Electrolyte Blood Press.
2015 Jun;13(1):30-36. 10.5049/EBP.2015.13.1.30.
A Case of Osmotic Demyelination Presenting with Severe Hypernatremia
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Incheon Christian Hospital, Incheon, Korea.
- 3Department of Internal Medicine, National Rehabilitation Center, Seoul, Korea. mk2066@hanmail.net
- KMID: 2052340
- DOI: http://doi.org/10.5049/EBP.2015.13.1.30
Abstract
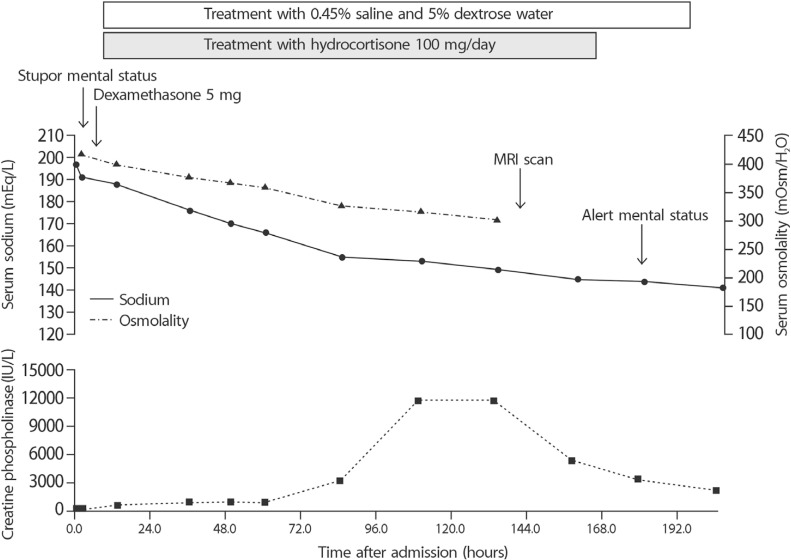
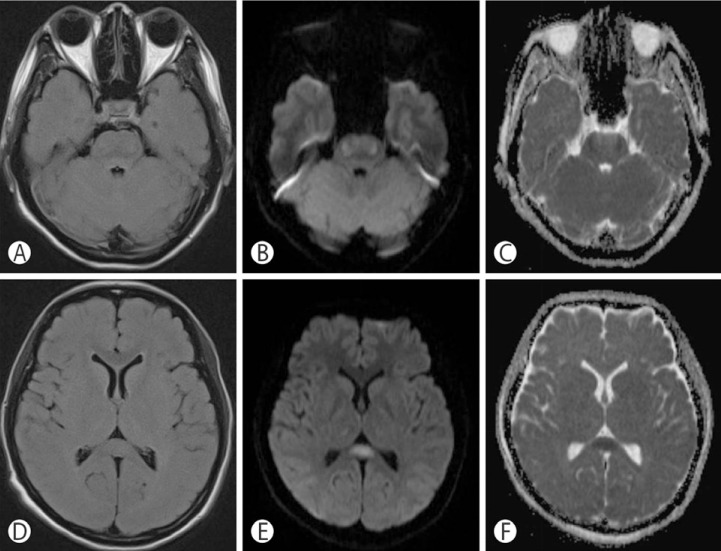
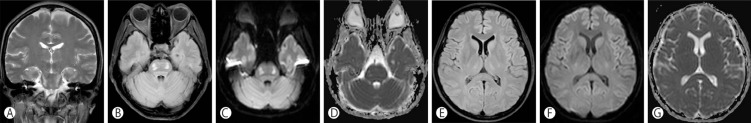
- Osmotic demyelination syndrome is a demyelinating disorder associated with rapid correction of hyponatremia. But, it rarely occurs in acute hypernatremia, and it leads to permanent neurologic symptoms and is associated with high mortality. A 44-year-old woman treated with alternative medicine was admitted with a history of drowsy mental status. Severe hypernatremia (197mEq/L) with hyperosmolality (415mOsm/kgH2O) was evident initially and magnetic resonance imaging revealed a high signal intensity lesion in the pons, consistent with central pontine myelinolysis. She was treated with 0.45% saline and 5% dextrose water and intravenous corticosteroids. Serum sodium normalized and her clinical course gradually improved. Brain lesion of myelinolysis also improved in a follow-up imaging study. This is the first report of a successful treatment of hypernatremia caused by iatrogenic salt intake, and it confirms the importance of adequate fluid supplementation in severe hypernatremia.
MeSH Terms
Figure
Reference
-
1. Samuels MA, Seifter JL. Encephalopathies caused by electrolyte disorders. Semin Neurol. 2011; 31:135–138. PMID: 21590618.
Article2. Naik KR, Saroja AO. Seasonal postpartum hypernatremic encephalopathy with osmotic extrapontine myelinolysis and rhabdomyolysis. J Neurol Sci. 2010; 291:5–11. PMID: 20129624.
Article3. Arieff AI. Central nervous system manifestations of disordered sodium metabolism. Clin Endocrinol Metab. 1984; 13:269–294. PMID: 6488574.
Article5. An JY, Park SK, Han SR, Song IU. Central pontine and extrapontine myelinolysis that developed during alcohol withdrawal, without hyponatremia, in a chronic alcoholic. Intern Med. 2010; 49:615–618. PMID: 20228603.
Article6. Ismail FY, Szollics A, Szolics M, Nagelkerke N, Ljubisavljevic M. Clinical semiology and neuroradiologic correlates of acute hypernatremic osmotic challenge in adults: A literature review. Am J Neuroradiol. 2013; 34:2225–2232. PMID: 23413245.
Article7. Machino T, Yoshizawa T. Brain shrinkage due to acute hypernatremia. Neurology. 2006; 67:880. PMID: 16966557.
Article8. Ayus JC, Armstrong DL, Arieff AI. Effects of hypernatraemia in the central nervous system and its therapy in rats and rabbits. J Physiol. 1996; 492:243–255. PMID: 8730599.
Article10. Sugimura Y, Murase T, Takefuji S, Hayasaka S, Takagishi Y, Oiso Y, et al. Protective effect of dexamethasone on osmotic-induced demyelination in rats. Exp Neurol. 2005; 192:178–183. PMID: 15698632.
Article11. Sakamoto E, Hagiwara D, Morishita Y, Tsukiyama K, Kondo K, Yamamoto M. Complete recovery of central pontine myelinolysis by high dose pulse therapy with methylprednisolone. Nihon Naika Gakkai Zasshi. 2007; 96:2291–2293. PMID: 18044169.
Article12. Adler S, Verbalis JG, Meyers S, Simplaceanu E, Williams DS. Changes in cerebral blood flow and distribution associated with acute increases in plasma sodium and osmolality of chronic hyponatremic rats. Exp Neurol. 2000; 163:63–71. PMID: 10785445.
Article13. Cramer SC, Stegbauer KC, Schneider A, Mukai J, Maravilla KR. Decreased diffusion in central pontine myelinolysis. Am J Neuroradiol. 2001; 22:1476–1479. PMID: 11559493.14. Ruzek KA, Campeau NG, Miller GM. Early diagnosis of central pontine myelinolysis with diffusion-weighted imaging. Am J Neuroradiol. 2004; 25:210–213. PMID: 14970019.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Central and Extrapontine Myelinolysis after Alcohol Withdrawal and Correction of Hypernatremia in a Chronic Alcoholic: a Case Report
- Cortical Laminar Necrosis associated with Osmotic Demyelination Syndrome
- Initial Transient Neurologic Recovery Followed by Delayed Deterioration of Osmotic Demyelination Syndrome: A Case Report
- Osmotic Demyelination Syndrome Associated with Hypernatremia Caused by Lactulose Enema in a Patient with Chronic Alcoholism
- A Case of Obstructive Uropathy Accompanied with Severe Hypernatremia