Korean J Obstet Gynecol.
2010 May;53(5):455-458. 10.5468/kjog.2010.53.5.455.
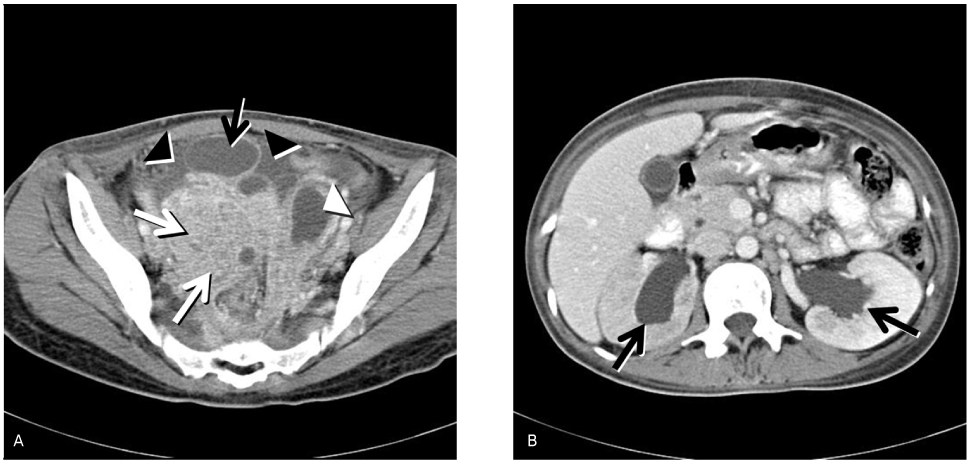
Pelvic actinomycosis associated with bilateral hydronephrosis developed in a nulligravida woman
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. dychang@paik.ac.kr
- KMID: 2273879
- DOI: http://doi.org/10.5468/kjog.2010.53.5.455
Abstract
- Pelvic actinomycosis is well-known to be associated with the longstanding use of intrauterine devices, sometimes related with a pregnancy history and an obstetric and/or gynecologic surgery. It can extend to the retroperitoneum and may also be associated with ureteral obstruction. In this case, pelvic actinomycosis in the form of bilateral tubo-ovarian abscess extending to the retroperitoneum resulting in bilateral hydronephrosis occurred in a nulligravida woman who had only few prior sexual intercourses. Apparently, pelvic actinomycosis can occur without any specific history. Moreover, such could possibly give rise to hydronephrosis by direct extension to the retroperitoneum.
MeSH Terms
Figure
Reference
-
1. Milam MR, Schultenover SJ, Crispens M, Parker L. Retroperitoneal fibrosis secondary to actinomycosis with no intrauterine device. Obstet Gynecol. 2004. 104:1134–1136.2. Zbar AP, Karayiannakis AJ, Chiappa AC. Obstructive uropathy and pelvic actinomycosis. Dis Colon Rectum. 2002. 45:1708.3. Russo TA. Mandell GL, Bennett JE, Dolin R, editors. Agents of actinomycosis. Principles and practice of infectious disease. 2005. 6th ed. Philadelphia: Churchill Livingstone;2924–2934.4. Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic 'failure' with good prognosis after treatment. Arch Intern Med. 1975. 135:1562–1568.5. Fiorino AS. Intrauterine contraceptive device-associated actinomycotic abscess and Actinomyces detection on cervical smear. Obstet Gynecol. 1996. 87:142–149.6. Hamid D, Baldauf JJ, Cuenin C, Ritter J. Treatment strategy for pelvic actinomycosis: case report and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2000. 89:197–200.7. O'Connor KF, Bagg MN, Croley MR, Schabel SI. Pelvic actinomycosis associated with intrauterine devices. Radiology. 1989. 170:559–560.8. Henderson SR. Pelvic actinomycosis associated with an intrauterine device. Obstet Gynecol. 1973. 41:726–732.9. Choi EN, Kim YM, Cha JM, Yoo HJ, Kim DY, Lee SS, et al. A clinical study of pelvic actinomycosis. Korean J Obstet Gynecol. 2002. 45:51–59.10. Hyung WJ, Kim MW, Kim MK, Chang DY, Jeon MK, Lee ES. 4 cases of pelvic actinomycosis associated with intrauterine contracptive device. Korean J Obstet Gynecol. 2005. 48:509–518.11. Lee JH, Kim JW, Lee JM, Park HT, Song JY, Lee KW. A clinical study of the treatment of pelvic actinomycosis. Korean J Obstet Gynecol. 2007. 50:1538–1543.12. Bae JJ, Kim JH, Park YK, Lee DJ, Koh MW, Lee TH, et al. A clinical analysis of pelvic actinomycosis. Korean J Obstet Gynecol. 2007. 50:1132–1140.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of pelvic actinomycosis mistaken for advanced ovarian cancer
- Pelvic actinomycosis with hydronephrosis and colon stricture simulating an advanced ovarian cancer
- A case of pelvic actinomyosis presenting as an advanced ovarian malignancy
- A Case of Pelvic Actinomycosis with Right Ureter Obstruction and Hydronephrosis
- Ureteral Obstruction Caused by Pelvic Actinomycosis