Korean J Obstet Gynecol.
2011 Apr;54(4):210-213. 10.5468/KJOG.2011.54.4.210.
A case of pelvic actinomycosis mistaken for advanced ovarian cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Dankook University College of Medicine, Cheonan, Korea. soo8541@hanmail.net
- KMID: 2013241
- DOI: http://doi.org/10.5468/KJOG.2011.54.4.210
Abstract
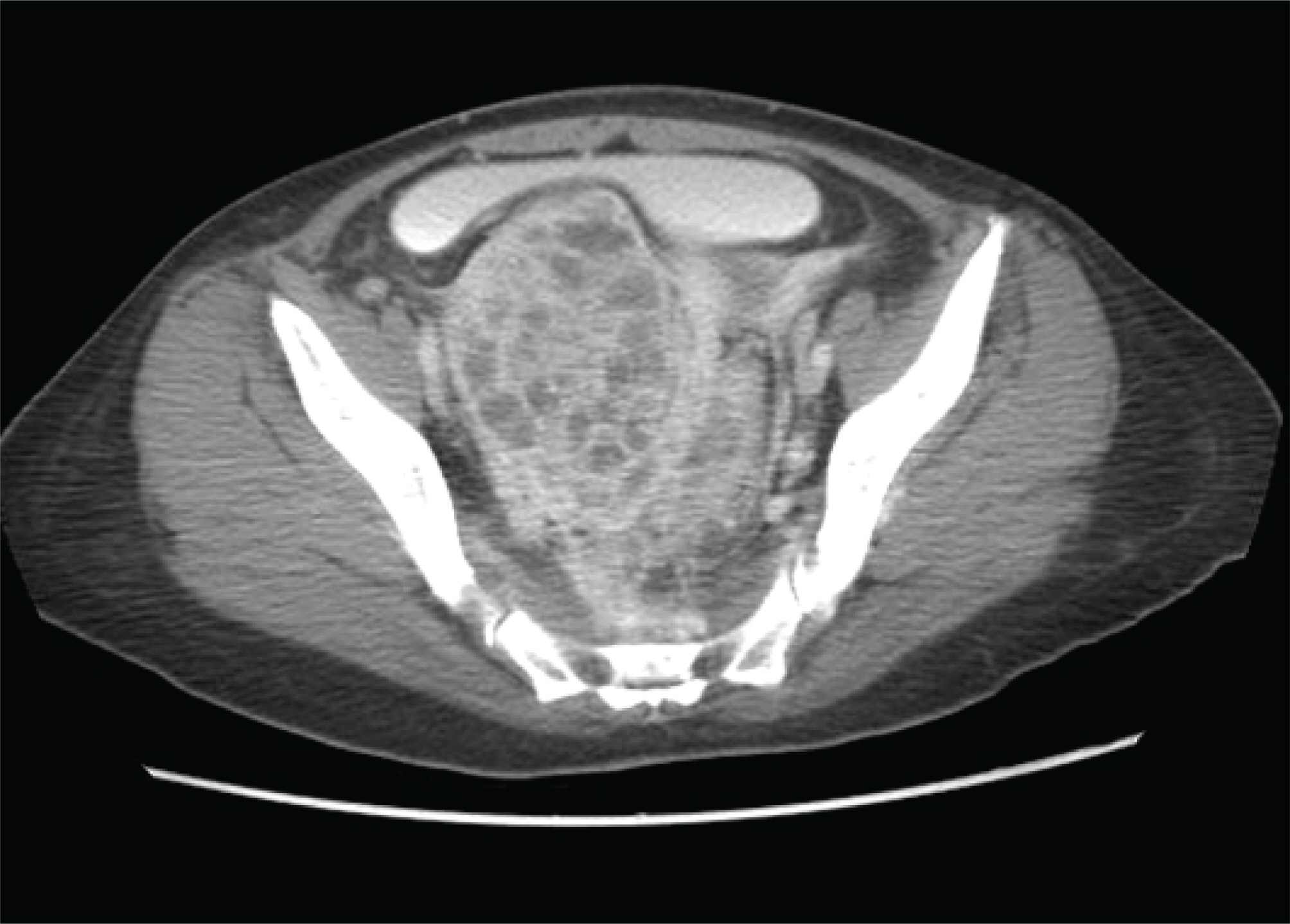
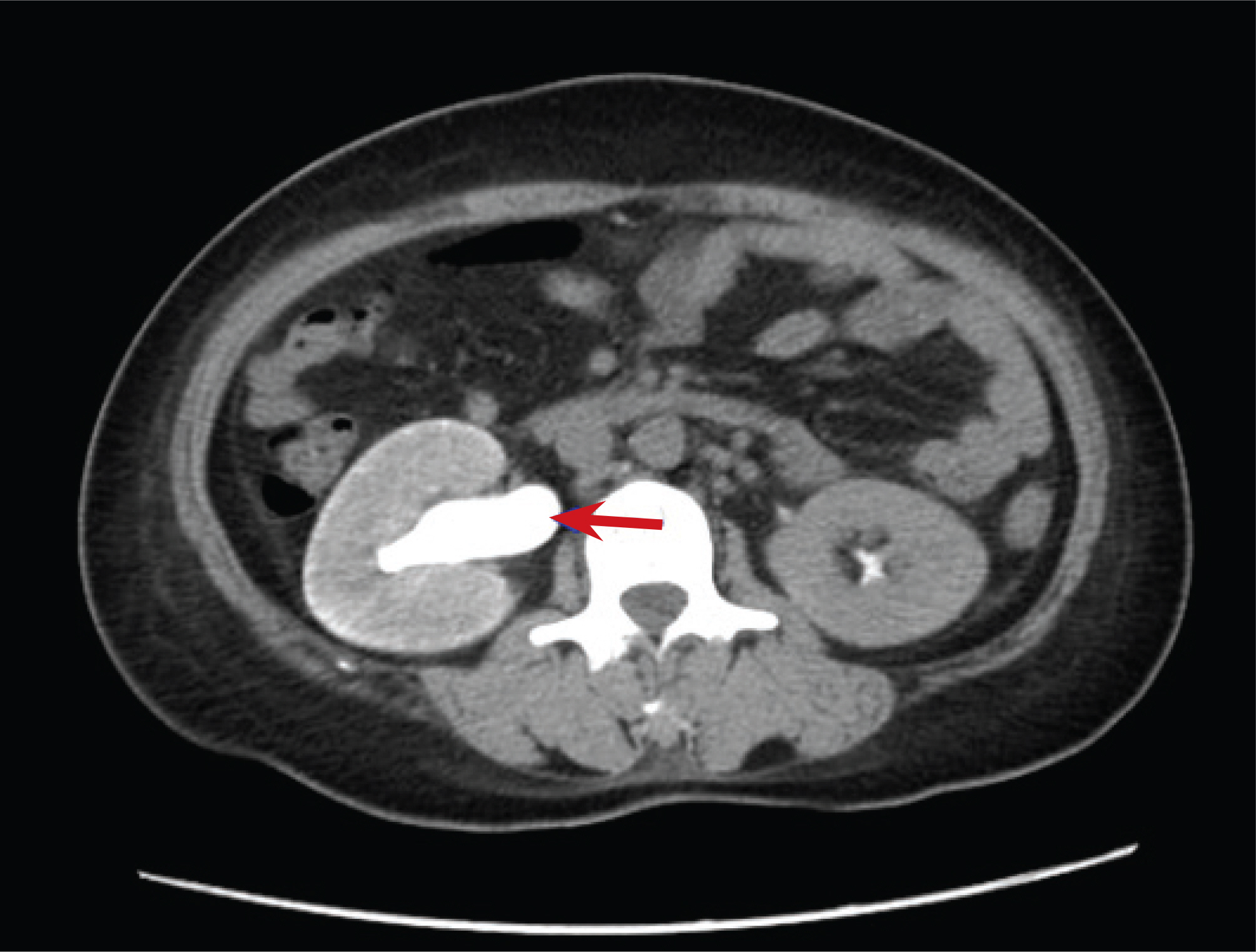
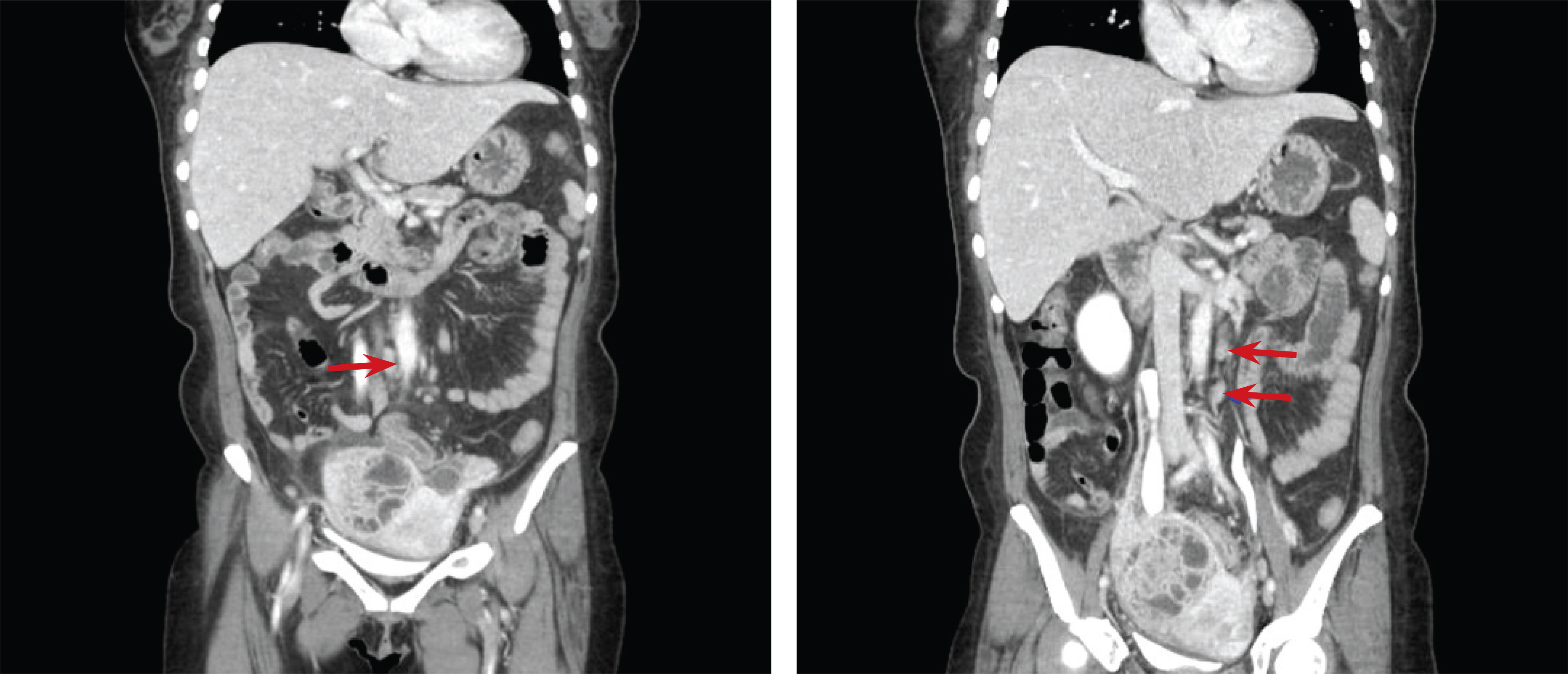
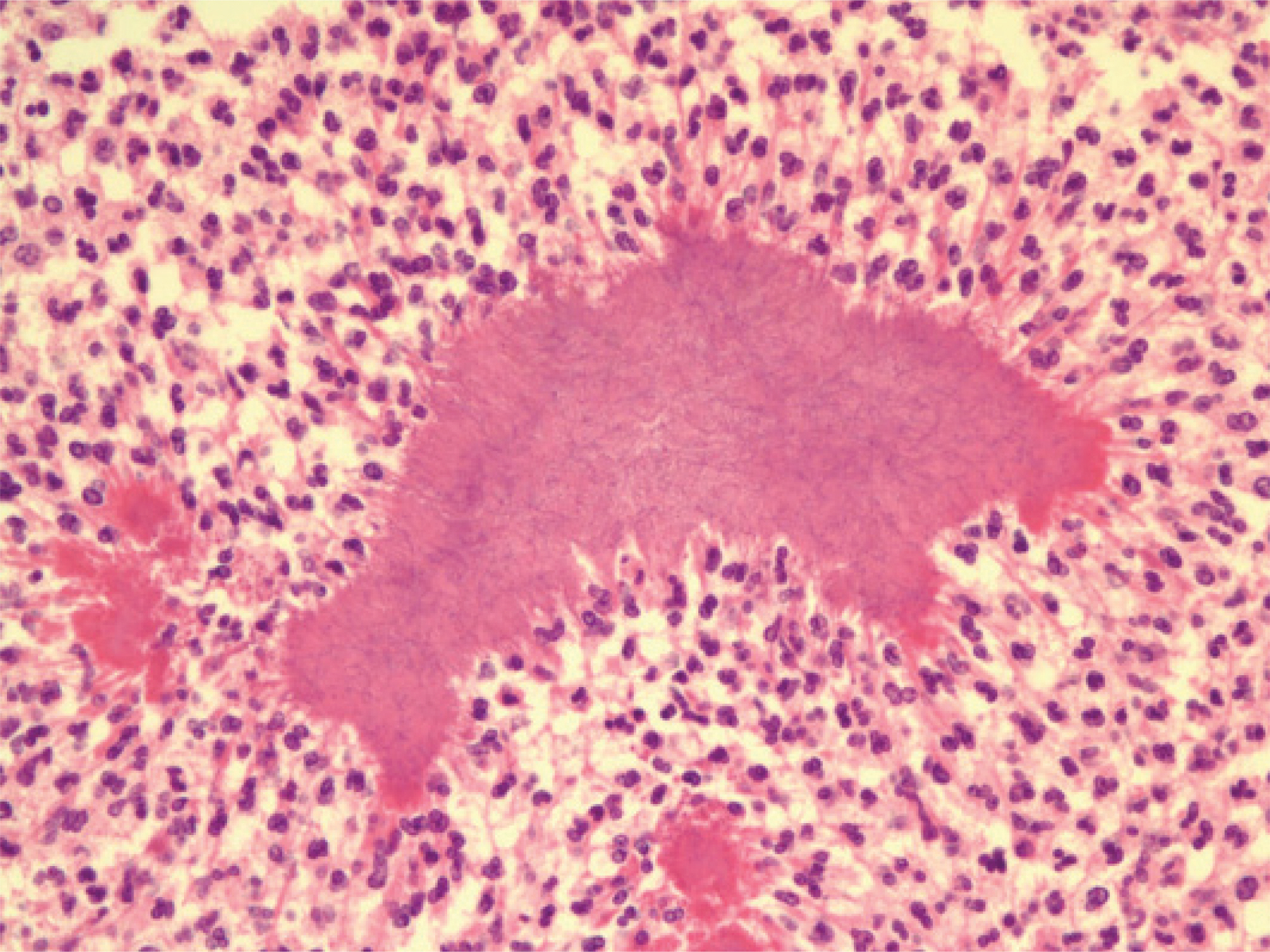
- Actinomycosis is a normal inhabitant of the mouth and gastrointestinal tract. Pelvic actinomycosis is a rare disease that can result in abscess formation, bowel obstruction, and other serious complications. Diagnosis can seldom be established before radical surgery because the disease often mimics pelvic neoplasms and depends on anaerobic culture or histologic identification of the organism. It has been recently recognized that pelvic actinomycosis is associated with long-term use of an intrauterine contraceptive device. But we had experienced a case of pelvic actinomycosis mimicking ovarian malignancy with a right hydronephrosis and lymph node enlargement in aortocarval and left paraaortic area in woman who did not use intra-uterine device.
Keyword
MeSH Terms
Figure
Reference
-
1. Choi PS, Kim SJ, Jeon HS, Hong HJ, Lee TU, Kim SY, et al. A case of pelvic and abdominal actinomycosis associated with wearing an intrauterine device. Korean J Obstet Gynecol. 2001; 44:1357–61.2. Bittar I, Solal JL, Cabanis P. Abdominopelvic actinomycosis. Ann Chir. 2001; 126:494–6.3. Kayikcioglu F, Akif Akgul M, Haberal A, Faruk Demir O. Actinomyces infection in female genital tract. Eur J Obstet Gynecol Reprod Biol. 2005; 118:77–80.
Article4. Marwah S, Marwah N, Singh I, Singh S, Gupta A, Jaiswal TS. Ovarian actinomycosis in absence of intrauterine contraceptive device: an unusual presentation. Acta Obstet Gynecol Scand. 2005; 84:602–3.
Article5. Cheong MA, Seo YS, Yang JS, Park JS, Youn JH, Lee JG, et al. A case of hydronephrosis as a complication of pelvic actinomycotic abscess. Korean J Nephrol. 2002; 21:337–40.6. Fiorino AS. Intrauterine contraceptive device-associated actinomycotic abscess and Actinomyces detection on cervical smear. Obstet Gynecol. 1996; 87:142–9.
Article7. Lim SY, Jeong DH, Lee KB. Pelvic actinomycosis with unilateral hydronephrosis and a rectal fistula mimicking an ovarian malignancy. J Womens Med. 2009; 2:158–61.8. Hager WD, Douglas B, Majmudar B, Naib ZM, Williams OJ, Ramsey C, et al. Pelvic colonization with actinomyces in women using intrauterine contraceptive devices. Am J Obstet Gynecol. 1979; 135:680–4.
Article9. Mali B, Joshi JV, Wagle U, Hazari K, Shah R, Chadha U, et al. Actinomyces in cervical smears of women using intrauterine contraceptive devices. Acta Cytol. 1986; 30:367–71.10. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 10-1992. A 41-year-old woman with a swollen left leg, pelvic mass, and bilateral hydronephrosis. N Engl J Med. 1992; 326:692–9.11. Lee HJ, Lee SJ, Kim YJ, Kim SH, Lee JH, Kim SR, et al. Preoperative diagnosis and medical treatment of pelvic actinomycosis. J Bacteriol Virol. 2008; 38:89–95.
Article12. Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic ‘failure’ with good prognosis after treatment. Arch Intern Med. 1975; 135:1562–8.
Article13. Nozawa H, Yamada Y, Muto Y, Arita S, Aisaka K. Pelvic actinomycosis presenting with a large abscess and bowel stenosis with marked response to conservative treatment: a case report. J Med Case Reports. 2007; 1:141.
Article14. Gupta PK, Hollander DH, Frost JK. Actinomycetes in cervicovaginal smears: an association with IUD usage. Acta Cytol. 1976; 20:295–7.15. Horn LC, Bilek K. Reactive and areactive actinomycosis infection of the female genitals and differentiation of pseudoacti-nomycosis. Zentralbl Gynakol. 1995; 117:466–71.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pelvic actinomycosis with hydronephrosis and colon stricture simulating an advanced ovarian cancer
- A Case of Pelvic Actinomycosis Simulating Metastatic Ovarian Cancer
- Ureteral Obstruction Caused by Pelvic Actinomycosis
- A case of pelvic actinomyosis presenting as an advanced ovarian malignancy
- Pelvic actinomycosis associated with bilateral hydronephrosis developed in a nulligravida woman