J Korean Soc Surg Hand.
2015 Sep;20(3):119-126. 10.12790/jkssh.2015.20.3.119.
Diagnosis and Treatment for Deep Nontuberculous Mycobacteria Infection of the Hand and Wrist
- Affiliations
-
- 1Department of Orthopedic Surgery, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University, Uijeongbu, Korea.
- 2Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. micro@amc.seoul.kr
- KMID: 2068817
- DOI: http://doi.org/10.12790/jkssh.2015.20.3.119
Abstract
- PURPOSE
The purpose of this study was to present a systematic treatment method for nontuberculous mycobacteria (NTM) infection of the hand and wrist to gain better clinical outcomes.
METHODS
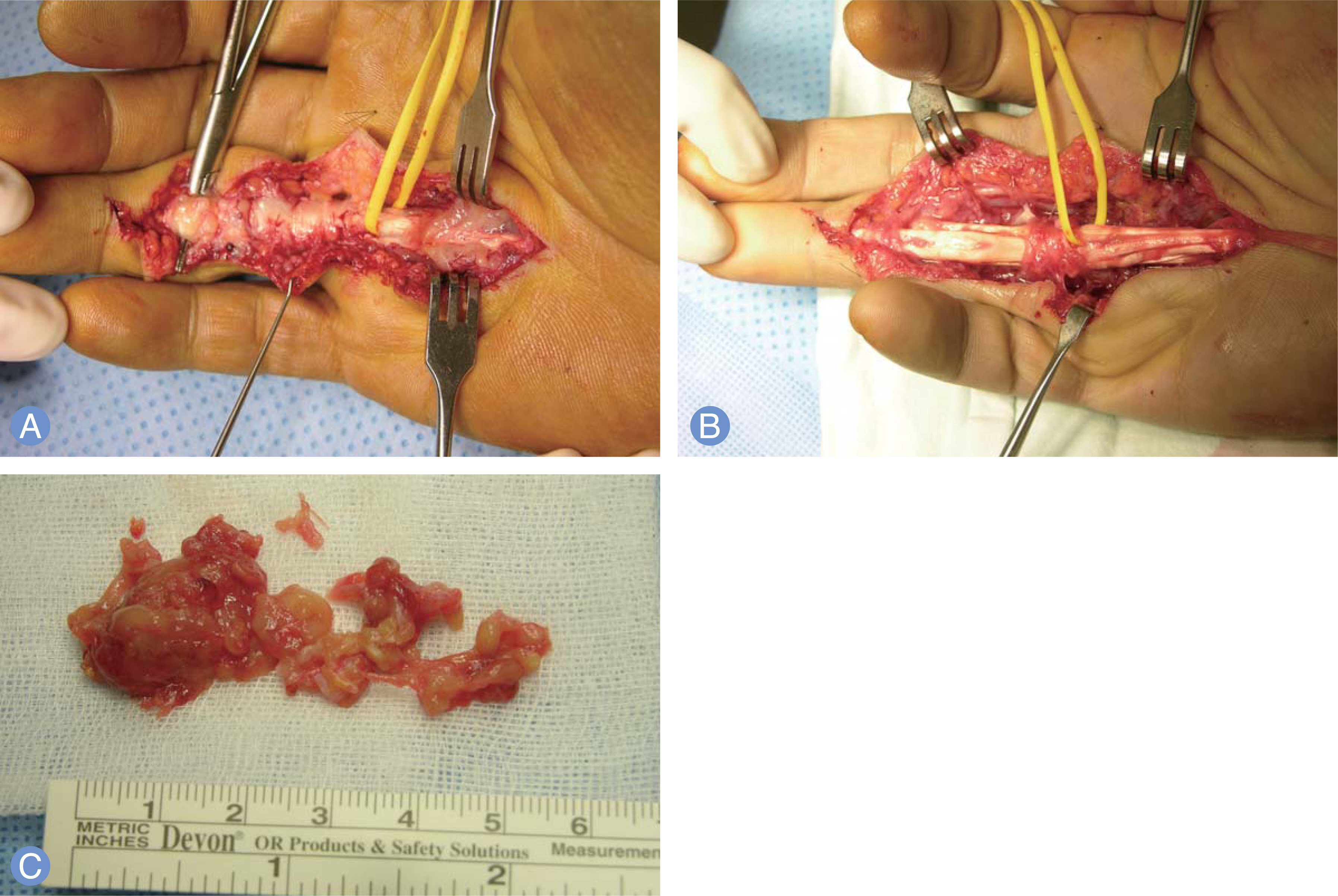
10 patients of deep NTM infection of the hand and wrist were reviewed. Extensive debridement was performed in all cases. When biopsy result suggested mycobacterial infection such as granulomatous inflammation, empirical tuberculosis medication was started. After culture confirmed NTM growth, the species was identified and in vitro sensitivity test was performed. Then medication was switched according to the results. Functional outcomes of the hand and wrist were measured by total active motion of the fingers and by range of motion of the wrist respectively.
RESULTS
Diagnosis was tenosynovitis in seven patients, infective arthritis and osteomyelitis combined with tenosynovitis of the wrist in three patients. Two patients had recurred skin ulcer during follow-up period and undergone second debridement. After second operation, no patient had a persistent discharging sinus and all patient were completely healed during follow-up period. Functional outcome of the eight patients who had NTM infection of their hand was excellent in two, good in four, fair in one, poor in one. Mean range of motion of the two patients who had osteomyelitis of their wrist was dorsiflexion 20degrees, volar flexion 15degrees, radial deviation 0degrees, ulnar deviation 15degrees.
CONCLUSION
Our standardized treatment protocol can be helpful for treatment of deep NTM infection of the hand and wrist.
MeSH Terms
Figure
Reference
-
References
1. Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.
Article2. von Reyn CF, Arbeit RD, Horsburgh CR, et al. Sources of disseminated Mycobacterium avium infection in AIDS. J Infect. 2002; 44:166–70.
Article3. Yoon HJ, Kwon JW, Yoon YC, Choi SH. Nontuberculous mycobacterial tenosynovitis in the hand: two case reports with the MR imaging findings. Korean J Radiol. 2011; 12:745–9.
Article4. Mazis GA, Sakellariou VI, Kontos F, Zerva L, Spyridonos SG. Recurrent fluctuant mass of the wrist and forearm associated with chronic tenosynovitis by Mycobacterium kansasii. Orthopedics. 2011; 34:400.
Article5. Lee WJ, Kang SM, Sung H, et al. Non-tuberculous mycobacterial infections of the skin: a retrospective study of 29 cases. J Dermatol. 2010; 37:965–72.
Article6. Woods GL. Clinical and Laboratory Standards Institute. Susceptibility testing of mycobacteria, nocardiae and other aerobic actinomycetes tmvpdltm tkrwp: approved standard. Wayne, PA: Clinical and Laboratory Standards Institute;2011.7. Strickland JW, Glogovac SV. Digital function following flexor tendon repair in Zone II: A comparison of immobilization and controlled passive motion techniques. J Hand Surg Am. 1980; 5:537–43.
Article8. Mazon A, Gil-Setas A, Alfaro J, Idigoras P. Diagnosis of tuberculous arthritis from the isolation of Mycobacterium tuberculosis in blood agar and chocolate agar. Enferm Infecc Microbiol Clin. 2000; 18:527–8.9. Wolinsky E. Nontuberculous mycobacteria and associated diseases. Am Rev Respir Dis. 1979; 119:107–59.10. Wallace RJ Jr, Swenson JM, Silcox VA, Good RC, Tschen JA, Stone MS. Spectrum of disease due to rapidly growing mycobacteria. Rev Infect Dis. 1983; 5:657–79.
Article11. Falkinham JO 3rd. Epidemiology of infection by nontuberculous mycobacteria. Clin Microbiol Rev. 1996; 9:177–215.
Article12. Wallace RJ Jr, Swenson JM, Silcox VA, Bullen MG. Treatment of nonpulmonary infections due to Mycobacterium fortuitum and Mycobacterium chelonei on the basis of in vitro susceptibilities. J Infect Dis. 1985; 152:500–14.
Article13. Wolinsky E, Gomez F, Zimpfer F. Sporotrichoid Mycobacterium marinum infection treated with rifampin-ethambutol. Am Rev Respir Dis. 1972; 105:964–7.14. Aubry A, Chosidow O, Caumes E, Robert J, Cambau E. Sixty-three cases of Mycobacterium marinum infection: clinical features, treatment, and antibiotic susceptibility of causative isolates. Arch Intern Med. 2002; 162:1746–52.15. Cheung JP, Fung B, Wong SS, Ip WY. Review article: Mycobacterium marinum infection of the hand and wrist. J Orthop Surg (Hong Kong). 2010; 18:98–103.
Article16. Chow SP, Stroebel AB, Lau JH, Collins RJ. Mycobacterium marinum infection of the hand involving deep structures. J Hand Surg Am. 1983; 8:568–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Nontuberculous Mycobacterium Manifestation 1 Year after a Dog Bite on the Hand
- Nontuberculous Mycobacterial Tenosynovitis in the Hand: Two Case Reports with the MR Imaging Findings
- Chronic Granulomatous Infection of Soft Tissue Complicated by Trauma of a Lower Leg
- Ultrasonographic Diagnosis of the Hand and Wrist Joint
- A Case of Tenosynovitis Due to Mycobacterium intracellulare in a Patient with Rheumatoid Arthritis