J Korean Orthop Assoc.
2007 Dec;42(6):756-763. 10.4055/jkoa.2007.42.6.756.
The Primary Malignant Bone Tumors of Distal Tibia: Comparison between Limb Salvage and Amputation
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea Cancer Center Hospital, Seoul, Korea. chomanner@hanmail.net
- KMID: 1947782
- DOI: http://doi.org/10.4055/jkoa.2007.42.6.756
Abstract
-
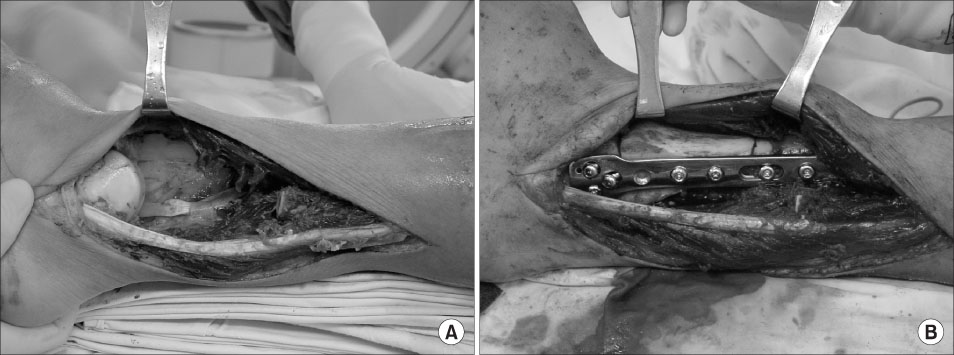
PURPOSE: The long term survival and indications of limb salvage surgery for primary malignant bone tumors of the distal tibia were evaluated, and the results of the reconstruction method using a pasteurized autograft alone or a pasteurized autograft and living fibular bone graft composite were examined.
MATERIALS AND METHODS
From March 1985 to June 2004, 13 cases were considered eligible. The diagnosis included 9 osteosarcomas, 2 chondrosarcomas, 1 parosteal osteosarcoma, and 1 malignant fibrous histiocytoma of the bone. There was 1 case of stage IB, 1 IIA, and 11 IIB according to the Enneking classification. Each case underwent surgery and 10 cases underwent additional chemotherapy. Six cases underwent a below-knee amputation and 7 cases had limb salvage surgery. The reconstruction methods were pasteurized bone alone (5), an additional living fibula bone graft (1) or a living fibula bone graft alone (1).
RESULTS
There was no recurrence or metastasis at the final follow up. The MSTS functional score of the limb salvage group and amputation group were 85% and 82% respectively. Two out of 5 cases of reconstruction with pasteurized bone alone achieved bony union at 6 and 9 months after surgery. The remaining 3 cases showed nonunion and fractures of the pasteurized bone that was followed by an additional living fibula graft (2 cases) and cancellous iliac bone graft (1 case). Two cases of primary living fibula grafts are in the course of healing.
CONCLUSION
The prognosis was good. Neurovascular invasion by the tumor and the necessity of a radical soft tissue excision indicated an amputation. There was no difference in the functional outcome between the limb salvage group and amputation group. A reconstruction method using pasteurized bone has bio-mechanical and economical benefits. However, primary additional living fibular bone graft is a promising method.
MeSH Terms
Figure
Reference
-
1. Abudu A, Grimer RJ, Tillman RM, Carter SR. Endoprosthetic replacement of the distal tibia and ankle joint for aggressive bone tumours. Int Orthop. 1999. 23:291–294.
Article2. Bishop AT, Wood MB, Sheetz KK. Arthrodesis of the ankle with a free vascularized autogenous bone graft. Reconstruction of segmental loss of bone secondary to osteomyelitis, tumor or trauma. J Bone Joint Surg Am. 1995. 77:1867–1875.
Article3. Casadei R, Ruggieri P, Giuseppe T, Biagini R, Mercuri M. Ankle resection arthrodesis in patients with bone tumors. Foot Ankle Int. 1994. 15:242–249.
Article4. Chacha PB, Ahmed M, Daruwalla JS. Vascular pedicle graft of the ipsilateral fibula for non-union of the tibia with a large defect. An experimental and clinical study. J Bone Joint Surg Br. 1981. 63:244–253.
Article5. Duffy GP, Wood MB, Rock MG, Sim FH. Vascularized free fibular transfer combined with autografting for the management of fracture nonunions associated with radiation therapy. J Bone Joint Surg Am. 2000. 82:544–554.
Article6. Enneking WF, Spanier SS, Goodman MA. Current concepts review. The surgical staging of musculoskeletal sarcoma. J Bone Joint Surg Am. 1980. 62:1027–1030.
Article7. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993. 286:241–246.
Article8. Huvos AJ. Huvos AJ, editor. bone tumors. 1991. 1st ed. Philadelphia: Saunders Co;85–115.9. Lee SH, Kim HS, Park YB, Rhie TY, Lee HK. Prosthetic reconstruction for tumors of the distal tibia and fibula. J Bone Joint Surg Br. 1999. 81:803–807.10. Manabe J, Ahmed AR, Kawaguchi N, Matsumoto S, Kuroda H. Pasteurized autologous bone graft in surgery for bone and soft tissue sarcoma. Clin Orthop Relat Res. 2004. 419:258–266.
Article11. Ozaki T, Hillmann A, Wuisman P, Winkelmann W. Reconstruction of tibia by ipsilateral vascularized fibula and allograft. 12 cases with malignant bone tumors. Acta Orthop Scand. 1997. 68:298–301.
Article12. Sakayama K, Kidani T, Fujibuchi T, Kamogawa J, Yamamoto H, Shibata T. Reconstruction surgery for patients with musculoskeletal tumor, using a pasteurized autogenous bone graft. Int J Clin Oncol. 2004. 9:167–173.
Article13. Shapiro MS, Endrizzi DP, Cannon RM, Dick HM. Treatment of tibial defects and nonunions using ipsilateral vascularized fibular transposition. Clin Orthop Relat Res. 1993. 296:207–212.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pathologic Fracture of Primary Malignant Bone Tumor: Survival, Limb Salvage, Local recurrence
- Endoprosthetic Reconstruction in the Limb Salvage Surgery for Treatment of Malignant Bone Tumors
- Treatment of Malignant Bone Tumors by Tumor Prosthesis
- Functional Evaluation of Tumor Prosthetic Arthroplasty for the Malignant Bone Tumor around the Knee: Interim Report
- Limb Salvage with Low and Heat Treated Autobone