A Common Immunopathogenesis Mechanism for Infectious Diseases: The Protein-Homeostasis-System Hypothesis
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea. leekyungyil@catholic.ac.kr
- 2Department of Pediatrics, The Catholic University of Korea, Daejeon St. Mary's Hospital, Daejeon, Korea.
- KMID: 1909519
- DOI: http://doi.org/10.3947/ic.2015.47.1.12
Abstract
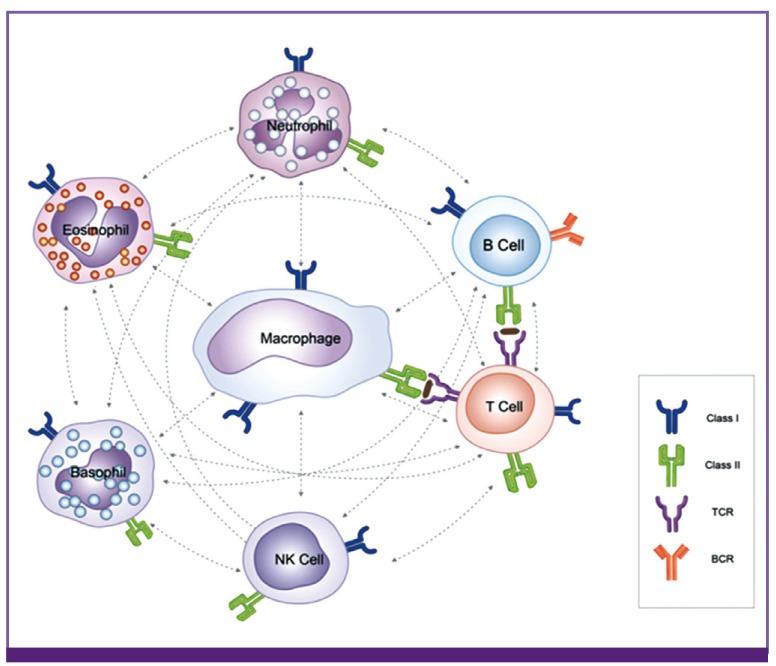
- It was once believed that host cell injury in various infectious diseases is caused solely by pathogens themselves; however, it is now known that host immune reactions to the substances from the infectious agents and/or from the injured host cells by infectious insults are also involved. All biological phenomena in living organisms, including biochemical, physiological and pathological processes, are performed by the proteins that have various sizes and shapes, which in turn are controlled by an interacting network within the living organisms. The author proposes that this network is controlled by the protein homeostasis system (PHS), and that the immune system is one part of the PHS of the host. Each immune cell in the host may recognize and respond to substances, including pathogenic proteins (PPs) that are toxic to target cells of the host, in ways that depend on the size and property of the PPs. Every infectious disease has its own set of toxic substances, including PPs, associated with disease onset, and the PPs and the corresponding immune cells may be responsible for the inflammatory processes that develop in those infectious diseases.
MeSH Terms
Figure
Cited by 4 articles
-
Severe Skin Lesions or Arthritis May be Associated with Coronary Artery Lesions in Kawasaki Disease
Song Ee Youn, Hee Young Ju, Kyung Suk Lee, Sung Ho Cha, Mi Young Han, Kyung Lim Yoon
Pediatr Infect Vaccine. 2016;23(2):102-108. doi: 10.14776/piv.2016.23.2.102.Kawasaki Disease with Influenza A Virus and
Mycoplasma pneumoniae Infections: A Case Report and Review of Literature
Hyeok Soo Moon, Jae Seong Huh, Mi Kyung Kim, Mulakwa Morisho Lambert
Pediatr Infect Vaccine. 2016;23(2):149-154. doi: 10.14776/piv.2016.23.2.149.A Case of Erythema Nodosum Associated with
Mycoplasma pneumoniae Infection: Pathologic Findings and a Presumed Pathogenesis
Hee Young Ju, Gou Young Kim, Sun Hee Choi
Pediatr Infect Vaccine. 2016;23(1):67-71. doi: 10.14776/piv.2016.23.1.67.Clinical Features of Kawasaki Disease with Pyuria
Hyo-Jin Kim, Joo-Young Lee, Ui-Yoon Choi, Soo-Young Lee
Pediatr Infect Vaccine. 2017;24(3):141-145. doi: 10.14776/piv.2017.24.3.141.
Reference
-
1. Lee KY. Pediatric respiratory infections by Mycoplasma pneumoniae. Expert Rev Anti Infect Ther. 2008; 6:509–521. PMID: 18662117.2. Youn YS, Lee KY. Mycoplasma pneumoniae pneumonia in children. Korean J Pediatr. 2012; 55:42–47. PMID: 22375148.3. Lee KY, Rhim JW, Kang JH. Hyperactive immune cells (T cells) may be responsible for acute lung injury in influenza virus infections: a need for early immune-modulators for severe cases. Med Hypotheses. 2011; 76:64–69. PMID: 20822853.
Article4. Ryu JU, Kim EK, Youn YS, Rhim JW, Lee KY. Outbreaks of mumps: an observational study over two decades in a single hospital in Korea. Korean J Pediatr. 2014; 57:396–402. PMID: 25324865.
Article5. Lee KY, Rhim JW, Kang JH. Kawasaki disease: laboratory findings and an immunopathogenesis on the premise of a "protein homeostasis system". Yonsei Med J. 2012; 53:262–275. PMID: 22318812.
Article6. Chen K, Rajewsky N. The evolution of gene regulation by transcription factors and microRNAs. Nat Rev Genet. 2007; 8:93–103. PMID: 17230196.
Article7. Jaenisch R, Bird A. Epigenetic regulation of gene expression: how the genome integrates intrinsic and environmental signals. Nat Genet. 2003; 33(Suppl):245–254. PMID: 12610534.
Article8. Sordillo PP, Helson L. Curcumin suppression of cytokine release and cytokine storm: a potential therapy for patients with Ebola and other severe viral infections. In Vivo. 2015; 29:1–4. PMID: 25600522.9. Chaithanyaa N, Devireddy SK, Kishore-Kumar RV, Gali RS, Aneja V. Sympathetic ophthalmia: a review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:172–176. PMID: 22677732.
Article10. Khan FY. Rhabdomyolysis: a review of the literature. Neth J Med. 2009; 67:272–283. PMID: 19841484.11. Bran GM, Goessler UR, Hormann K, Riedel F, Sadick H. Keloids: current concepts of pathogenesis (review). Int J Mol Med. 2009; 24:283–293. PMID: 19639219.
Article12. Narasaraju T-, Yang E, Samy RP, Ng HH, Poh WP, Liew AA, Phoon MC, van Rooijen N, Chow VT. Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am J Pathol. 2011; 179:199–210. PMID: 21703402.
Article13. Yousefi S, Simon D, Simon HU. Eosinophil extracellular DNA traps: molecular mechanisms and potential roles in disease. Curr Opin Immunol. 2012; 24:736–739. PMID: 22981682.
Article14. Johann DJ Jr, McGuigan MD, Patel AR, Tomov S, Ross S, Conrads TP, Veenstra TD, Fishman DA, Whiteley GR, Petricoin EF 3rd, Liotta LA. Clinical proteomics and biomarker discovery. Ann NY Acad Sci. 2004; 1022:295–305. PMID: 15251975.
Article15. Kurian MA, Gissen P, Smith M, Heales S Jr, Clayton PT. The monoamine neurotransmitter disorders: an expanding range of neurological syndromes. Lancet Neurol. 2011; 10:721–733. PMID: 21777827.
Article16. Fricker LD. Neuropeptide-processing enzymes: applications for drug discovery. AAPS J. 2005; 7:E449–E455. PMID: 16353923.
Article17. Vaidya A, Brown JM, Williams JS. The renin-angiotensin-aldosterone system and calcium-regulatory hormones. J Hum Hypertens. 2015; [Epub ahead of print].
Article18. Weinstein SA, Schmidt JJ, Bernheimer AW, Smith LA. Characterization and amino acid sequences of two lethal peptides isolated from venom of Wagler's pit viper, Trimeresurus wagleri. Toxicon. 1991; 29:227–236. PMID: 2048140.
Article19. Kasheverov IE, Utkin YN, Tsetlin VI. Naturally occurring and synthetic peptides acting on nicotinic acetylcholine receptors. Curr Pharm Des. 2009; 15:2430–2452. PMID: 19601841.
Article20. Hervé JC. Therapeutic potential of peptide motifs - part V. Curr Pharm Des. 2011; 17:2592–2593. PMID: 21728975.21. Gaspar D, Veiga AS, Castanho MA. From antimicrobial to anticancer peptides. A review. Front Microbiol. 2013; 4:294. PMID: 24101917.
Article22. Walsh CM, Edinger AL. The complex interplay between autophagy, apoptosis, and necrotic signals promotes T-cell homeostasis. Immunol Rev. 2010; 236:95–109. PMID: 20636811.
Article23. Levine B, Mizushima N, Virgin HW. Autophagy in immunity and inflammation. Nature. 2011; 469:323–335. PMID: 21248839.
Article24. Perrone LA, Plowden JK, García-Sastre A, Katz JM, Tumpey TM. H5N1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathog. 2008; 4:e1000115. PMID: 18670648.
Article25. Tanaka H, Honma S, Abe S, Tamura H. Effects of interleukin-2 and cyclosporin A on pathologic features in Mycoplasma pneumonia. Am J Respir Crit Care Med. 1996; 154:1908–1912. PMID: 8970385.26. Bhatt NY, Allen JN. Update on eosinophilic lung diseases. Semin Respir Crit Care Med. 2012; 33:555–571. PMID: 23001808.
Article27. Fish AJ, Herdman RC, Michael AF, Pickering RJ, Good RA. Epidemic acute glomerulonephritis associated with type 49 streptococcal pyoderma. II. Correlative study of light, immunofluorescent and electron microscopic findings. Am J Med. 1970; 48:28–39. PMID: 4906107.28. Wyatt RJ, Julian BA. IgA nephropathy. N Engl J Med. 2013; 368:2402–2414. PMID: 23782179.
Article29. Sandora TJ, Sectish TC. Pneumonia. In : Kliegman RM, Behrman RE, Staton BF, Schov NF, St.Geme JW, editors. Nelson text books of pediatrics. 19th ed. Philadelphia, PA: Saunders Elsevier;2011. p. 1474–1479.30. Downey A, Jackson C, Harun N, Cooper A. Toxic epidermal necrolysis: review of pathogenesis and management. J Am Acad Dermatol. 2012; 66:995–1003. PMID: 22169256.
Article31. Yasui S, Fujiwara K, Yonemitsu Y, Oda S, Nakano M, Yokosuka O. Clinicopathological features of severe and fulminant forms of autoimmune hepatitis. J Gastroenterol. 2011; 46:378–390. PMID: 20821236.
Article32. Poletti V, Romagnoli M, Piciucchi S, Chilosi M. Current status of idiopathic nonspecific interstitial pneumonia. Semin Respir Crit Care Med. 2012; 33:440–449. PMID: 23001799.
Article34. Lahmer T, Heemann U. Anti-glomerular basement membrane antibody disease: a rare autoimmune disorder affecting the kidney and the lung. Autoimmun Rev. 2012; 12:169–173. PMID: 22546293.
Article35. Talukdar R, Swaroop Vege S. Early management of severe acute pancreatitis. Curr Gastroenterol Rep. 2011; 13:123–130. PMID: 21243452.
Article36. Hoshino A, Saitoh M, Oka A, Okumura A, Kubota M, Saito Y, Takanashi J, Hirose S, Yamagata T, Yamanouchi H, Mizuguchi M. Epidemiology of acute encephalopathy in Japan, with emphasis on the association of viruses and syndromes. Brain Dev. 2012; 34:337–343. PMID: 21924570.
Article37. Hamilton D, Harris MD, Foweraker J, Gresham GA. Waterhouse-Friderichsen syndrome as a result of non-meningococcal infection. J Clin Pathol. 2004; 57:208–209. PMID: 14747454.
Article38. Ranjit S, Kissoon N. Dengue hemorrhagic fever and shock syndromes. Pediatr Crit Care Med. 2011; 12:90–100. PMID: 20639791.
Article39. Sinha A, Bagga A. Nephrotic syndrome. Indian J Pediatr. 2012; 79:1045–1055. PMID: 22644544.
Article40. Ramig RF. Pathogenesis of intestinal and systemic rotavirus infection. J Virol. 2004; 78:10213–10220. PMID: 15367586.
Article41. Bradford BM, Mabbott NA. Prion disease and the innate immune system. Viruses. 2012; 4:3389–3419. PMID: 23342365.
Article42. Garcia-Vidal C, Carratalà J. Early and late treatment failure in community-acquired pneumonia. Semin Respir Crit Care Med. 2009; 30:154–160. PMID: 19296415.
Article43. Benninger F, Steiner I. Steroids in bacterial meningitis: yes. J Neural Transm. 2013; 120:339–342. PMID: 23238974.
Article44. Kim DH, Lee KY, Kim MS, Youn YS, Hwang JY, Rhim JW, Kang JH, Lee JS. Corticosteroid treatment in siblings affected with severe Mycoplasma pneumoniae pneumonia. Infect Chemother. 2009; 41:190–195.45. Jefferson T, Doshi P. Multisystem failure: the story of anti-influenza drugs. BMJ. 2014; 348:g2263. PMID: 24721793.
Article46. Rhim JW, Lee KY, Youn YS, Kang JH, Kim JC. Epidemiological and clinical characteristics of childhood pandemic 2009 H1N1 virus infection: an observational cohort study. BMC Infect Dis. 2011; 11:225. PMID: 21864391.
Article47. Lee KY, Lee HS, Hong JH, Lee MH, Lee JS, Burgner D, Lee BC. Role of prednisolone treatment in severe Mycoplasma pneumoniae pneumonia in children. Pediatr Pulmonol. 2006; 41:263–268. PMID: 16437541.48. Youn YS, Lee SC, Rhim JW, Shin MS, Kang JH, Lee KY. Early additional immune-modulators for Mycoplasma pneumoniae pneumonia in children: an observation study. Infect Chemother. 2014; 46:239–247. PMID: 25566403.49. Kil HR, Lee JH, Lee KY, Rhim JW, Youn YS, Kang JH. Early corticoid treatment for severe pneumonia caused by 2009 H1N1 influenza virus. Crit Care. 2011; 15:413. PMID: 21457512.50. Annane D. Pro: the illegitimate crusade against corticosteroids for severe H1N1 pneumonia. Am J Respir Crit Care Med. 2011; 183:1125–1126. PMID: 21531952.
Article51. McGee S, Hirschmann J. Use of corticosteroids in treating infectious diseases. Arch Intern Med. 2008; 168:1034–1046. PMID: 18504331.
Article52. Baschant U, Tuckermann J. The role of the glucocorticoid receptor in inflammation and immunity. J Steroid Biochem Mol Biol. 2010; 120:69–75. PMID: 20346397.
Article53. Hutchinson CB, Wang E. Kikuchi-Fujimoto disease. Arch Pathol Lab Med. 2010; 134:289–293. PMID: 20121621.
Article54. Lee KY, Yeon YH, Lee BC. Kikuchi-Fujimoto disease with prolonged fever in children. Pediatrics. 2004; 114:e752–e756. PMID: 15545615.
Article55. Denny FW, Taylor-Robinson D, Allison AC. The role of thymus-dependent immunity in Mycoplasma pulmonis infections of mice. J Med Microbiol. 1972; 5:327–336. PMID: 4560750.56. Wyde PR, Couch RB, Mackler BF, Cate TR, Levy BM. Effects of low- and high-passage influenza virus infection in normal and nude mice. Infect Immun. 1997; 15:221–229. PMID: 832899.
Article57. Crowe CR, Chen K, Pociask DA, Alcorn JF, Krivich C, Enelow RI, Ross TM, Witztum JL, Kolls JK. Critical role of IL-17RA in immunopathology of influenza infection. J Immunol. 2009; 183:5301–5310. PMID: 19783685.
Article58. Rodríguez-Iturbe B, Batsford S. Pathogenesis of poststreptococcal glomerulonephritis a century after Clemens von Pirquet. Kidney Int. 2007; 71:1094–1104. PMID: 17342179.
Article59. Cunningham MW. Streptococcus and rheumatic fever. Curr Opin Rheumatol. 2012; 24:408–416. PMID: 22617826.
Article60. Imboden JB. The immunopathogenesis of rheumatoid arthritis. Annu Rev Pathol. 2009; 4:417–434. PMID: 18954286.
Article62. Hirano M, Das S, Guo P, Cooper MD. The evolution of adaptive immunity in vertebrates. Adv Immunol. 2011; 109:125–157. PMID: 21569914.
Article63. Steinman RM. Decisions about dendritic cells: past, present, and future. Annu Rev Immunol. 2012; 30:1–22. PMID: 22136168.
Article64. Auffray C, Sieweke MH, Geissmann F. Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annu Rev Immunol. 2009; 27:669–692. PMID: 19132917.
Article65. Hozumi N, Tonegawa S. Evidence for somatic rearrangement of immunoglobulin genes coding for variable and constant regions. Proc Natl Acad Sci USA. 1976; 73:3628–3632. PMID: 824647.
Article66. Tonegawa S. Somatic generation of immune diversity. Biosci Rep. 1988; 8:3–26. PMID: 3134960.
Article67. Rekvig OP, Putterman C, Casu C, Gao HX, Ghirardello A, Mortensen ES, Tincani A, Doria A. Autoantibodies in lupus: culprits or passive bystanders? Autoimmun Rev. 2011; 11:596–603. PMID: 22041579.
Article68. Gut JP, Spiess C, Schmitt S, Kirn A. Rapid diagnosis of acute mumps infection by a direct immunoglobulin M antibody capture enzyme immunoassay with labeled antigen. J Clin Microbiol. 1985; 21:346–352. PMID: 3884652.
Article69. Krause CH, Molyneaux PJ, Ho-Yen DO, McIntyre P, Carman WF, Templeton KE. Comparison of mumps-IgM ELISAs in acute infection. J Clin Virol. 2007; 38:153–156. PMID: 17142100.
Article70. Barskey AE, Schulte C, Rosen JB, Handschur EF, Rausch-Phung E, Doll MK, Cummings KP, Alleyne EO, High P, Lawler J, Apostolou A, Blog D, Zimmerman CM, Montana B, Harpaz R, Hickman CJ, Rota PA, Rota JS, Bellini WJ, Gallagher KM. Mumps outbreak in Orthodox Jewish communities in the United States. N Engl J Med. 2012; 367:1704–1713. PMID: 23113481.
Article71. Rota JS, Turner JC, Yost-Daljev MK, Freeman M, Toney DM, Meisel E, Williams N, Sowers SB, Lowe L, Rota PA, Nicolai LA, Peake L, Bellini WJ. Investigation of a mumps outbreak among university students with two measles-mumps-rubella (MMR) vaccinations, Virginia, September-December 2006. J Med Virol. 2009; 81:1819–1825. PMID: 19697404.
Article72. Lee KY, Lee HS, Hur JK, Kang JH, Lee BC. The changing epidemiology of hospitalized pediatric patients in three measles outbreaks. J Infect. 2007; 54:167–172. PMID: 16620998.
Article73. Chaves SS, Gargiullo P, Zhang JX, Civen R, Guris D, Mascola L, Seward JF. Loss of vaccine-induced immunity to varicella over time. N Engl J Med. 2007; 356:1121–1129. PMID: 17360990.
Article74. Dudareva S, Schweiger B, Thamm M, Höhle M, Stark K, Krause G, Buda S, Haas W. Prevalence of antibodies to 2009 pandemic Influenza A (H1N1) virus in German adult population in pre- and post-pandemic period. PLoS One. 2011; 6:e21340. PMID: 21701598.
Article75. Rhim JW, Go EJ, Lee KY, Youn YS, Kim MS, Park SH, Kim JC, Kang JH. Pandemic 2009 H1N1 virus infection in children and adults: A cohort study at a single hospital throughout the epidemic. Int Arch Med. 2012; 5:13. PMID: 22443897.
Article76. Schwartz-Albiez R, Monteiro RC, Rodriguez M, Binder CJ, Shoenfeld Y. Natural antibodies, intravenous immunoglobulin and their role in autoimmunity, cancer and inflammation. Clin Exp Immunol. 2009; 158(Suppl 1):43–50. PMID: 19883423.
Article77. Panda S, Ding JL. Natural antibodies bridge innate and adaptive immunity. J Immunol. 2015; 194:13–20. PMID: 25527792.
Article78. Lee KY, Han JW, Lee JS, Whang KT. Alteration of biochemical profiles after high-dose intravenous immunoglobulin administration in Kawasaki disease. Acta Paediatr. 2002; 91:164–167. PMID: 11952003.
Article79. Lee KY, Lee HS, Hong JH, Han JW, Lee JS, Whang KT. High-dose intravenous immunoglobulin downregulates the activated levels of inflammatory indices except erythrocyte sedimentation rate in acute stage of Kawasaki Disease. J Trop Pediatr. 2005; 51:98–101. PMID: 15677370.
Article80. Han JW, Lee KY, Hwang JY, Koh DK, Lee JS. Antibody status in children with steroid-sensitive nephrotic syndrome. Yonsei Med J. 2010; 51:239–243. PMID: 20191016.
Article81. Lee KY, Lee JS. Immunoglobulin G has a role for systemic protein modulation in vivo: a new concept of protein homeostasis. Med Hypotheses. 2006; 67:848–855. PMID: 16759810.82. Trowsdale J. The MHC, disease and selection. Immunol Lett. 2011; 137:1–8. PMID: 21262263.
Article83. Zinkernagel RM, Doherty PC. The discovery of MHC restriction. Immunol Today. 1997; 18:14–17. PMID: 9018968.
Article84. Tsan MF, Gao B. Heat shock proteins and immune system. J Leukoc Biol. 2009; 85:905–910. PMID: 19276179.
Article85. Li Z, Menoret A, Srivastava P. Roles of heat-shock proteins in antigen presentation and cross-presentation. Curr Opin Immunol. 2002; 14:45–51. PMID: 11790532.
Article86. Gimferrer I, Arias MT, Suárez B, Martorell J, Vives J, Lozano F. Discrepancies between serology- and sequence-based typing of HLA class I alleles among unrelated donor/recipient pairs. Transplant Proc. 1999; 31:2579–2580. PMID: 10500726.
Article87. Matzinger P. The danger model: a renewed sense of self. Science. 2002; 296:301–305. PMID: 11951032.
Article88. Kawai T, Akira S. Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity. 2011; 34:637–650. PMID: 21616434.
Article89. Kumar S, Ingle H, Prasad DV, Kumar H. Recognition of bacterial infection by innate immune sensors. Crit Rev Microbiol. 2013; 39:229–246. PMID: 22866947.
Article90. Weitz IC. Complement the hemostatic system: an intimate relationship. Thromb Res. 2014; 133(Suppl 2):S117–S121. PMID: 24862131.
Article91. Ochs HD, Hitzig WH. History of primary immunodeficiency diseases. Curr Opin Allergy Clin Immunol. 2012; 12:577–587. PMID: 23095909.
Article92. Liston A, Enders A, Siggs OM. Unraveling the association of partial T-cell immunodeficiency and immune dysregulation. Nat Rev Immunol. 2008; 8:545–558. PMID: 18551129.93. Fraser JD, Proft T. The bacterial superantigen and superantigen-like proteins. Immunol Rev. 2008; 225:226–243. PMID: 18837785.
Article94. Stach CS, Herrera A, Schlievert PM. Staphylococcal superantigens interact with multiple host receptors to cause serious diseases. Immunol Res. 2014; 59:177–181. PMID: 24838262.
Article95. Dolff S, Bijl M, Huitema MG, Limburg PC, Kallenberg CG, Abdulahad WH. Disturbed Th1, Th2, Th17 and T(reg) balance in patients with systemic lupus erythematosus. Clin Immunol. 2011; 141:197–204. PMID: 21920821.
Article96. Allen JE, Maizels RM. Diversity and dialogue in immunity to helminths. Nat Rev Immunol. 2011; 11:375–388. PMID: 21610741.
Article97. Mucida D, Cheroutre H. The many face-lifts of CD4 T helper cells. Adv Immunol. 2010; 107:139–152. PMID: 21034973.
Article98. Macleod AS, Havran WL. Functions of skin-resident γδ T cells. Cell Mol Life Sci. 2011; 68:2399–2408. PMID: 21560071.
Article