J Korean Med Assoc.
2012 Dec;55(12):1201-1206. 10.5124/jkma.2012.55.12.1201.
New regimen of inhaled corticosteroid in preschool children with asthma
- Affiliations
-
- 1Department of Pediatrics, Inha University School of Medicine, Incheon, Korea. dhyunlim@inha.ac.kr
- 2Environmental Health Center for Allergic Disease, Ministry of Environment, Gwacheon, Korea.
- KMID: 2015665
- DOI: http://doi.org/10.5124/jkma.2012.55.12.1201
Abstract
- Daily low-dose inhaled corticosteroid in preschool children with asthma is recommended to prevent the development of asthma symptom and sign based on many asthma management guidelines. But the retarded growth after long-term steroid inhalation has been concerned. Recently the method of intermittent high-dose (suspension, 1,000 microg, 2 times a day for 7 days) budesonide inhalation when the initial phase to develop the asthma exacerbation was studied to compare the efficacy and safety with daily low-dose budesonide (500 microg) inhalation regimen in preschool children positive with modified asthma predictive index in recurrent wheezer during the study period with 52 weeks. There were no significant difference between two regimen with respect to the frequency of exacerbations, the time to the first exacerbation and to the second exacerbation, and the frequency of treatment failure. The total exposure to budesonide over the period was less in the intermittent high-dose regimen than in the daily low-dose regimen. There were no significant difference in change in height. But the change in height from baseline in intermittent high-dose regimen group was 8.01 cm and in daily low-dose was 7.76 cm. We need the more clinical studies in preschool children with persistent moderate and severe asthma and in various country and nations. It is suggested the intermittent high-dose budesonide inhalation regimen in preschool children with freqeunt wheezing may be a very good alternative to control the allergic inflammation and symptoms of asthma without concerning the adverse effect of steroid.
Keyword
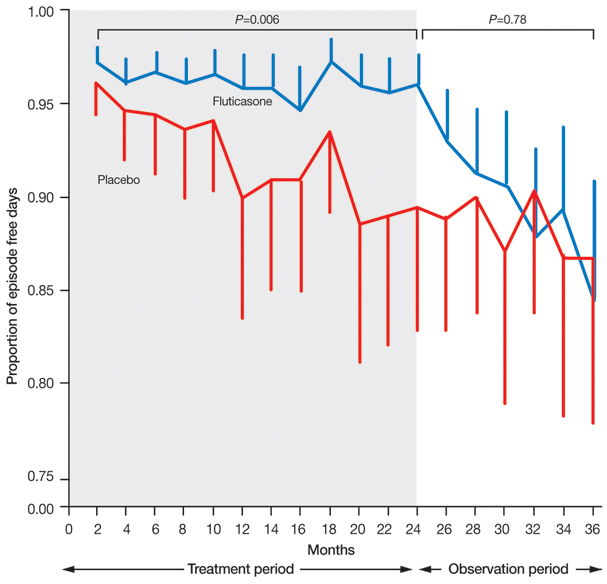
MeSH Terms
Figure
Reference
-
1. Korean Academy of Pediatric Allergy and Respiratory Disease. Asthma management guideline in children. 2008. Seoul: Kwangmoon.2. Kim BJ, Kim CW, Rha YH, Park YM, Song DJ, Yem HY, Lee JS, Chang YS, Cho YJ, Cho YS, Han MY, editors. Korean Academy of Asthma, Allergy, and Clinical Immunology. Asthma in children. Asthma and allergic diseases. 2012. 2nd ed. Seoul: Ryo Moon Gak;267–278.3. Ahn HS. Ahn HS, editor. Bronchial asthma. Pediatrics. 2012. Seoul: MiraeN;1132–1144.
Article4. National Heart Lung and Blood Institute. Expert panel report 3 (EPR-3): guidelines for the diagnosis and management of asthma: full report 2007 [Internet]. 2007. cited 2012 Nov 22. Bethesda: National Heart, Ling, and Blood Institute;Availabe from: http://www.nhlbi.nih.gov/guidelines/asthma.
Article5. Global Initiative for Asthma. Global strategy for asthma management and prevention. 2007. Bethesda: National Institutes of Health, National Heart, Lung, and Blood Institute.6. Global Initiative for Asthma. GINA report, global strategy for asthma management and prevention 2009 [Internet]. 2009. cited 2012 Nov 22. [place unknown]: Global Initiative for Asthma;Available from: http://www.ginasthma.org/Guidelines/guidelines-gina-report-global-strategy-for-asthma-management.html.7. Global Initiative for Asthma. GINA report, global strategy for the diagnosis and management of asthma in children 5 years and younger [Internet]. 2009. cited 2012 Nov 22. [place unknown]: Global Initiative for Asthma;Available from: http://www.ginasthma.org/uploads/users/files/GINA_Under5_2009_CorxAug11.pdf.8. Douglas G, Higgins B, Barnes N, Boyter A, Burge S, Cates C, Connett G, Couriel J, Cullinan P, Edwards S, Evans E, Fletcher M, Griffiths C, Heaney L, Boon MH, Holmes S, McArthur R, Nelson-Piercy C, Partridge M, Paton J, Pavord I, Carnegie E, Pinnock H, Qureshi S, Robertson C, Shields M, Warner J, White J. British guideline on the management of asthma: a national clinical guideline. Thorax. 2008. 63:Suppl 4. iv1–iv121.9. Nishimuta T, Kondo N, Hamasaki Y, Morikawa A, Nishima S. Japanese guideline for childhood asthma. Allergol Int. 2011. 60:147–169.
Article10. Bousquet J, Jeffery PK, Busse WW, Johnson M, Vignola AM. Asthma. From bronchoconstriction to airways inflammation and remodeling. Am J Respir Crit Care Med. 2000. 161:1720–1745.
Article11. The Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med. 2000. 343:1054–1063.
Article12. Guilbert TW, Morgan WJ, Zeiger RS, Mauger DT, Boehmer SJ, Szefler SJ, Bacharier LB, Lemanske RF Jr, Strunk RC, Allen DB, Bloomberg GR, Heldt G, Krawiec M, Larsen G, Liu AH, Chinchilli VM, Sorkness CA, Taussig LM, Martinez FD. Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med. 2006. 354:1985–1997.
Article13. Zeiger RS, Mauger D, Bacharier LB, Guilbert TW, Martinez FD, Lemanske RF Jr, Strunk RC, Covar R, Szefler SJ, Boehmer S, Jackson DJ, Sorkness CA, Gern JE, Kelly HW, Friedman NJ, Mellon MH, Schatz M, Morgan WJ, Chinchilli VM, Raissy HH, Bade E, Malka-Rais J, Beigelman A, Taussig LM. CARE Network of the National Heart, Lung, and Blood Institute. Daily or intermittent budesonide in preschool children with recurrent wheezing. N Engl J Med. 2011. 365:1990–2001.
Article14. Bisgaard H, Hermansen MN, Loland L, Halkjaer LB, Buchvald F. Intermittent inhaled corticosteroids in infants with episodic wheezing. N Engl J Med. 2006. 354:1998–2005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Bronchodilator and Corticosteroid Inhalation Therapy in Cough Variant Childhood Asthma
- Effect of Inhaled Corticosteroid and Leukotriene Receptor Antagonist in Cough-variant Asthma Patients under Five Years of Age
- A case of esophageal candidiasis caused by inhaled corticosteroid
- The role of inhaled and/or nasal corticosteroids on the bronchodilator response
- Size of Inhaled Corticosteroid and Small Airway Inflammation in Asthma