J Korean Soc Spine Surg.
2006 Mar;13(1):16-22. 10.4184/jkss.2006.13.1.16.
Augmentation of Anterior Vertebral Screws Using Direct Anterior Vertebroplasty in the Porcine Model
- Affiliations
-
- 1Department of Orthopaedic Surgery, Asan Medical Center, College of Medicine, Ulsan Univerity, Korea.
- 2Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. ortho@hananet.net
- KMID: 2040776
- DOI: http://doi.org/10.4184/jkss.2006.13.1.16
Abstract
-
STUDY DESIGN: A biomechanical study using the porcine spine.
OBJECTIVES
To investigate the efficacy of direct anterior vertebroplasty [Polymethylmetacrylic acid (PMMA) augmentation] with anterior vertebral screw fixation. SUMMARY AND LITERATURE REVIEW: We are not aware of any previous reports that described this technique.
MATERIALS AND METHODS
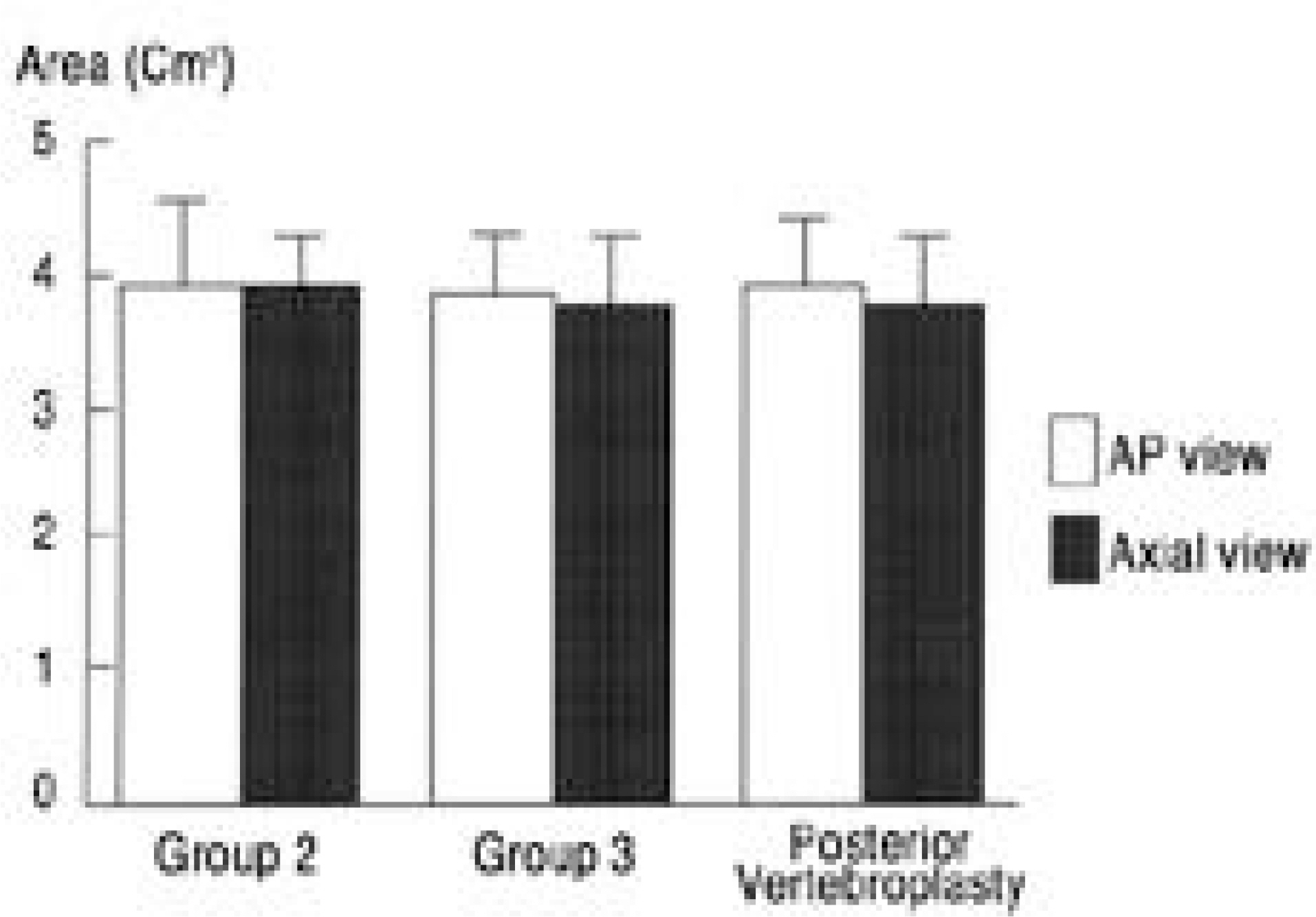
Thirty out of 35 fresh porcine lumbar vertebral bodies (L1-5) were instrumented with single anteriorvertebral screws using different augmentation methods. In group 1 (n=10), the non-augmented group, each vertebral body was pre-drilled and an anterior vertebral screw was inserted unicortically at 90 degrees laterally. In groups 2 (n=10) and 3 (n=10), after the unicortical pre-drilling, 2 ml of PMMA were injected through an 11-gauge bone biopsy needle. The screw was inserted immediately after the cement injection in group 2, and after complete consolidation of the cement in group 3. Axial pullout loads to loosen the screws were measured. Conventional vertebroplasties via bilateral pedicles were performed in the other 5 vertebral bodies, the cement distribution areas of which were compared with the 5 specimens of groups 2 and 3, respectively, using radiomorphometry. The data were analyzed using the Mann-Whitney test.
RESULTS
The mean pullout loads were 459+/-111N in group 1, 1510+/-165N in group 2, and 1241+/-189N in group 3. The PMMA augmented anterior vertebral screws (groups 2 and 3) provided more than 100% of an increase in pullout strength compared with non-augmented screws (group 1) (P < 0.001). Among the augmented screws, the screws that were inserted during the consolidation of PMMA (group 2) had a greater resistance against pullout loads than did those that were inserted after complete consolidation (group 3) (P < 0.01). The cement distribution areas after the direct anterior vertebroplasties (groups 2 and 3) was no different than that after conventional posterior vertebroplasties (P > 0.05)
CONCLUSIONS
Direct anterior vertebroplasty is another effective augmentation method for anterior vertebral screw fixation. With this technique, we avoided an unnecessary posterior procedure and achieved a more rigid fixation because we could insert the screws during the consolidation of PMMA.
Figure
Reference
-
1). Cooper C Atkinson EJ, O'fallon WM, Melton LF III. Incidence of clinically diagnosed vertebral fractures: A population-based study in Rochester, Minnesota 1985-1989. J Bone Miner Res. 1992; 7:221–227.
Article2). Lim TH, An HS, Hong JH, et al. Biomechanical evaluation of anterior and posterior fixations in an unstable calf spine model. Spine. 1997; 22(3):261–266.
Article3). Shono Y, McAfee PC, Cunningham BW. Experimental study of thoracolumbar burst fractures. A radiographic and biomechanical analysis of anterior and posterior insturmentation systems. Spine. 1994; 19(15):1711–1722.4). Gurwitz GS, Dawson JM, McNamara MJ, Federspiel CF, Spengler DM. Biomechanical analysis of three surgical approaches for lumbar burst fractures using short-segment instrumentation. Spine. 1993; 18(8):977–982.
Article5). Oda I, Cunningham BW, Abumi K, Kaneda K, McAfee PC. The stability of reconstruction methods after thoracolumbar total spondylectomy. An in vitro investigation. Spine. 1999; 24(16):1634–1638.6). Kaneda K, Fujiya N, Satoh S. Results with Zielke instrumentation for idiopathic thoracolumbar and lumbar scoliosis. Clin Orthop. 1986; 205:195–203.
Article7). Kostuik JP, Carl A, Ferron S. Anterior Zielke instrumentation for spinal deformity in adults. J Bone Joint Surg Am. 1989; 71:898–912.
Article8). Moe JH, Purcell GA, Bradford DS. Zielke instumentation (VDS) for the correction of spinal curvature: analysis of results in 66 patients. Clin Orthop. 1983; 180:133–153.9). Korovessis PG, Deligianni D, Stamatakes M, Missirlis Y. Augmentation of anterior transvertebral screws using threaded teflon anchoring. J Spinal Disord. 1998; 11(4):300–306.
Article10). Lee YL, Yip KM. The osteoporotic spine. Clin Orthop. 1996; 323:91–97.
Article11). Hamilton A, Webb JK. The role of anterior surgery for vertebral fractures with and without cord compression. Clin Orthop. 1994; 300:79–89.
Article12). Kostuik JP, Errico TJ, Gleason TF. Techniques of internal fixation for degenerative conditions of the lumbar spine. Clin Orthop. 1986; 203-219:-231.
Article13). Lotz JC, Hu SS, Chiu DF, Yu M, Colliou O, Poser RD. Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine. 1997; 22:2716–2723.
Article14). Staffe AD, Biscup RS, Sitkowski DJ. Segmental spine plates with pedicle screw fixation: a new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop. 1986; 203:45–53.15). Weinstein JN, Rydevik BL, Rauschning W. Anat omic and technical considerations of pedicle screw fixation. Clin Orthop. 1992; 284:34–46.16). Wuisman PI, Van Dijk M, Staal H, Van Royen BJ. Augmentation of (pedicle) screws with calcium apatite cement in patients with severe progressive osteoporotic spinal deformities: An innovative technique. Eur Spine J. 2000; 9:528–533.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertebral Body Height Restoration after Vertebroplasty in Osteoporotic Vertebral Fracture
- Percutaneous Vertebroplasty: Considerations for the Safe Procedures
- Short-term Treatment Comparison of Teriparatide and Percutaneous Vertebroplasty in Patients with Acute Osteoporotic Vertebral Compression Fractures
- Posterior Surgery with Selective Anterior Reinforcement and Screw Augmentation for a Delayed Myelopathy from an Osteoporotic Vertebral Compression Fracture
- Vertebral Recompression after Vertebroplasty or Kyphoplasty