Infect Chemother.
2015 Sep;47(3):183-189. 10.3947/ic.2015.47.3.183.
A Case of Recurrent Meningitis Caused by Rhodococcus species Successfully Treated with Antibiotic Treatment and Intrathecal Injection of Vancomycin through an Ommaya Reservoir
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. paihj@hanyang.ac.kr
- KMID: 2068984
- DOI: http://doi.org/10.3947/ic.2015.47.3.183
Abstract
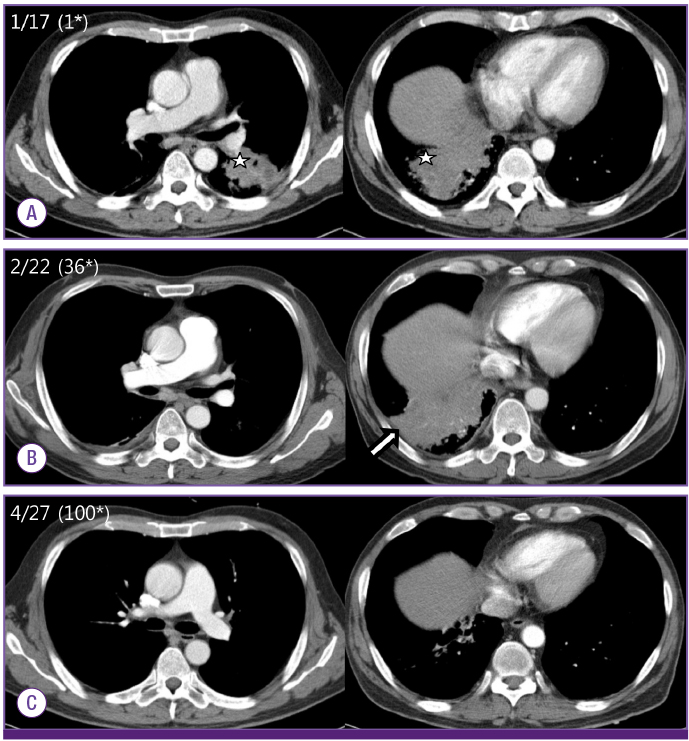
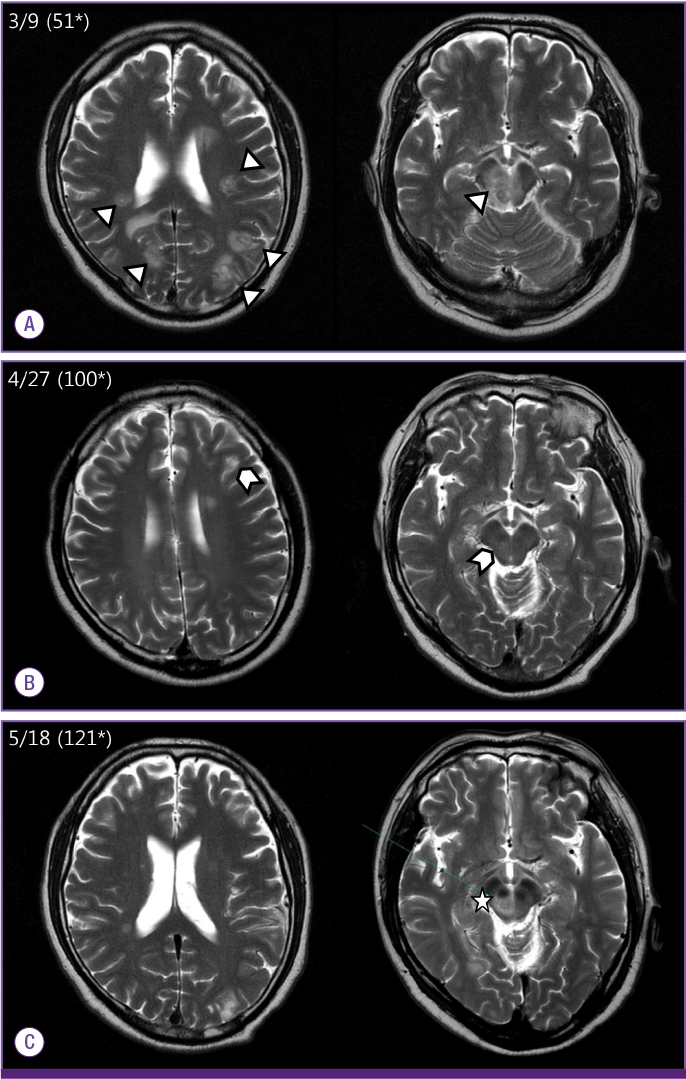
- Human infection by Rhodococcus species is rare and mostly limited to immunocompromised hosts such as patients infected with the human immunodeficiency virus (HIV) or organ transplant recipients. The most common strain is R. equi, and the most common clinical presentation is pulmonary infection, reported in 80% of Rhodococcus spp. infections. The central nervous system is an uncommon infection site. We report a case of a patient with pneumonia, brain abscess, and recurrent meningitis caused by Rhodococcus spp. He initially presented with pneumonia with necrosis, which progressed to brain abscess and recurrent meningitis. Rhodococcus spp. was identified from the cerobrospinal fluid (CSF) collected during his fourth hospital admission. Despite prolonged treatment with appropriate antibiotics, meningitis recurred three times. Finally, in order to administer antibiotics directly into the CSF and bypass the blood-brain barrier, an Ommaya reservoir was inserted for administration of 90 days of intrathecal vancomycin and amikacin in conjunction with intravenous and oral antibiotics; the patient was finally cured with this treatment regimen.
MeSH Terms
Figure
Cited by 1 articles
-
Pneumococcal Meningitis Successfully Treated with Adjuvant Management of Intrathecal Vancomycin, Oral Rifampicin and Shunt Surgery
Byeongsoo Yim, Seung-Hun Oh, Jinkwon Kim
J Neurocrit Care. 2016;9(2):166-170. doi: 10.18700/jnc.160069.
Reference
-
1. Weinstock DM, Brown AE. Rhodococcus equi: an emerging pathogen. Clin Infect Dis. 2002; 34:1379–1385.2. Golub B, Falk G, Spink WW. Lung abscess due to Corynebacterium equi: report of first human infection. Ann Intern Med. 1967; 66:1174–1177.3. Lasky JA, Pulkingham N, Powers MA, Durack DT. Rhodococcus equi causing human infections: review of 29 cases. South Med J. 1991; 84:1217–1220.4. Verville TD, Huycke MM, Greenfield RA, Fine DP, Kuhls TL, Slater LN. Rhodococcus equi infections of humans 12 cases and a review of the literature. Medicine (Baltimore). 1994; 73:119–132.5. Weingarten JS, Huang DY, Jackman JD Jr. Rhodococcus equi pneumonia: an unusual early manifestation of the acquired immunodeficiency syndrome (AIDS). Chest. 1988; 94:195–196.6. Kedlaya I, Ing MB, Wong SS. Rhodococcus equi infections in immunocompetent hosts: case report and review. Clin Infect Dis. 2001; 32:E39–E46.7. Harvey RL, Sunstrum JC. Rhodococcus equi infection in patients with and without human immunodeficiency virus infection. Rev Infect Dis. 1991; 13:139–145.
Article8. McNeil MM, Brown JM. Distribution and antimicrobial susceptibility of Rhodococcus equi from clinical specimens. Eur J Epidemiol. 1992; 8:437–443.
Article9. Rouquet RM, Clove D, Massip P, Moatti N, Leophonte P. Imipenem/vancomycin for Rhodococcus equi pulmonary infection in an HIV-positive patient. Lancet. 1991; 337:375.
Article10. Nordmann P, Ronco E. In-vitro antimicrobial susceptibility of Rhodococcus equi. J Antimicrob Chemother. 1992; 29:383–393.11. Bowersock TL, Salmon SA, Portis ES, Prescott JF, Robison DA, Ford CW, Watts JL. MICs of oxazolidinones for Rhodococcus equi strains isolated from humans and animals. Antimicrob Agents Chemother. 2000; 44:1367–1369.
Article12. Samies JH, Hathaway BN, Echols RM, Veazey JM Jr, Pilon VA. Lung abscess due to Corynebacterium equi. Report of the first case in a patient with acquired immune deficiency syndrome. Am J Med. 1986; 80:685–688.
Article13. Nordmann P, Chavanet P, Caillon J, Duez JM, Portier H. Recurrent pneumonia due to rifampicin-resistant Rhodococcus equi in a patient infected with HIV. J Infect. 1992; 24:104–107.
Article14. Van Etta LL, Filice GA, Ferguson RM, Gerding DN. Corynebacterium equi: a review of 12 cases of human infection. Rev Infect Dis. 1983; 5:1012–1018.15. Drancourt M, Bonnet E, Gallais H, Peloux Y, Raoult D. Rhodococcus equi infection in patients with AIDS. J Infect. 1992; 24:123–131.16. Nau R, Sörgel F, Eiffert H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin Microbiol Rev. 2010; 23:858–883.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapeutic Trials in Two Cases with Chronic Meningitisvia Ommaya Reservoir
- Traumatic Subdural Hygroma Due to Injury of an Ommaya Reservoir: A Case Report
- Treatment of Meningitis Caused by Vancomycin-Resistant Enterococcus with Synercid
- Vancomycin-Resistant Enterococcus faecium Meningitis Treated with Linezolid: A Case Report and Review of the Literature
- Two Cases of Meningitis Caused by Penicillin-and Cephalosporin-resistant Streptococcus pneumoniae