Ann Surg Treat Res.
2015 Jul;89(1):17-22. 10.4174/astr.2015.89.1.17.
The effects of ventilation with high density oxygen on the strength of gastrointestinal anastomosis
- Affiliations
-
- 1Department of General Surgery, Ankara University Medical School, Ankara, Turkey. volkangenc77@yahoo.com
- 2Department of General Surgery, Ankara Penal Institution Campus State Hospital, Ankara, Turkey.
- 3Ankara University Biotechnology Institute, Ankara, Turkey.
- 4Department of Anesthesiology and Reanimation, Ankara University Medical School, Ankara, Turkey.
- 5Department of General Surgery, Antalya Education and Training Hospital, Antalya, Turkey.
- 6Department of Medical Biochemistry, Gazi University Medical School, Ankara, Turkey.
- KMID: 2047709
- DOI: http://doi.org/10.4174/astr.2015.89.1.17
Abstract
- PURPOSE
The aim of our study is to evaluate the effects of administration of perioperative supplemental oxygen on anastomoses.
METHODS
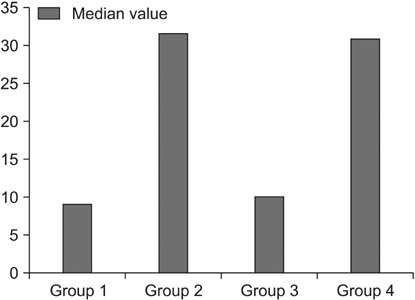
Forty male Wistar albino rats were used in the study and randomized into 4 groups. Ischemia-reperfusion models were built in groups 3 and 4. Jejunojejunostomy was performed in all rats and assigned to an oxygen/nitrous oxide mixture with a fraction of inspired oxygen of 30% in groups 1 and 3 and 80% in groups 2 and 4. The measurements of perianastomotic tissue oxygen pressure, bursting pressure, level of hydroxyproline were evaluated and compared in all groups.
RESULTS
The perianastomotic tissue oxygen pressures, bursting pressures and levels of hydroxyproline were identified as significantly high in groups 2 and 4, administered a fraction of inspired oxygen of 80%, compared to groups 1 and 3, administered a fraction of inspired oxygen of 30%.
CONCLUSION
Perioperative supplemental oxygen contributes positively to the anastomotic healing.
Keyword
Figure
Reference
-
1. Chen C. The art of bowel anastomosis. Scand J Surg. 2012; 101:238–240.2. Sheridan WG, Lowndes RH, Young HL. Tissue oxygen tension as a predictor of colonic anastomotic healing. Dis Colon Rectum. 1987; 30:867–871.3. Garcia-Botello SA, Garcia-Granero E, Lillo R, Lopez-Mozos F, Millan M, Lledo S. Randomized clinical trial to evaluate the effects of perioperative supplemental oxygen administration on the colorectal anastomosis. Br J Surg. 2006; 93:698–706.4. Belda FJ, Aguilera L, Garcia de la Asuncion J, Alberti J, Vicente R, Ferrandiz L, et al. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA. 2005; 294:2035–2042.5. Hunt TK, Pai MP. The effect of varying ambient oxygen tensions on wound metabolism and collagen synthesis. Surg Gynecol Obstet. 1972; 135:561–567.6. Greif R, Akca O, Horn EP, Kurz A, Sessler DI. Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000; 342:161–167.7. Brasel K, McRitchie D, Dellinger P. EBRS Group. Canadian Association of General Surgeons and American College of Surgeons Evidence Based Reviews in Surgery. 21: the risk of surgical site infection is reduced with perioperative oxygen. Can J Surg. 2007; 50:214–216.8. Mayzler O, Weksler N, Domchik S, Klein M, Mizrahi S, Gurman GM. Does supplemental perioperative oxygen administration reduce the incidence of wound infection in elective colorectal surgery? Minerva Anestesiol. 2005; 71:21–25.9. Pryor KO, Fahey TJ 3rd, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgical population: a randomized controlled trial. JAMA. 2004; 291:79–87.10. Qadan M, Akca O, Mahid SS, Hornung CA, Polk HC Jr. Perioperative supplemental oxygen therapy and surgical site infection: a meta-analysis of randomized controlled trials. Arch Surg. 2009; 144:359–366.11. Al-Niaimi A, Safdar N. Supplemental perioperative oxygen for reducing surgical site infection: a meta-analysis. J Eval Clin Pract. 2009; 15:360–365.12. Turan A, Apfel CC, Kumpch M, Danzeisen O, Eberhart LH, Forst H, et al. Does the efficacy of supplemental oxygen for the prevention of postoperative nausea and vomiting depend on the measured outcome, observational period or site of surgery? Anaesthesia. 2006; 61:628–633.13. Schietroma M, Cecilia EM, Sista F, Carlei F, Pessia B, Amicucci G. High-concentration supplemental perioperative oxygen and surgical site infection following elective colorectal surgery for rectal cancer: a prospective, randomized, double-blind, controlled, single-site trial. Am J Surg. 2014; 208:719–726.14. DuBois AB, Turaids T, Mammen RE, Nobrega FT. Pulmonary atelectasis in subjects breathing oxygen at sea level or at simulated altitude. J Appl Physiol. 1966; 21:828–836.15. Caldwell PR, Lee WL Jr, Schildkraut HS, Archibald ER. Changes in lung volume, diffusing capacity, and blood gases in men breathing oxygen. J Appl Physiol. 1966; 21:1477–1483.16. Montgomery AB, Luce JM, Murray JF. Retrosternal pain is an early indicator of oxygen toxicity. Am Rev Respir Dis. 1989; 139:1548–1550.17. Schietroma M, Carlei F, Cecilia EM, Piccione F, Bianchi Z, Amicucci G. Colorectal Infraperitoneal anastomosis: the effects of perioperative supplemental oxygen administration on the anastomotic dehiscence. J Gastrointest Surg. 2012; 16:427–434.18. Kimberger O, Fleischmann E, Brandt S, Kugener A, Kabon B, Hiltebrand L, et al. Supplemental oxygen, but not supplemental crystalloid fluid, increases tissue oxygen tension in healthy and anastomotic colon in pigs. Anesth Analg. 2007; 105:773–779.19. Cohen IK, Diegelmann RF, Lindblad WJ. Wound healing: biochemical & clinical aspects. Philadelphia: W.B. Saunders Co.;1992.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Respiratory Effects of Acute Coronary Embolism
- A Case of high-Frequency Oscillatory Ventilation
- Comparison of Oxygenation and Lung Damage of High Frequency Flow Interruption to Conventional Ventilation in Surfactant Deficient Rabbits
- The Study of Fraction of Delivered Oxygen in Laerdal Resuscitator Bag
- The effects of inspiratory to expiratory ratio on ventilation and oxygenation during high frequency partial liquid ventilation in a rabbit model of acute lung injury