Hynyen K, et al. MRI guidance of focused ultrasound therapy of uterine fibroids: early results. AJR Am J Roentgenol. 2004; 183:1713–1719.
Article17. Leon-Villapalos J, Kaniorou-Larai M, Dziewulski P. Full thickness abdominal burn following magnetic resonance guided focused ultrasound therapy. Burns. 2005; 31:1054–1055.
Article18. Stewart EA, Gedroyc WM, Tempany CM, Quade BJ, Inbar Y, Ehrenstein T, et al. Focused ultrasound treatment of uterine fibroid tumors: safety and feasibility of a noninvasive thermoablative technique. Am J Obstet Gynecol. 2003; 189:48–54.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Use of Magnetic Resonance-Guided Focused Ultrasound Surgery for Long-Term Pain Palliation in a Patient Suffering from Metastatic Bone Tumor
- Pregnancy and Natural Delivery Following Magnetic Resonance Imaging-Guided Focused Ultrasound Surgery of Uterine Myomas
- Magnetic Resonance-Guided Focused Ultrasound in Neurosurgery: Taking Lessons from the Past to Inform the Future
- Magnetic Resonance Guided Focused Ultrasound Induced Dermal Burn, Case Report
- Characteristics of Focused Ultrasound Mediated Blood-Brain Barrier Opening in Magnetic Resonance Images