J Korean Med Assoc.
2010 Dec;53(12):1065-1073. 10.5124/jkma.2010.53.12.1065.
High field strength magnetic resonance imaging of abdominal diseases
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. serha@catholic.ac.kr
- KMID: 2064722
- DOI: http://doi.org/10.5124/jkma.2010.53.12.1065
Abstract
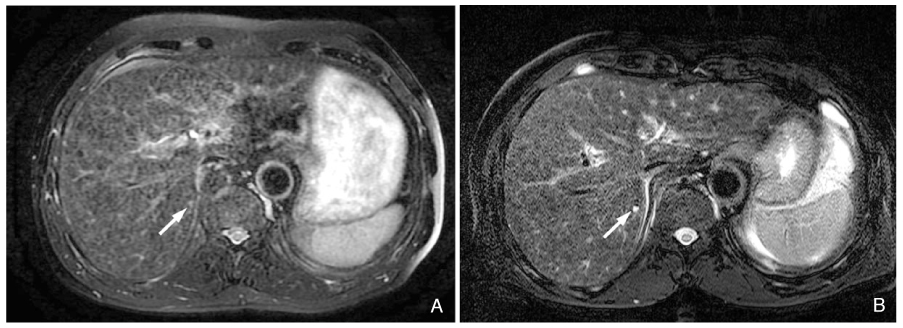
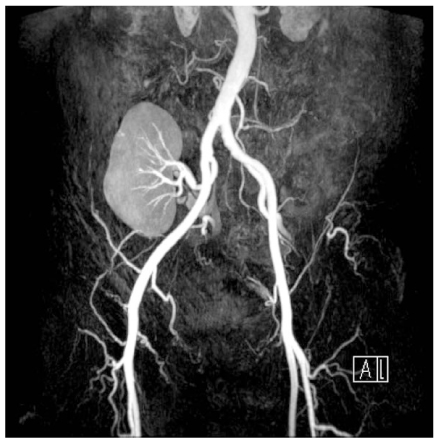
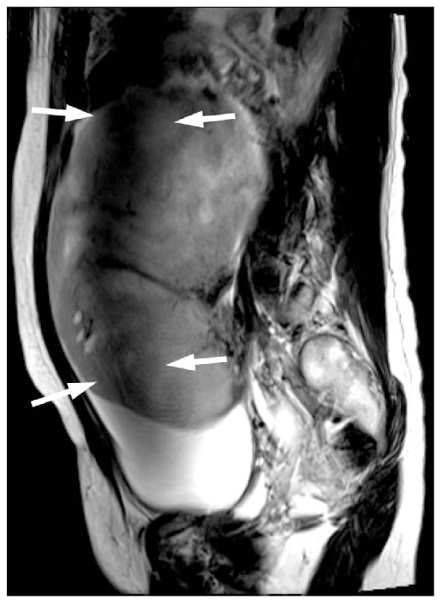
- Due to the development of dedicated receiver coils for 3 tesla (T) magnetic resonance (MR) imaging and increased gradient performance, 3T MR imaging of the abdomen is rapidly becoming a part of routine clinical practice. The most important advantage of 3T MR imaging is a higher signal-to-noise ratio and contrast-to-noise ratio compared with 1.5T systems, which can be used to improve spatial resolution and shorten image acquisition time. In the abdomen, the improved image quality of non-enhanced and enhanced solid organ imaging, MR angiography, MR cholangiopancreatography, and MR spectroscopy can be obtained at 3T due to the increased signal-to-noise ratio and contrast-to-noise ratio. However, 3T abdominal MR imaging also presents several technical challenges, such as increased energy deposition within the patient's body, standing wave artifacts, and increased susceptibility artifacts. Therefore, abdominal MR imaging at 3T requires adjustments in the sequence parameters of pulse sequences designed for 1.5T to optimize image quality. At present, 3T abdominal MR imaging is feasible with high image quality in an acceptable scan time, but 3T imaging is not significantly superior to 1.5T imaging in terms of cost-effectiveness. Future improvements in coil technology and new sequences suitable for 3T may enable wider clinical use of 3T for abdominal MR imaging.
MeSH Terms
Figure
Reference
-
1. Merkle EM, Dale BM, Paulson EK. Abdominal MR imaging at 3T. Magn Reson Imaging Clin N Am. 2006. 14:17–26.
Article2. Barth MM, Smith MP, Pedrosa I, Lenkinski RE, Rofsky NM. Body MR imaging at 3.0 T: understanding the opportunities and challenges. Radiographics. 2007. 27:1445–1462.
Article3. Chang KJ, Kamel IR, Macura KJ, Bluemke DA. 3.0-T MR imaging of the abdomen: comparison with 1.5 T. Radiographics. 2008. 28:1983–1998.
Article4. Merkle EM, Dale BM. Abdominal MRI at 3.0 T: the basics revisited. AJR Am J Roentgenol. 2006. 186:1524–1532.
Article5. Katz-Brull R, Rofsky NM, Lenkinski RE. Breathhold abdominal and thoracic proton MR spectroscopy at 3T. Magn Reson Med. 2003. 50:461–467.
Article6. Soher BJ, Dale BM, Merkle EM. A review of MR physics: 3T versus 1.5T. Magn Reson Imaging Clin N Am. 2007. 15:277–290.
Article7. Akisik FM, Sandrasegaran K, Aisen AM, Lin C, Lall C. Abdominal MR imaging at 3.0 T. Radiographics. 2007. 27:1433–1444.
Article8. Erturk SM, Alberich-Bayarri A, Herrmann KA, Marti-Bonmati L, Ros PR. Use of 3.0-T MR imaging for evaluation of the abdomen. Radiographics. 2009. 29:1547–1563.
Article9. Hussain SM, Wielopolski PA, Martin DR. Abdominal magnetic resonance imaging at 3.0 T: problem or a promise for the future? Top Magn Reson Imaging. 2005. 16:325–335.10. Martin DR, Friel HT, Danrad R, De Becker J, Hussain SM. Approach to abdominal imaging at 1.5 Tesla and optimization at 3 Tesla. Magn Reson Imaging Clin N Am. 2005. 13:241–254.
Article11. Krautmacher C, Willinek WA, Tschampa HJ, Born M, Träber F, Gieseke J, Textor HJ, Schild HH, Kuhl CK. Brain tumors: full- and half-dose contrast-enhanced MR imaging at 3.0 T compared with 1.5 T. Initial Experience. Radiology. 2005. 237:1014–1019.
Article12. Tsurusaki M, Semelka RC, Zapparoli M, Elias J Jr, Altun E, Pamuklar E, Sugimura K. Quantitative and qualitative comparison of 3.0T and 1.5T MR imaging of the liver in patients with diffuse parenchymal liver disease. Eur J Radiol. 2009. 72:314–320.
Article13. Ramalho M, Altun E, Herédia V, Zapparoli M, Semelka R. Liver MR imaging: 1.5T versus 3T. Magn Reson Imaging Clin N Am. 2007. 15:321–347.
Article14. Campeau NG, Huston J 3rd, Bernstein MA, Lin C, Gibbs GF. Magnetic resonance angiography at 3.0 Tesla: initial clinical experience. Top Magn Reson Imaging. 2001. 12:183–204.
Article15. Rohrer M, Bauer H, Mintorovitch J, Requardt M, Weinmann HJ. Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Invest Radiol. 2005. 40:715–724.
Article16. Michaely HJ, Nael K, Schoenberg SO, Finn JP, Laub G, Reiser MF, Ruehm SG. The feasibility of spatial high-resolution magnetic resonance angiography (MRA) of the renal arteries at 3.0 T. Rofo. 2005. 177:800–804.
Article17. Prince MR, Zhang HL, Prowda JC, Grossman ME, Silvers DN. Nephrogenic systemic fibrosis and its impact on abdominal imaging. Radiographics. 2009. 29:1565–1574.
Article18. Perez-Rodriguez J, Lai S, Ehst BD, Fine DM, Bluemke DA. Nephrogenic systemic fibrosis: incidence, associations, and effect of risk factor assessment: report of 33 cases. Radiology. 2009. 250:371–377.
Article19. Schindera ST, Miller CM, Ho LM, DeLong DM, Merkle EM. Magnetic resonance (MR) cholangiography: quantitative and qualitative comparison of 3.0 Tesla with 1.5 Tesla. Invest Radiol. 2007. 42:399–405.20. Isoda H, Kataoka M, Maetani Y, Kido A, Umeoka S, Tamai K, Koyama T, Nakamoto Y, Miki Y, Saga T, Togashi K. MRCP imaging at 3.0 T vs. 1.5 T: preliminary experience in healthy volunteers. J Magn Reson Imaging. 2007. 25:1000–1006.
Article21. Choi JY, Kim MJ, Chung YE, Kim JY, Jones AC, de Becker J, van Cauteren M. Abdominal applications of 3.0-T MR imaging: comparative review versus a 1.5-T system. Radiographics. 2008. 28:e30.
Article22. Koh DM, Collins DJ. Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol. 2007. 188:1622–1635.
Article23. Naganawa S, Kawai H, Fukatsu H, Sakurai Y, Aoki I, Miura S, Mimura T, Kanazawa H, Ishigaki T. Diffusion-weighted imaging of the liver: technical challenges and prospects for the future. Magn Reson Med Sci. 2005. 4:175–186.
Article24. Notohamiprodjo M, Dietrich O, Horger W, Horng A, Helck AD, Herrmann KA, Reiser MF, Glaser C. Diffusion tensor imaging (DTI) of the kidney at 3 tesla-feasibility, protocol evaluation and comparison to 1.5 Tesla. Invest Radiol. 2010. 45:245–254.
Article25. Jacobs MA, Ouwerkerk R, Petrowski K, Macura KJ. Diffusion-weighted imaging with apparent diffusion coefficient mapping and spectroscopy in prostate cancer. Top Magn Reson Imaging. 2008. 19:261–272.
Article26. Wang J, Yu T, Bai R, Sun H, Zhao X, Li Y. The value of the apparent diffusion coefficient in differentiating stage IA endometrial carcinoma from normal endometrium and benign diseases of the endometrium: initial study at 3-T magnetic resonance scanner. J Comput Assist Tomogr. 2010. 34:332–337.
Article27. Namimoto T, Awai K, Nakaura T, Yanaga Y, Hirai T, Yamashita Y. Role of diffusion-weighted imaging in the diagnosis of gynecological diseases. Eur Radiol. 2009. 19:745–760.
Article28. Lin G, Ng KK, Chang CJ, Wang JJ, Ho KC, Yen TC, Wu TI, Wang CC, Chen YR, Huang YT, Ng SH, Jung SM, Chang TC, Lai CH. Myometrial invasion in endometrial cancer. Diagnostic accuracy of diffusion-weighted 3.0-T MR imaging: initial experience. Radiology. 2009. 250:784–792.
Article29. Kim SH, Lee JM, Hong SH, Kim GH, Lee JY, Han JK, Choi BI. Locally advanced rectal cancer: added value of diffusion-weighted MR imaging in the evaluation of tumor response to neoadjuvant chemo- and radiation therapy. Radiology. 2009. 253:116–125.
Article30. Goshima S, Kanematsu M, Kondo H, Yokoyama R, Kajita K, Tsuge Y, Watanabe H, Shiratori Y, Onozuka M, Moriyama N. Diffusion-weighted imaging of the liver: optimizing b value for the detection and characterization of benign and malignant hepatic lesions. J Magn Reson Imaging. 2008. 28:691–697.
Article31. Zech CJ, Herrmann KA, Dietrich O, Horger W, Reiser MF, Schoenberg SO. Black-blood diffusion-weighted EPI acquisition of the liver with parallel imaging: comparison with a standard T2-weighted sequence for detection of focal liver lesions. Invest Radiol. 2008. 43:261–266.
Article32. Shellock FG, Crues JV. MR procedures: biologic effects, safety, and patient care. Radiology. 2004. 232:635–652.
Article33. Shellock FG. Radiofrequency energy-induced heating during MR procedures: a review. J Magn Reson Imaging. 2000. 12:30–36.
Article34. Franklin KM, Dale BM, Merkle EM. Improvement in B1-inhomogeneity artifacts in the abdomen at 3T MR imaging using a radiofrequency cushion. J Magn Reson Imaging. 2008. 27:1443–1447.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- High field strength magnetic resonance imaging of cardiovascular diseases
- Introduction to high field strength magnetic resonance imaging
- Clinical application of high field strength magnetic resonance imaging
- High field strength magnetic resonance imaging of brain lesion
- Review of Recent Advancement of Ultra High Field Magnetic Resonance Imaging: from Anatomy to Tractography