J Korean Soc Spine Surg.
2015 Sep;22(3):114-117. 10.4184/jkss.2015.22.3.114.
Nodular Fasciitis as a Pseudosarcomatous Lesion in the Ligamentum Nuchae: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. jheaj@paik.ac.kr
- 2Department of Pathology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2068930
- DOI: http://doi.org/10.4184/jkss.2015.22.3.114
Abstract
- STUDY DESIGN: A case report.
OBJECTIVES
Nodular fasciitis is a non-neoplastic soft-tissue lesion located in the deep subcutaneous region; it may be misdiagnosed as a malignant tumor due to its rapid growth and microscopic characteristics. We introduce an unusual case of nodular fasciitis which presented as a posterior neck mass. SUMMARY OF LITERATURE REVIEW: Nodular fasciitis is an unusual benign lesion.Becaue it sometimes shows aggressive microscopic characteristics, (being hypercellular and polymorphic), the condition has the potential to be misdiagnosed as sarcoma.
MATERIALS AND METHODS
A 20-year-old woman presented with a 1-month history of a progressively enlarging mass on her posterior neck. Computed tomography (CT) scans of the neck showed a markedly enhanced, well-defined, ovoid soft tissue mass at the posterior of the spinous process of C2. The patient underwent marginal excision. There was a 2 cm, well-capsulated, pinkish-gray mass.
RESULTS
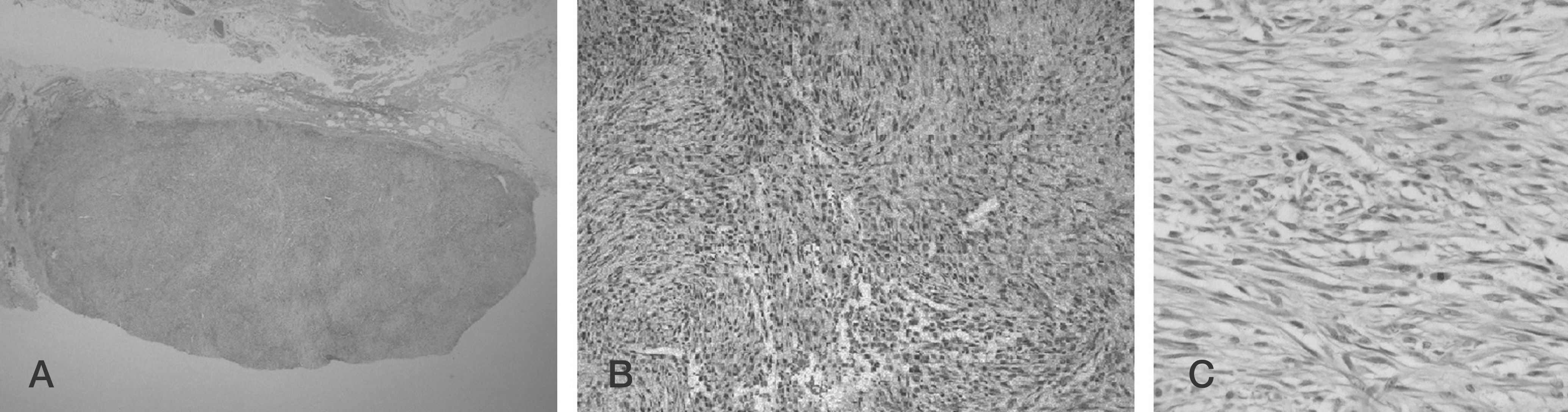
She recovered without any complications. Histopathologic examination showed a spindle cell proliferation, increased cellularity, and nuclear atypia with mitosis. The immunohistochemistry stain showed negative findings. The mass was diagnosed as nodular fasciitis.
CONCLUSIONS
A diagnosis of nodular fasciitis, not just malignant tumor, should be considered for a rapidly growing posterior neck mass showing aggressive microscopic appearance, Nodular fasciitis is a self-limiting lesion readily treated by marginal excision. However, follow-ups should be increased to watch for recurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Shin J, Lee H, Cho K-J, et al. Nodular fasciitis of the head and neck: radiographic findings. Clin Imaging. 2003; 27:31–7.2. Harrison HC, Motbey J, Kan AE, de Silva M. Nodular fasciitis of the nose in a child. Int J Pediatr Otorhinolaryngol. 1995; 33:257–64.
Article3. Powers CN, Berardo MD, Frable WJ. Fine-needle aspiration biopsy: pitfalls in the diagnosis of spindle-cell lesions. Diagn Cytopathol. 1994; 10:232–40.
Article4. Montgomery EA, Meis JM. Nodular fasciitis. Its morpho-logic spectrum and immunohistochemical profile. Am J Surg Pathol. 1991; 15:942–8.5. Chung EB, Enzinger FM. Proliferative fasciitis. Cancer. 1975; 36:1450–8.
Article6. Plaza J, Mayerson J, Wakely P. Nodular fasciitis of the hand: a potential diagnostic pitfall in fine-needle aspiration cytopathology. Am J Clin Pathol. 2005; 123:388–93.7. Koenigsberg RA, Faro S, Chen X, Marlowe F. Nodular fasciitis as a vascular neck mass. AJNR, Am J Neuroradiol. 1996; 17:567–9.8. Oshiro Y, Fukuda T, Tsuneyoshi M. Fibrosarcoma versus fibromatoses and cellular nodular fasciitis. A comparative study of their proliferative activity using proliferating cell nuclear antigen, DNA flow cytometry, and p53. Am J Surg Pathol. 1994; 18:712–9.9. Kim S, Kim H-J, Park S-W, et al. Nodular fasciitis in the head and neck: CT and MR imaging findings. AJNR, Am J Neuroradiol. 2005; 26:2617–23.10. Dahl I, Jarlstedt J. Nodular fasciitis in the head and neck. A clinicopathological study of 18 cases. Act otolaryngol. 1980; 90:152–9.
Article11. Batsakis JG, el Naggar AK. Pseudosarcomatous proliferative lesions of soft tissues. The Annals of otology, rhinology & laryngology. Ann Otol Rhinol Laryngol. 1994; 103:578–82.12. DiNardo LJ, Wetmore RF, Potsic WP. Nodular fasciitis of the head and neck in children. A deceptive lesion. Arch Otolaryngol Head Neck Surg. 1991; 117:1001–2.
Article13. Wong N, Di F. Pseudosarcomatous fasciitis and myositis: diagnosis by fine-needle aspiration cytology. Am J Clin Pathol. 2009; 132:857–65.14. Jo V, Fletcher CDM. WHO classification of soft tissue tu-mours: an update based on the 2013 (4th) edition. Pathology. 2014; 46:95–104.
Article