Korean J Urol.
2007 Jan;48(1):61-65. 10.4111/kju.2007.48.1.61.
Testicular Injuries-Efficacy of the Organ Injury Scale Developed by the American Association for the Surgery of Trauma
- Affiliations
-
- 1Department of Urology, Seoul Adventist Hospital, Kyung Hee University, Seoul, Korea.
- 2Department of Urology, School of Medicine, Kyung Hee University, Seoul, Korea. sjlee@khu.ac.kr
- KMID: 1915023
- DOI: http://doi.org/10.4111/kju.2007.48.1.61
Abstract
-
PURPOSE: According to the AAST (American Association for the Surgery of Trauma) injuries to the testes are rare, but there are many reports in the literature on other organs using the AAST Organ Injury Scale (OIS). In the present study, the authors evaluated the usefulness of the AAST OIS when applied to the testis.
MATERIALS AND METHODS
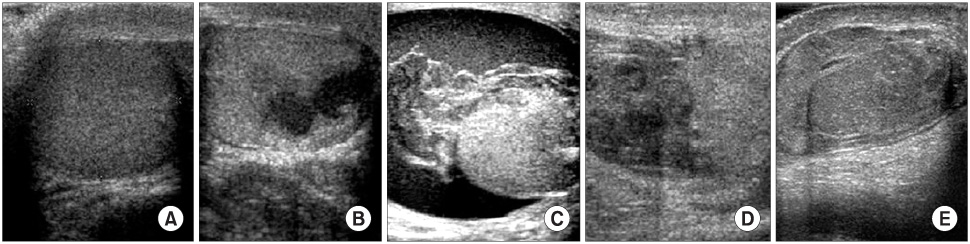
A retrospective review was performed on 65 patients (mean age 30.0 years) with a testis injury treated between March 1986 and July 2006. Of the 65 patients, preoperative ultrasonography was performed on 51. Injuries were classified according to the OIS of the AAST, based on history taking, a physical examination and scrotal ultrasonography.
RESULTS
Of the 51 patients, 46 and 5 underwent surgical intervention and conservative management, respectively. Of the included patients, 38 were found to have abnormal testis contours on ultrasonography, 29 had a rupture of the tunica albuginea, with a sensitivity of 76.3%. Of the 13 patients with normal contours, the tunica albuginea was normal in 7, and 8 underwent operation, with a specificity of 87.5%. Of the 12 Grade I patients, 7 underwent an operation, but the testes contours were normal. Of the 8 Grade II patients, only 1 underwent a primary repair with partial orchiectomy, but of the 45 Grades III, IV or V patients, 35 underwent a primary repair with a partial orchiectomy or orchiectomy with a hematoma evacuation performed in 10.
CONCLUSIONS
Ultrasonography was found to be the most effective modality for detecting a rupture of the tunica albuginea, and the authors conclude that the AAST OIS can be used to determine the treatment modality. Our recommended treatment policy is as follows; conservative for Grade I, exploration and repair for Grade II, and exploration, and a partial orchiectomy or orchiectomy for Grades III, IV or V. In particular, an orchiectomy is the most commonly used modality for Grade V.
Keyword
MeSH Terms
Figure
Reference
-
1. Moore EE, Malangoni MA, Cogbill TH, Peterson NE, Champion HR, Jurkovich GJ, et al. Organ injury scaling VII: cervical vascular, peripheral vascular, adrenal, penis, testis, and scrotum. J Trauma. 1996. 41:523–524.2. Ficarra V, Caleffi G, Mofferdin A, Zanon G, Tallarigo C, Malossini G. Penetrating trauma to the scrotum and the corpora cavernosa caused by gunshot. Urol Int. 1999. 62:192–194.3. Cline KJ, Mata JA, Venable DD, Eastham JA. Penetrating trauma to the male external genitalia. J Trauma. 1998. 44:492–494.4. Gomez RG, Castanheira AC, McAninch JW. Gunshot wounds to the male external genitalia. J Urol. 1993. 150:1147–1149.5. Brandes SB, Buckman RF, Chelsky MJ, Hanno PM. External genitalia gunshot wounds: a ten-year experience with fifty-six cases. J Trauma. 1995. 39:266–271.6. Mohr AM, Pham AM, Lavery RF, Sifri Z, Bargman V, Livingston DH. Management of trauma to the male external genitalia: the usefulness of American Association for the Surgery of Trauma organ injury scales. J Urol. 2003. 170:2311–2315.7. Wan J, Corvino TF, Greenfield SP, DiScala C. Kidney and testicle injuries in team and individual sports: data from the national pediatric trauma registry. J Urol. 2003. 170:1528–1533.8. Gomes CM, Ribeiro-Filho L, Giron AM, Mitre AI, Figueira ER, Arap S. Genital trauma due to animal bites. J Urol. 2000. 165:80–83.9. Cummings JM, Boullier JA. Scrotal dog bites. J Urol. 2000. 164:57–58.10. Cass AS. Testicular trauma. J Urol. 1983. 129:299–300.11. Cass AS, Luxenberg M. Testicular injuries. Urology. 1991. 37:528–530.12. Micallef M, Ahmad I, Ramesh N, Hurley M, McInerney D. Ultrasound features of blunt testicular injury. Injury. 2001. 32:23–26.13. Joudi FN, Lux MM, Sandlow JI. Testicular rupture secondary to paint ball injury. J Urol. 2004. 171:797.14. Haas CA, Brown SL, Spirnak JP. Penile fracture and testicular rupture. World J Urol. 1999. 17:101–106.15. Buckley JC, McAninch JW. Use of ultrasonography for the diagnosis of testicular injuries in blunt scrotal trauma. J Urol. 2006. 175:175–178.16. Fournier GR Jr, Laing FC, Jeffrey RB, McAninch JW. High resolution scrotal ultrasonography: a highly sensitive but nonspecific diagnostic technique. J Urol. 1985. 134:490–493.17. Anderson KA, McAninch JW, Jeffrey RB, Laing FC. Ultrasonography for the diagnosis and staging of blunt scrotal trauma. J Urol. 1983. 130:933–935.18. Bree RL. Pollack HM, McClennan BL, editors. Trauma to the scrotum and scrotal contents. Clinical urography. 2002. 2nd ed. Philadelphia: Saunders;1839–1845.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multidetector CT Findings of Solid Organ Injury Based on 2018 Updated American Association for the Surgery of Trauma Organ Injury Scaling System
- Testicular Dislocation Associated with Pelvic Ring Injury
- Successful nonoperative management of a simultaneous high-grade splenic injury and devascularized kidney in Australia: a case report
- Intervention for Urologic Trauma
- Outcomes of open neck injuries