Clin Endosc.
2013 May;46(3):306-309. 10.5946/ce.2013.46.3.306.
Hepatic and Splenic Infarction and Bowel Ischemia Following Endoscopic Ultrasound-Guided Celiac Plexus Neurolysis
- Affiliations
-
- 1Institute for Digestive Research, Digestive Disease Center, Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea. swcha@schmc.ac.kr
- KMID: 2048940
- DOI: http://doi.org/10.5946/ce.2013.46.3.306
Abstract
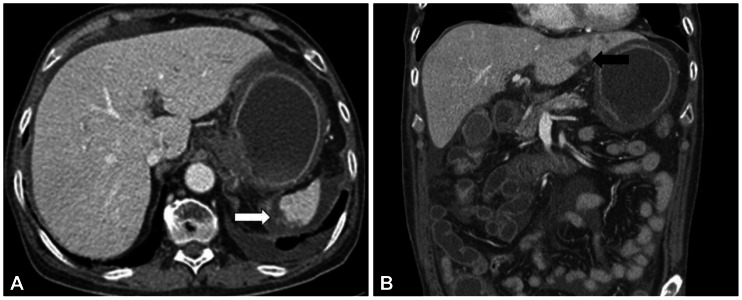
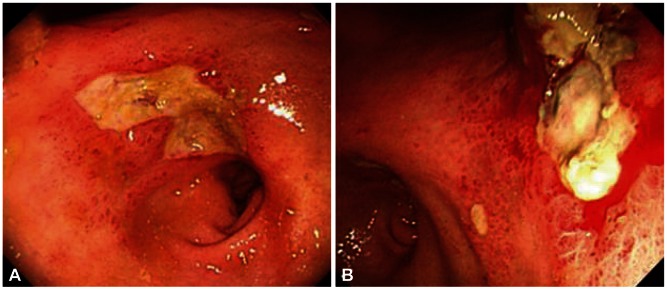
- Endoscopic ultrasound-guided celiac plexus neurolysis (EUS-CPN) is a well-established intervention to palliate malignant pain. We report a patient who developed hepatic and splenic infarction and bowel ischemia following EUS-CPN. A 69-year-old man with known lung cancer and pancreatic metastasis was transferred for debilitating, significant epigastric pain for several months. The patient underwent EUS-CPN to palliate the pain. After the procedure, the patient complained continuously of abdominal pain, nausea, and vomiting; hematemesis and hematochezia were newly developed. Abdominal computed tomography revealed infarction of the liver and spleen and ischemia of the stomach and proximal small bowel. On esophagogastroduodenoscopy, hemorrhagic gastroduodenitis, and multiple gastric ulcers were noted without active bleeding. The patient expired on postoperative day 27 despite the best supportive care.
Keyword
MeSH Terms
Figure
Reference
-
1. Pello S, Miller A, Ku T, Wang D. Hemorrhagic gastritis and duodenitis following celiac plexus neurolysis. Pain Physician. 2009; 12:1001–1003. PMID: 19935986.2. Mercadante S, Nicosia F. Celiac plexus block: a reappraisal. Reg Anesth Pain Med. 1998; 23:37–48. PMID: 9552777.
Article3. O'Toole TM, Schmulewitz N. Complication rates of EUS-guided celiac plexus blockade and neurolysis: results of a large case series. Endoscopy. 2009; 41:593–597. PMID: 19588286.4. Ahmed HM, Friedman SE, Henriques HF, Berk BS. End-organ ischemia as an unforeseen complication of endoscopic-ultrasound-guided celiac plexus neurolysis. Endoscopy. 2009; 41(Suppl 2):E218–E219. PMID: 19757362.
Article5. Buckley NM, Brazeau P, Frasier ID, Gootman PM. Circulatory effects of splanchnic nerve stimulation in developing swine. Am J Physiol. 1985; 248(1 Pt 2):H69–H74. PMID: 3970177.
Article6. Yang Z, Wang J, Zheng T, Altura BT, Altura BM. Importance of extracellular Ca2+ and intracellular Ca2+ release in ethanol-induced contraction of cerebral arterial smooth muscle. Alcohol. 2001; 24:145–153. PMID: 11557300.
Article7. Eisenberg E, Carr DB, Chalmers TC. Neurolytic celiac plexus block for treatment of cancer pain: a meta-analysis. Anesth Analg. 1995; 80:290–295. PMID: 7818115.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic ultrasound-guided celiac plexus neurolysis for managing abdominal pain related with advanced cancer
- A Case of Pancreatic Cancer and Opioid Withdrawal after Endoscopic Ultrasound-guided Celiac Plexus Neurolysis
- Role of interventional endoscopic ultrasound in a developing country
- Endoscopic Ultrasound-Guided Treatment beyond Drainage: Hemostasis, Anastomosis, and Others
- CT Guided Celiac Plexus Block