Ann Rehabil Med.
2017 Aug;41(4):610-620. 10.5535/arm.2017.41.4.610.
Intraoperative Neurophysiological Monitoring for Spinal Cord Tumor Surgery: Comparison of Motor and Somatosensory Evoked Potentials According to Tumor Types
- Affiliations
-
- 1Department of Rehabilitation Medicine and Rehabilitation Institute of Neuromuscular Disease, Yonsei University College of Medicine, Seoul, Korea. HANLEZZ@yuhs.ac
- KMID: 2389407
- DOI: http://doi.org/10.5535/arm.2017.41.4.610
Abstract
OBJECTIVE
To identify which combination of motor evoked potentials (MEPs) and somatosensory evoked potentials (SEPs) is most reliable for postoperative motor deterioration during spinal cord tumor surgery, according to anatomical and pathologic type.
METHODS
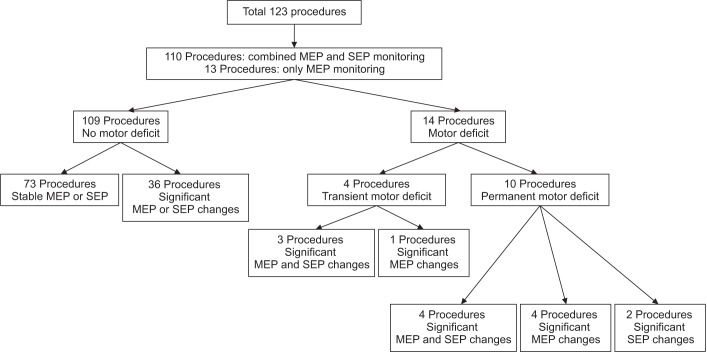
MEPs and SEPs were monitored in patients who underwent spinal cord tumor surgery between November 2012 and August 2016. Muscle strength was examined in all patients before surgery, within 48 hours postoperatively and 4 weeks later. We analyzed sensitivity, specificity, positive and negative predictive values of each significant change in SEPs and MEPs.
RESULTS
The overall sensitivity and specificity of SEPs or MEPs were 100% and 61.3%, respectively. The intraoperative MEP monitoring alone showed both higher sensitivity (67.9%) and specificity (83.2%) than SEP monitoring alone for postoperative motor deterioration. Two patients with persistent motor deterioration had significant changes only in SEPs. There are no significant differences in reliabilities between anatomical types, except with hemangioma, where SEPs were more specific than MEPs for postoperative motor deterioration. Both overall positive and negative predictive values of MEPs were higher than the predictive values of SEPs. However, the positive predictive value was higher by the dual monitoring of MEPs and SEPs, compared to MEPs alone.
CONCLUSION
For spinal cord tumor surgery, combined MEP and SEP monitoring showed the highest sensitivity for the postoperative motor deterioration. Although MEPs are more specific than SEPs in most types of spinal cord tumor surgery, SEPs should still be monitored, especially in hemangioma surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Lall RR, Lall RR, Hauptman JS, Munoz C, Cybulski GR, Koski T, et al. Intraoperative neurophysiological monitoring in spine surgery: indications, efficacy, and role of the preoperative checklist. Neurosurg Focus. 2012; 33:E10.
Article2. Malhotra NR, Shaffrey CI. Intraoperative electrophysiological monitoring in spine surgery. Spine (Phila Pa 1976). 2010; 35:2167–2179. PMID: 21102290.
Article3. Scibilia A, Terranova C, Rizzo V, Raffa G, Morelli A, Esposito F, et al. Intraoperative neurophysiological mapping and monitoring in spinal tumor surgery: sirens or indispensable tools? Neurosurg Focus. 2016; 41:E18. PMID: 27476842.
Article4. Kim DG, Son YR, Park YS, Hyun SJ, Kim KJ, Jahng TA, et al. Differences in multimodality intraoperative neurophysiological monitoring changes between spinal intramedullary ependymoma and hemangioblastoma. J Clin Neurophysiol. 2016; 33:120–126. PMID: 26690548.
Article5. Krammer MJ, Wolf S, Schul DB, Gerstner W, Lumenta CB. Significance of intraoperative motor function monitoring using transcranial electrical motor evoked potentials (MEP) in patients with spinal and cranial lesions near the motor pathways. Br J Neurosurg. 2009; 23:48–55. PMID: 19234909.
Article6. Sutter M, Eggspuehler A, Grob D, Jeszenszky D, Benini A, Porchet F, et al. The validity of multimodal intraoperative monitoring (MIOM) in surgery of 109 spine and spinal cord tumors. Eur Spine J. 2007; 16(Suppl 2):S197–S208. PMID: 17661095.
Article7. Cruccu G, Aminoff MJ, Curio G, Guerit JM, Kakigi R, Mauguiere F, et al. Recommendations for the clinical use of somatosensory-evoked potentials. Clin Neurophysiol. 2008; 119:1705–1719. PMID: 18486546.
Article8. Hirano K, Imagama S, Sato K, Kato F, Yukawa Y, Yoshihara H, et al. Primary spinal cord tumors: review of 678 surgically treated patients in Japan: a multicenter study. Eur Spine J. 2012; 21:2019–2026. PMID: 22581192.
Article9. Duong LM, McCarthy BJ, McLendon RE, Dolecek TA, Kruchko C, Douglas LL, et al. Descriptive epidemiology of malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumors, United States, 2004-2007. Cancer. 2012; 118:4220–4227. PMID: 22907705.
Article10. Seppala MT, Haltia MJ, Sankila RJ, Jaaskelainen JE, Heiskanen O. Long-term outcome after removal of spinal schwannoma: a clinicopathological study of 187 cases. J Neurosurg. 1995; 83:621–626. PMID: 7674010.11. Abul-Kasim K, Thurnher MM, McKeever P, Sundgren PC. Intradural spinal tumors: current classification and MRI features. Neuroradiology. 2008; 50:301–314. PMID: 18084751.
Article12. Ando K, Imagama S, Wakao N, Hirano K, Tauchi R, Muramoto A, et al. Single-stage removal of thoracic dumbbell tumors from a posterior approach only with costotransversectomy. Yonsei Med J. 2012; 53:611–617. PMID: 22477007.
Article13. Koeller KK, Rosenblum RS, Morrison AL. Neoplasms of the spinal cord and filum terminale: radiologic-pathologic correlation. Radiographics. 2000; 20:1721–1749. PMID: 11112826.
Article14. Macdonald DB. Intraoperative motor evoked potential monitoring: overview and update. J Clin Monit Comput. 2006; 20:347–377. PMID: 16832580.
Article15. Fehlings MG, Tator CH, Linden RD. The relationships among the severity of spinal cord injury, motor and somatosensory evoked potentials and spinal cord blood flow. Electroencephalogr Clin Neurophysiol. 1989; 74:241–259. PMID: 2471626.
Article16. Epstein FJ, Farmer JP, Freed D. Adult intramedullary spinal cord ependymomas: the result of surgery in 38 patients. J Neurosurg. 1993; 79:204–209. PMID: 8331401.
Article17. Loblaw DA, Laperriere NJ. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol. 1998; 16:1613–1624. PMID: 9552073.
Article18. Siegal T, Siegal T. Surgical decompression of anterior and posterior malignant epidural tumors compressing the spinal cord: a prospective study. Neurosurgery. 1985; 17:424–432. PMID: 4047353.
Article19. Lee JM, Kim DH, Kim HS, Choi BK, Han IH. The applicability of intraoperative neuromonitoring in patients with preoperative motor weakness during spine surgery. Korean J Spine. 2016; 13:9–12. PMID: 27123024.
Article20. Chang SH, Park YG, Kim DH, Yoon SY. Monitoring of motor and somatosensory evoked potentials during spine surgery: intraoperative changes and postoperative outcomes. Ann Rehabil Med. 2016; 40:470–480. PMID: 27446784.
Article21. Toleikis JR. American Society of Neurophysiological Monitoring. Intraoperative monitoring using somatosensory evoked potentials: a position statement by the American Society of Neurophysiological Monitoring. J Clin Monit Comput. 2005; 19:241–258. PMID: 16244848.22. Macdonald DB, Skinner S, Shils J, Yingling C. American Society of Neurophysiological Monitoring. Intraoperative motor evoked potential monitoring: a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol. 2013; 124:2291–2316. PMID: 24055297.23. Hilibrand AS, Schwartz DM, Sethuraman V, Vaccaro AR, Albert TJ. Comparison of transcranial electric motor and somatosensory evoked potential monitoring during cervical spine surgery. J Bone Joint Surg Am. 2004; 86-A:1248–1253. PMID: 15173299.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Monitoring of Motor and Somatosensory Evoked Potentials During Spine Surgery: Intraoperative Changes and Postoperative Outcomes
- Intraoperative Monitoring for Tethered Cord Syndrome Using Somatosensory Evoked Potential and Motor Evoked Potential: Report of three cases
- Intraoperative Neurophysiologic Monitoring: Basic Principles and Recent Update
- Changes of motor evoked potentials and spinal cord evoked potentials following spinal cord injury in rats
- Intraoperative Monitoring Using Somatosensory Evoked Potential during Spinal Deformity Surgery