J Korean Neurosurg Soc.
2014 Aug;56(2):98-102. 10.3340/jkns.2014.56.2.98.
Intraoperative Monitoring of Motor-Evoked Potentials for Supratentorial Tumor Surgery
- Affiliations
-
- 1Department of Neurosurgery, St. Vincent's Hospital, The Catholic University of Korea, Suwon, Korea. 72ysh@catholic.ac.kr
- KMID: 1956510
- DOI: http://doi.org/10.3340/jkns.2014.56.2.98
Abstract
OBJECTIVE
The purpose of this study was to assess the feasibility and clinical efficacy of motor evoked potential (MEP) monitoring for supratentorial tumor surgery.
METHODS
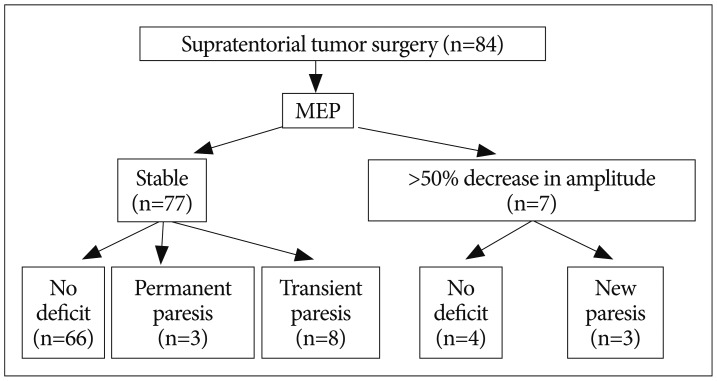
Between 2010 and 2012, to prevent postoperative motor deterioration, MEP recording after transcranial stimulation was performed in 84 patients with supratentorial brain tumors (45 males, 39 females; age range, 24-80 years; median age, 58 years). MEP monitoring results were correlated with postoperative motor outcome compared to preoperative motor status.
RESULTS
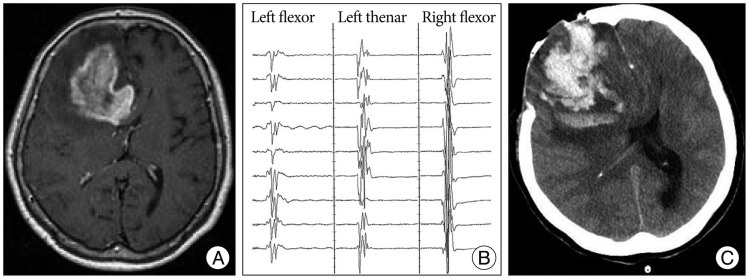
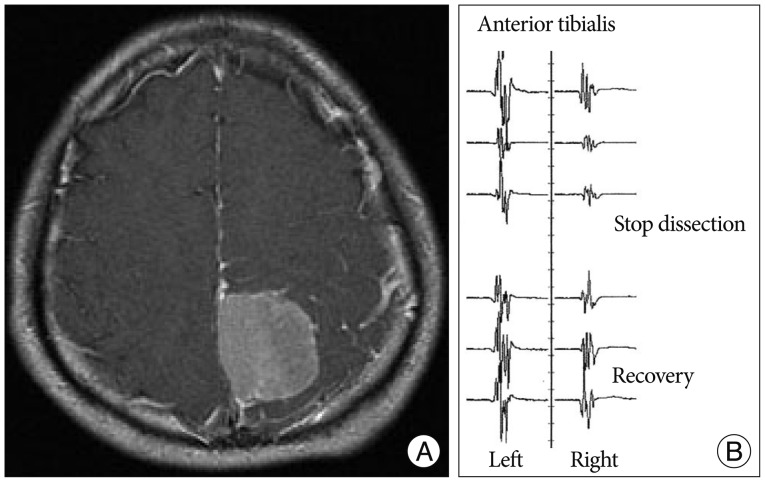
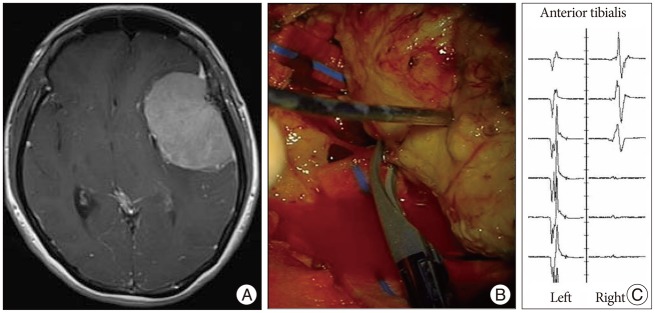
MEP recordings were stable in amplitude (<50% reduction in amplitude) during surgery in 77 patients (91.7%). No postoperative motor deficit was found in 66 out of 77 patients with stable MEP amplitudes. However, postoperative paresis developed in 11 patients. False negative findings were associated with edema in peri-resectional regions and postoperative bleeding in the tumor bed. MEP decrease in amplitude (>50%) occurred in seven patients (8.3%). However, no deficit occurred postoperatively in four patients following preventive management during the operation. Three patients had permanent paresis, which could have been associated with vascular injury during tumor resection.
CONCLUSIONS
MEP monitoring during supratentorial tumor surgery is feasible and safe. However, false negative MEP results associated with postoperative events may occur in some patients. To achieve successful monitoring, collaboration between surgeon, anesthesiologist and an experienced technician is mandatory.
MeSH Terms
Figure
Cited by 2 articles
-
Surgical Resection of Non-Glial Tumors in the Motor Cortex
Seong-Jong Lee, Sun-Chul Hwang, Soo Bin Im, Bum-Tae Kim
Brain Tumor Res Treat. 2016;4(2):70-76. doi: 10.14791/btrt.2016.4.2.70.Temporal Analysis of Postoperative Outcomes With or Without Intraoperative Motor Evoked Potentials and Somatosensory Evoked Potentials Monitoring for Intracranial Meningioma Surgery
Na Il Shin, Hye Jin Hong, Young Il Kim, Il Sup Kim, Jae Hoon Sung, Sang Won Lee, Seung Ho Yang
Brain Tumor Res Treat. 2024;12(1):50-57. doi: 10.14791/btrt.2023.0050.
Reference
-
1. Cabraja M, Stockhammer F, Mularski S, Suess O, Kombos T, Vajkoczy P. Neurophysiological intraoperative monitoring in neurosurgery : aid or handicap? An international survey. Neurosurg Focus. 2009; 27:E2. PMID: 19795951.2. Fukuda M, Oishi M, Takao T, Hiraishi T, Kobayashi T, Aoki H, et al. [Intraoperative monitoring of motor evoked potentials during glioma removal]. No Shinkei Geka. 2013; 41:219–227. PMID: 23459519.3. Gempt J, Krieg SM, Hüttinger S, Buchmann N, Ryang YM, Shiban E, et al. Postoperative ischemic changes after glioma resection identified by diffusion-weighted magnetic resonance imaging and their association with intraoperative motor evoked potentials. J Neurosurg. 2013; 119:829–836. PMID: 23829818.
Article4. Hashiguchi K, Morioka T, Yoshida F, Yoshimoto K, Shono T, Natori Y, et al. Feasibility of intraoperative motor-evoked potential monitoring for skull base tumors with a high risk of postoperative motor deterioration. Acta Neurochir (Wien). 2011; 153:1191–1200. discussion 1200. PMID: 21499783.
Article5. Horiuchi K, Suzuki K, Sasaki T, Matsumoto M, Sakuma J, Konno Y, et al. Intraoperative monitoring of blood flow insufficiency during surgery of middle cerebral artery aneurysms. J Neurosurg. 2005; 103:275–283. PMID: 16175857.
Article6. Iwasaki M, Kuroda S, Niiya Y, Ishikawa T, Iwasaki Y. Sensitivity of motor evoked potential (MEP) to intraoperative cerebral ischemia : case report. Jpn J Neurosurg (Tokyo). 2008; 17:622–626.
Article7. Kang D, Yao P, Wu Z, Yu L. Ischemia changes and tolerance ratio of evoked potential monitoring in intracranial aneurysm surgery. Clin Neurol Neurosurg. 2013; 115:552–556. PMID: 22795547.
Article8. Kombos T, Kopetsch O, Suess O, Brock M. Does preoperative paresis influence intraoperative monitoring of the motor cortex? J Clin Neurophysiol. 2003; 20:129–134. PMID: 12766686.
Article9. Kombos T, Suess O, Ciklatekerlio O, Brock M. Monitoring of intraoperative motor evoked potentials to increase the safety of surgery in and around the motor cortex. J Neurosurg. 2001; 95:608–614. PMID: 11596955.
Article10. Kong DS, Park K. Hemifacial spasm : a neurosurgical perspective. J Korean Neurosurg Soc. 2007; 42:355–362. PMID: 19096569.11. Langeloo DD, Lelivelt A, Louis Journée H, Slappendel R, de Kleuver M. Transcranial electrical motor-evoked potential monitoring during surgery for spinal deformity : a study of 145 patients. Spine (Phila Pa 1976). 2003; 28:1043–1050. PMID: 12768147.
Article12. MacDonald DB. Safety of intraoperative transcranial electrical stimulation motor evoked potential monitoring. J Clin Neurophysiol. 2002; 19:416–429. PMID: 12477987.
Article13. Neuloh G, Pechstein U, Cedzich C, Schramm J. Motor evoked potential monitoring with supratentorial surgery. Neurosurgery. 2004; 54:1061–1070. discussion 1070-1072. PMID: 15113459.
Article14. Neuloh G, Pechstein U, Schramm J. Motor tract monitoring during insular glioma surgery. J Neurosurg. 2007; 106:582–592. PMID: 17432707.
Article15. Quiñones-Hinojosa A, Lyon R, Zada G, Lamborn KR, Gupta N, Parsa AT, et al. Changes in transcranial motor evoked potentials during intramedullary spinal cord tumor resection correlate with postoperative motor function. Neurosurgery. 2005; 56:982–993. discussion 982-993. PMID: 15854246.16. Smith I, White PF, Nathanson M, Gouldson R. Propofol. An update on its clinical use. Anesthesiology. 1994; 81:1005–1043. PMID: 7943815.17. Son BC, Lee SW, Kim S, Hong JT, Sung JH, Yang SH. Transzygomatic approach with intraoperative neuromonitoring for resection of middle cranial fossa tumors. J Neurol Surg B Skull Base. 2012; 73:28–35. PMID: 23372992.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Neurophysiological Monitoring for Spinal Cord Tumor Surgery: Comparison of Motor and Somatosensory Evoked Potentials According to Tumor Types
- Monitoring of Motor and Somatosensory Evoked Potentials During Spine Surgery: Intraoperative Changes and Postoperative Outcomes
- Intraoperative Neurophysiologic Monitoring: Basic Principles and Recent Update
- Intraoperative Monitoring for Tethered Cord Syndrome Using Somatosensory Evoked Potential and Motor Evoked Potential: Report of three cases
- Intraoperative Monitoring of Hypoglossal Nerve Using Hypoglossal Motor Evoked Potential in Infratentorial Tumor Surgery: A Report of Two Cases