Korean J Urol.
2014 Sep;55(9):620-623. 10.4111/kju.2014.55.9.620.
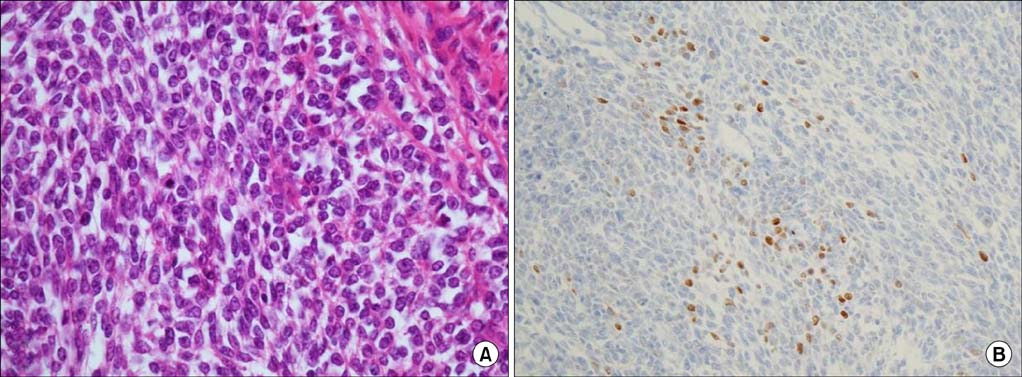
Two Different Surgical Approaches for Prostatic Stromal Sarcoma: Robot-Assisted Laparoscopic Radical Prostatectomy and Open Radical Cysto-Prostatectomy With Ileal Conduit
- Affiliations
-
- 1Department of Urology, Kyungpook National University School of Medicine, Daegu, Korea. tgkwon@knu.ac.kr
- 2Department of Pathology, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 2069781
- DOI: http://doi.org/10.4111/kju.2014.55.9.620
Abstract
- Stromal sarcoma of the prostate is very rare and shows rapid growth, which consequently is related to poor prognosis. Recently, we treated two cases of prostatic stromal sarcoma: one with robot-assisted laparoscopic radical prostatectomy and the other with open radical cysto-prostatectomy with an ileal conduit. To the best of our knowledge, this is the first case report of a prostatic stromal sarcoma managed by use of a robotic procedure. Here, we report of our experiences in the treatment of prostatic stromal sarcoma by use of two different methods.
Keyword
MeSH Terms
-
Adult
Humans
Laparoscopy/*methods
Magnetic Resonance Imaging
Male
Middle Aged
Prostate/surgery
Prostatectomy/*methods
Prostatic Neoplasms/diagnosis/*surgery
Rectum/surgery
*Robotics
Sarcoma/diagnosis/*surgery
Seminal Vesicles/surgery
Tomography, X-Ray Computed
Treatment Outcome
Urinary Bladder/surgery
Urinary Diversion/*methods
Figure
Reference
-
1. Chang YS, Chuang CK, Ng KF, Liao SK. Prostatic stromal sarcoma in a young adult: a case report. Arch Androl. 2005; 51:419–424.2. Gaudin PB, Rosai J, Epstein JI. Sarcomas and related proliferative lesions of specialized prostatic stroma: a clinicopathologic study of 22 cases. Am J Surg Pathol. 1998; 22:148–162.3. Sexton WJ, Lance RE, Reyes AO, Pisters PW, Tu SM, Pisters LL. Adult prostate sarcoma: the M. D. Anderson Cancer Center Experience. J Urol. 2001; 166:521–525.4. Tamada T, Sone T, Miyaji Y, Kozuka Y, Ito K. MRI appearance of prostatic stromal sarcoma in a young adult. Korean J Radiol. 2011; 12:519–523.5. Herawi M, Epstein JI. Specialized stromal tumors of the prostate: a clinicopathologic study of 50 cases. Am J Surg Pathol. 2006; 30:694–704.6. Hossain D, Meiers I, Qian J, MacLennan GT, Bostwick DG. Prostatic stromal hyperplasia with atypia: follow-up study of 18 cases. Arch Pathol Lab Med. 2008; 132:1729–1733.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robot-Assisted Laparoscopic Radical Prostatectomy
- Erratum: Robot-Assisted Laparoscopic Radical Prostatectomy
- Radical Prostatectomy
- A Case of Robot-Assisted Laparoscopic Radical Prostatectomy in Primary Small Cell Prostate Cancer
- Changes in Patterns of Radical Prostatectomy due to Diffusion of Robotic Surgical System: A Nationwide Study Using Health Insurance Claims Data