J Korean Neurotraumatol Soc.
2011 Oct;7(2):57-62. 10.13004/jknts.2011.7.2.57.
Comparison of Peri-Operative Effectiveness between Anterior-Posterior Approach and Posterior Only Approach in Metastatic Thoracic Spinal Tumor
- Affiliations
-
- 1Department Neurological Surgery, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea. srjeon@amc.seoul.kr
- KMID: 2019914
- DOI: http://doi.org/10.13004/jknts.2011.7.2.57
Abstract
OBJECTIVE
This paper shows the appropriate method of metastatic thoracic spine cord surgery by comparing survival, pain scale (Numeric Rating Scale) and Barthel index which are considered as the prognosis of surgery in anterior-posterior approach and posterior approach.
METHODS
The author has researched 61 cases of metastatic thoracic spine tumor operations; 10 cases of anterior-posterior approach and 51 cases of posterior approach, performed in this institution for 8 years from January 2001 to December 2008. The author has compared improvement of neurologic symptoms after surgery (improvement in ambulation), survival, pain scale (Numeric Rating Scale) and functional outcome according to Barthel index. Statistical analysis was done using Kaplan Meyer Survival analysis, Log-Rank test and Mann-Whitney test.
RESULTS
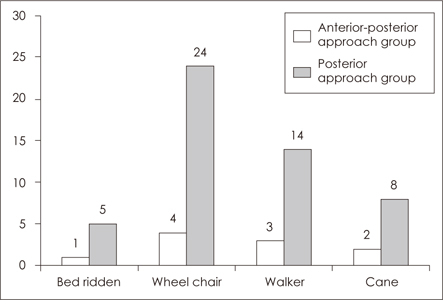
The average age of patients who received surgery were 56.8 years (35-72 years) and 53.9 years (26-75 years), in the anterior-posterior approach group and the posterior approach group respectively. The Barthel index increased from average 68.7 to 72.9 in the anterior-posterior approach group and 61.6 to 69.3 in the posterior approach group (p=0.027, p<0.001). Improvement in pain were 40% in the anterior-posterior approach group and 51% in the posterior approach on 1 month post-operation. Both posterior decompression and screw fixation were performed in both operations, and it has shown that there were no significant difference in survival, improvement of ambulation, improvement in pain and functional outcome compared with the anterior-posterior approach.
CONCLUSION
Considering similar survival and clinical outcomes, posterior approach can minimize morbidity related with operation.
Figure
Reference
-
1. Akeyson EW, McCutcheon IE. Single-stage posterior vertebrectomy and replacement combined with posterior instrumentation for spinal metastasis. J Neurosurg. 1996; 85:211–220.
Article2. Bach F, Larsen BH, Rohde K, Børgesen SE, Gjerris F, Bøge-Rasmussen T, et al. Metastatic spinal cord compression. Occurrence, symptoms, clinical presentations and prognosis in 398 patients with spinal cord compression. Acta Neurochir (Wien). 1990; 107:37–43.3. Barcena A, Lobato RD, Rivas JJ, Cordobes F, de Castro S, Cabrera A, et al. Spinal metastatic disease: analysis of factors determining functional prognosis and the choice of treatment. Neurosurgery. 1984; 15:820–827.
Article4. Black P. Spinal metastasis: current status and recommended guidelines for management. Neurosurgery. 1979; 5:726–746.5. Boland PJ, Lane JM, Sundaresan N. Metastatic disease of the spine. Clin Orthop Relat Res. 1982; 95–102.
Article6. Brice J, Mckissock W. Surgical treatment of malignant extradural spinal tumours. Br Med J. 1965; 1:1341–1344.
Article7. Bridwell KH, Jenny AB, Saul T, Rich KM, Grubb RL. Posterior segmental spinal instrumentation (PSSI) with posterolateral decompression and debulking for metastatic thoracic and lumbar spine disease. Limitations of the technique. Spine (Phila Pa 1976). 1988; 13:1383–1394.8. Bucy PC. The treatment of malignant tumors of the spine: a review. Neurology. 1963; 13:938–944.
Article9. Chadduck WM, Boop WC Jr. Acrylic stabilization of the cervical spine for neoplastic disease: evolution of a technique for vertebral body replacement. Neurosurgery. 1983; 13:23–29.
Article10. Constans JP, de Divitiis E, Donzelli R, Spaziante R, Meder JF, Haye C. Spinal metastases with neurological manifestations. Review of 600 cases. J Neurosurg. 1983; 59:111–118.11. Cooper PR, Errico TJ, Martin R, Crawford B, DiBartolo T. A systematic approach to spinal reconstruction after anterior decompression for neoplastic disease of the thoracic and lumbar spine. Neurosurgery. 1993; 32:1–8.
Article12. Cybulski GR, Stone JL, Opesanmi O. Spinal cord decompression via a modified costotransversectomy approach combined with posterior instrumentation for management of metastatic neoplasms of the thoracic spine. Surg Neurol. 1991; 35:280–285.
Article13. Cahill DW, Kumar R. Palliative subtotal vertebrectomy with anterior and posterior reconstruction via a single posterior approach. J Neurosurg. 1999; 90:1 Suppl. 42–47.
Article14. DeWald RL, Bridwell KH, Prodromas C, Rodts MF. Reconstructive spinal surgery as palliation for metastatic malignancies of the spine. Spine (Phila Pa 1976). 1985; 10:21–26.
Article15. Dunn EJ. The role of methylmethacrylate in the stabilization and replacement of the tumors of the cervical spine. Spine. 1977; 15–24.16. Faccioli F, Lima J, Bricolo A. One-stage decompression and stabilization in the treatment of spinal tumors. J Neurosurg Sci. 1985; 29:199–205.17. Fessler RG, Dietze DD Jr, Millan MM, Peace D. Lateral parascapular extrapleural approach to the upper thoracic spine. J Neurosurg. 1991; 75:349–355.
Article18. Fidler MW. Posterior instrumentation of the spine. An experimental comparison of various possible techniques. Spine (Phila Pa 1976). 1986; 11:367–372.19. Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: diagnosis and treatment. Ann Neurol. 1978; 3:40–51.
Article20. Greenberg HS, Kim JH, Posner JB. results with a new treatment protocol. Ann Neurol. 1980; 8:361–366.21. Hall AJ, Mackay NN. The results of laminectomy for compression of the cord or cauda equina by extradural malignant tumour. J Bone Joint Surg Br. 1973; 55:497–505.
Article22. Harrington KD. Anterior cord decompression and spinal stabilization for patients with metastatic lesions of the spine. J Neurosurg. 1984; 61:107–117.
Article23. Harrington KD. Anterior decompression and stabilization of the spine as a treatment for vertebral collapse and spinal cord compression from metastatic malignancy. Clin Orthop Relat Res. 1988; 177–197.
Article24. Harrington KD. The use of methlymethacrylate for vertebral-body replacement and anterior stabilization of pathological fracture-dislocations of the spine due to metastatic malignant disease. J Bone Joint Surg Am. 1981; 63:36–46.25. Heller JG, Zdeblick TA, Kunz DA, McCabe R, Cooke ME. Spinal instrumentation for metastatic disease: in vitro biomechanical analysis. J Spinal Disord. 1993; 6:17–22.26. Heller M, Perrin R, Macnab I. Treatment of metastatic disease of the spine with posterolateral decompression and luque instrumentation. Neuroorthopedics. 1986; 2:70–74.27. King GJ, Kostuik JP, McBroom RJ, Richardson W. Surgical management of metastatic renal carcinoma of the spine. Spine (Phila Pa 1976). 1991; 16:265–271.
Article28. Kostuik JP, Errico TJ, Gleason TF, Errico CC. Spinal stabilization of vertebral column tumors. Spine (Phila Pa 1976). 1988; 13:250–256.
Article29. McAfee PC, Bohlman HH. One-stage anterior cervical decompression and posterior stabilization with circumferential arthrodesis. A study of twenty-four patients who had a traumatic or a neoplastic lesion. J Bone Joint Surg Am. 1989; 71:78–88.
Article30. McAfee PC, Bohlman HH, Ducker T, Eismont FJ. Failure of stabilization of the spine with methylmethacrylate. A retrospective analysis of twenty-four cases. J Bone Joint Surg Am. 1986; 68:1145–1157.
Article31. Overby MC, Rothman AS. Anterolateral decompression for metastatic epidural spinal cord tumors. Results of a modified costotransversectomy approach. J Neurosurg. 1985; 62:344–348.32. Shaw B, Mansfield FL, Borges L. One-stage posterolateral decompression and stabilization for primary and metastatic vertebral tumors in the thoracic and lumbar spine. J Neurosurg. 1989; 70:405–410.
Article33. Siegal T, Siegal T. Surgical decompression of anterior and posterior malignant epidural tumors compressing the spinal cord: a prospective study. Neurosurgery. 1985; 17:424–432.
Article34. Siegal T, Tiqva P, Siegal T. Vertebral body resection for epidural compression by malignant tumors. Results of forty-seven consecutive operative procedures. J Bone Joint Surg Am. 1985; 67:375–382.
Article35. Sundaresan N, Choi IS, Hughes JE, Sachdev VP, Berenstein A. Treatment of spinal metastases from kidney cancer by presurgical embolization and resection. J Neurosurg. 1990; 73:548–554.
Article36. Sundaresan N, Digiacinto GV, Hughes JE, Cafferty M, Vallejo A. Treatment of neoplastic spinal cord compression: results of a prospective study. Neurosurgery. 1991; 29:645–650.
Article37. Sundaresan N, DiGiacinto GV, Krol G, Hughes JE. Spondylectomy for malignant tumors of the spine. J Clin Oncol. 1989; 7:1485–1491.
Article38. Sundaresan N, Galicich JH, Lane JM. Harrington rod stabilization for pathological fractures of the spine. J Neurosurg. 1984; 60:282–286.
Article39. Sundaresan N, Galicich JH, Lane JM, Bains MS, McCormack P. Treatment of neoplastic epidural cord compression by vertebral body resection and stabilization. J Neurosurg. 1985; 63:676–684.
Article40. Sundaresan N, Steinberger AA, Moore F, Sachdev VP, Krol G, Hough L, et al. Indications and results of combined anterior-posterior approaches for spine tumor surgery. J Neurosurg. 1996; 85:438–446.
Article41. Tokuhashi Y, Ajiro Y, Umezawa N. Outcome of treatment for spinal metastases using scoring system for preoperative evaluation of prognosis. Spine (Phila Pa 1976). 2009; 34:69–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- One Stage Three Column Fixation by Posterior Approach in Thoracolumbar Junction Lesion
- Surgical Treatment of Metastatic Spinal Tumor
- Lateral Extracavitary Approach to Thoracic Cord Tumor and Disc Herniation
- Three-column reconstruction through the posterior approach alone for the treatment of a severe lumbar burst fracture: a case report
- Unilateral Paramedian Transpedicular Approach for Repair of Anterior Transdural Spinal Cord Herniation: Report of a Case and Literature Review