Hanyang Med Rev.
2012 Feb;32(1):8-16. 10.7599/hmr.2012.32.1.8.
The Process of Developing a Clinical Presentation Curriculum
- Affiliations
-
- 1Department of Internal Medicine, Inje University College of Medicine, Busan, Korea.
- 2Department of Medical Education, Hanyang University College of Medicine, Seoul, Korea. hoonkp@hanyang.ac.kr
- KMID: 2053753
- DOI: http://doi.org/10.7599/hmr.2012.32.1.8
Abstract
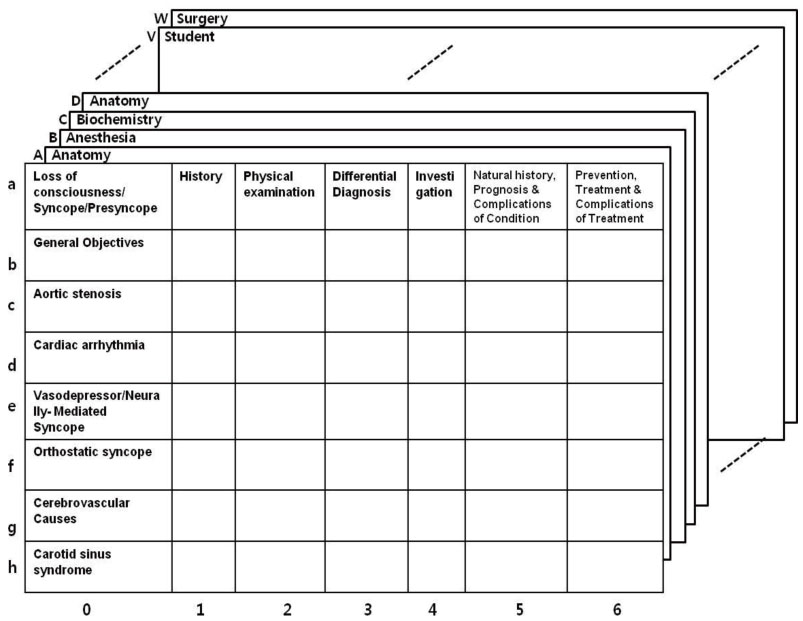
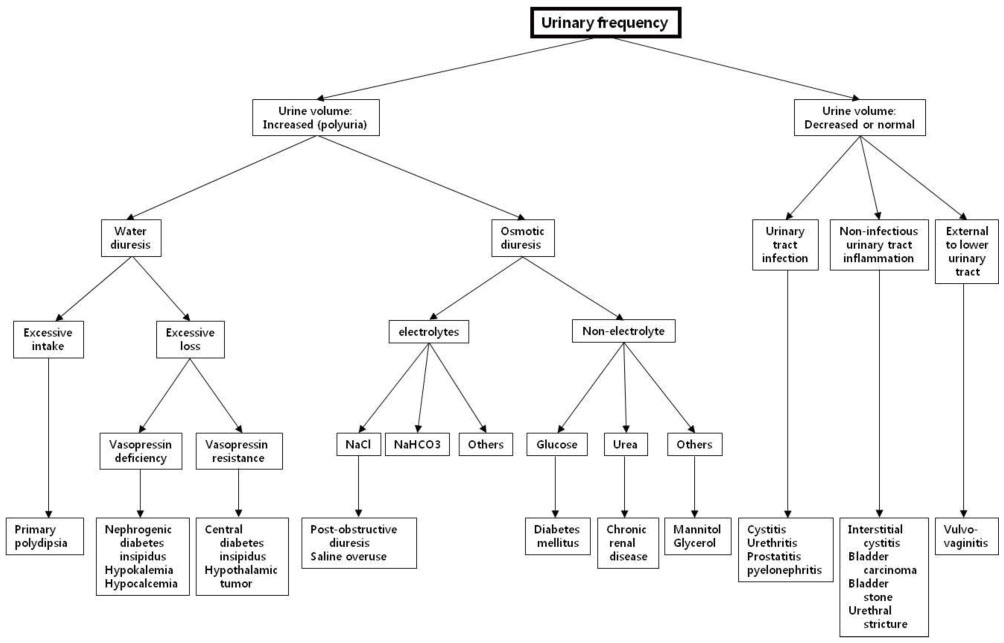
- In Korea, many medical schools have adapted their curricula to the recent paradigm shift introducing a professional graduate school system with universal accreditation criteria for medical education. This rapid transformation has driven the new adoption of system-based integrated curriculum, problem-based learning, team-based learning, and competency-based assessment. In the hundred years since the publication of Flexner's report that suggested a two-phase educational structure consisting of a basic science didactic curriculum followed by the practicum of clinical clerkships, there have been many advancements in curriculum development for medical education. Medical education is undergoing a major paradigm shift from structure- and process-based to competency-based education utilizing outcome-based assessments. The authors reviewed the existing medical literature to provide practical insight into the clinical presentation curriculum introduced by University of Calgary in 1994, developing a roadmap to accomplish full implementation and evaluation. In the clinical presentation based curriculum, schemata (schemes) are organized by experts from terminal objectives, and are considered to have two functions: first, to serve as frameworks around which students can learn new information and secondly, to provide an approach to clinical problem solving. We conclude that there should be further meticulous review of this new system and a prospective evaluation of the students' ability to benefit from it before launching a program based on the indiscreet adoption of a fashionable curricular reform.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Visualization of unstructured personal narratives of perterm birth using text network analysis
Jeung-Im Kim
Korean J Women Health Nurs. 2020;26(3):205-212. doi: 10.4069/kjwhn.2020.08.08.
Reference
-
1. Kim YI. Integrated curriculum: a pedagogical background in medical school. Korean J Med Educ. 1998. 10:1–10.
Article2. Kang PS. Integrated curriculum development in medical education. Korean J Med Educ. 1996. 8:83–87.
Article3. Shin JS, Lee YS. A study on the integrated medical teaching courses administration at Seoul national university college of medicine for the past thirty years. Korean J Med Educ. 2000. 12:271–287.
Article4. Chae SJ, Lee DS, Lee YS. Causal analysis and improvement strategies of the problems in implementing a PBL program in integrated curriculum. Korean J Med Educ. 2003. 15:35–43.
Article5. Oh SA, Chung EK, Rhee JA, Baik YH. An evaluation of integrated curriculum based on students' perspective. Korean J Med Educ. 2007. 19:305–311.
Article6. Park KH, Park CH, Chung WJ, Yoo CJ. Implementation of a problem-based learning program combined with team-based learning. Korean J Med Educ. 2010. 22:225–230.
Article7. Flexner A, Pritchett HS. Medical education in the United States and Canada: a report to the Carnegie foundation for the advancement of teaching. 1910. New York: Carnegie Foundation for the Advancement of Teaching;60–61.8. Dornan T, Mann KV, Scherpbier A, Spencer J. Medical education: theory and practice. 2010. Edinburgh: Churchill Livingstone;81–84.9. Woodward CA, Ferrier BM. The content of the medical curriculum at McMaster University: graduates' evaluation of their preparation for postgraduate training. Med Educ. 1983. 17:54–60.
Article10. Harden RM, Crosby JR, Davis MH, Friedman M. AMEE Guide No. 14: outcome-based education: par t 5-From competency to meta-competency: a model for the specification of learning outcomes. Med Teach. 1999. 21:546–552.
Article11. Harden RM. Developments in outcome-based education. Med Teach. 2002. 24:117–120.
Article12. Harden RM. Outcome-based education--the ostrich, the peacock and the beaver. Med Teach. 2007. 29:666–671.
Article13. Davis MH, Amin Z, Grande JP, O'Neill AE, Pawlina W, Viggiano TR, et al. Case studies in outcome-based education. Med Teach. 2007. 29:717–722.
Article14. Frank JR, Mungroo R, Ahmad Y, Wang M, De Rossi S, Horsley T. Toward a definition of competency-based education in medicine: a systematic review of published definitions. Med Teach. 2010. 32:631–637.
Article15. Carraccio C, Wolfsthal SD, Englander R, Ferentz K, Martin C. Shifting paradigms: from Flexner to competencies. Acad Med. 2002. 77:361–367.
Article16. Iobst WF, Sherbino J, Cate OT, Richardson DL, Dath D, Swing SR, et al. Competency-based medical education in postgraduate medical education. Med Teach. 2010. 32:651–656.
Article17. Harris P, Snell L, Talbot M, Harden RM. Competency-based medical education: implications for undergraduate programs. Med Teach. 2010. 32:646–650.
Article18. Mandin H, Harasym P, Eagle C, Watanabe M. Developing a "clinical presentation" curriculum at the University of Calgary. Acad Med. 1995. 70:186–193.
Article19. Mandin H, Dauphinee WD. Conceptual guidelines for developing and maintaining curriculum and examination objectives: the experience of the Medical Council of Canada. Acad Med. 2000. 75:1031–1037.
Article20. Woloschuk W, Harasym P, Mandin H, Jones A. Use of scheme-based problem solving: an evaluation of the implementation and utilization of schemes in a clinical presentation curriculum. Med Educ. 2000. 34:437–442.
Article21. Norman GR, Trott AD, Brooks LR, Smith EKM. Cognitive differences in clinical reasoning related to postgraduate training. Teach Learn Med. 1994. 6:114–120.
Article22. Woloschuk W, Mandin H, Harasym P, Lorscheider F, Brant R. Retention of basic science knowledge: a comparison between body system-based and clinical presentation curricula. Teach Learn Med. 2004. 16:116–122.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proper Level of Knowledge on Anatomy for Learning Embryology: Based in the Survey Analysis on the Newly Introduced Teaching Method (Group Presentation of Anatomy) to the Embryology Class
- Development and Evaluation of the 'Doctor and Leadership' Curriculum
- Developing a conceptual framework for a nursing curriculum
- Outcomes-based Curriculum Development and Student Evaluation in Nursing Education
- Implementation of Outcome-Based Medical Education Theory into the Pre-existing Curriculum